Abstract
Objective
This study reviewed and analyzed the prenatal diagnosis experience of thalassemia in our center over the past decade and the abnormal ultrasonic characteristics of fetuses with hemoglobin (Hb) Bart’s hydrops fetalis.
Methods
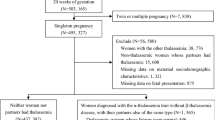
Pregnant women and their partners who tested positive for α0-thalassemia or were diagnosed with thalassemia intermedia (HbH diseases) underwent genetic counseling, and a prenatal diagnostic procedure for α-thalassemia was recommended. Ultrasonography was performed before prenatal diagnosis.
Results
Invasive prenatal α-thalassemia diagnosis and ultrasonography were performed in 1049 patients at risk for Hb Bart’s hydrops fetalis syndrome at our hospital from 2012 to 2021. Chorionic villus sampling (CVS) was performed in 58 cases (5.5%), amniocentesis in 902 cases (86%), and cordocentesis in 89 cases (8.5%). Hb Bart’s hydrops fetalis syndrome was diagnosed in 280 fetuses. The most common body cavity effusion was pericardial effusion, ascites, and fetal systemic edema.
Conclusions
The extensive experience at our center shows that carrier screening, molecular diagnostics, genetic counseling, and prenatal diagnosis are effective measures to prevent Hb Bart’s hydrops fetalis syndrome. The ultrasonographic abnormalities in fetuses with Hb Bart’s hydrops are mainly caused by an increase in cardiac output, which leads to the body cavity effusion from various organs.


Similar content being viewed by others
Data availability
All data in this article is available through personal communication with the the corresponding author.
References
Higgs DR, Vickers MA, Wilkie AO, Pretorius IM, Jarman AP, Weatherall DJ. A review of the molecular genetics of the human alpha-globin gene cluster. Blood. 1989;73(5):1081–104.
Iarovaia OV, Ulianov SV, Ioudinkova ES, Razin SV. Segregation of α- and β-Globin Gene Cluster in Vertebrate Evolution: Chance or Necessity? Biochemistry (Mosc). 2022;87(9):1035–49.
Weatherall DJ, Clegg JB. Inherited haemoglobin disorders: an increasing global health problem. Bull World Health Organ. 2001;79(8):704–12.
Muncie HL Jr, Campbell J. Alpha and beta thalassemia. Am Fam Physician. 2009;80(4):339–44.
Li D, Liao C, Li J, Xie X, Huang Y, Zhong H. Detection of alpha-thalassemia in beta-thalassemia carriers and prevention of Hb Bart’s hydrops fetalis through prenatal screening. Haematologica. 2006;91(5):649–51.
King AJ, Higgs DR. Potential new approaches to the management of the Hb Bart’s hydrops fetalis syndrome: the most severe form of α-thalassemia. Hematology Am Soc Hematol Educ Program. 2018;2018(1):353–60.
Chui DH, Waye JS. Hydrops fetalis caused by alpha-thalassemia: an emerging health care problem. Blood. 1998;91(7):2213–22.
Chong SC, Metassan S, Yusof N, et al. Thalassemia in Asia 2021 Thalassemia in Brunei Darussalam. Hemoglobin. 2022;46(1):15–9. https://doi.org/10.1080/03630269.2021.2008959.
Xu XM, Zhou YQ, Luo GX, et al. The prevalence and spectrum of alpha and beta thalassaemia in Guangdong Province: implications for the future health burden and population screening. J Clin Pathol. 2004;57(5):517–22.
Liao C, Pan M, Han J, et al. Prenatal control of Hb Bart’s hydrops fetalis: a two-year experience at a mainland Chinese hospital. J Matern Fetal Neonatal Med. 2015;28(4):413–5.
Liao C, Wei J, Li Q, Li J, Li L, Li D. Nonimmune hydrops fetalis diagnosed during the second half of pregnancy in Southern China. Fetal Diagn Ther. 2007;22(4):302–5.
Lai K, Li S, Lin W, et al. Invasive prenatal diagnosis of α-thalassemia to control Hb Bart’s hydrops fetalis syndrome: 15 years of experience. Arch Gynecol Obstet. 2018;298(2):307–11.
Weatherall DJ. Pathophysiology of thalassaemia. Baillieres Clin Haematol. 1998;11(1):127–46.
Jatavan P, Chattipakorn N, Tongsong T. Fetal hemoglobin Bart’s hydrops fetalis: pathophysiology, prenatal diagnosis and possibility of intrauterine treatment. J Matern Fetal Neonatal Med. 2018;31(7):946–57.
Chankhunaphas W, Tongsong T, Tongprasert F, et al. Comparison of the performances of middle cerebral artery peak systolic velocity and cardiothoracic diameter ratio in predicting fetal anemia: using fetal hemoglobin Bart’s disease as a study model. Fetal Diagn Ther. 2021;48(10):738–45.
Thammavong K, Luewan S, Tongsong T. Performance of fetal cardiac volume derived from VOCAL (Virtual Organ Computer-Aided AnaLysis) in predicting hemoglobin (Hb) Bart’s disease. J Clin Med. 2021;10(20):4651.
Funding
This study was supported by a research grant from the Zhongshan Science and Technology Bureau (Nos. 2020B1057, 2021B1084, 2021B3003, and 2022B1022).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Li, H., Wang, J., Wang, D. et al. Ten years’ experience in prenatal diagnosis of α-thalassemia in a municipal hospital and retrospective analysis of ultrasonic abnormalities. Int J Hematol 118, 355–363 (2023). https://doi.org/10.1007/s12185-023-03643-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-023-03643-6