Abstract
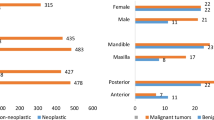
Gingival growths, barring a few are mostly reactive and seldom exhibit significant true neoplastic potential. The common etiology is local irritation from dental plaque/calculus, trauma as well as medication-related overgrowth. Such lesions are easily distinguishable and categorized into diagnoses such as pyogenic granuloma, peripheral ossifying fibroma, etc. We present a previously undescribed, but commonly encountered, reactive gingival growth with unique histologic features and suggest the diagnostic term “gingival fibroma.” An IRB approved retrospective review of the University of Florida Oral Pathology Biopsy Service encompassing years 2010–2019, was performed to select cases. Demographics, clinical data, and microscopic diagnoses were recorded and analyzed. Four board-certified oral and maxillofacial pathologists agreed upon and established the diagnostic criteria. These are: a prominent fibromyxoid stroma, variable cellularity, a whorled or storiform pattern of arrangement of the cellular elements, lack of significant inflammation or vascularity, and complete absence of calcification, and/or odontogenic islands. A total of 60 cases met all criteria and were included in the study. Age range in years was 14–87 with the mean at 45.11 years. A striking female predilection (90%) was noted. Approximately 62% of cases were reported on the maxillary gingiva, followed by 38.3% in the mandibular gingiva. Majority, 66.7% were in the anterior incisor region followed by 11.7% in the canine/first premolar areas. All lesions were submitted as excisional biopsy, and 4 cases recurred within 2–3 years of excision. In all cases, lesional tissue appeared to extend to the surgical base of the specimen. We present 60 cases of a histologically unique entity occurring exclusively on the gingiva and introduce the diagnostic term “Gingival Fibroma” for these lesions. Further studies with adequate clinical follow-up may help understand the exact clinical behavior of these lesions.


Similar content being viewed by others
References
Hunasgi S, Koneru A, Vanishree M, Manvikar V. Assessment of reactive gingival lesions of oral cavity: a histopathological study. J Oral Maxillofac Pathol. 2017;21(1):180. https://doi.org/10.4103/jomfp.JOMFP_23_16.
Park SH, Lee JH, Tak MS, Lee HJ, Choi HJ. A research of pyogenic granuloma genesis factor with immunohistochemical analysis. J Craniofac Surg. 2017;28(8):2068–72. https://doi.org/10.1097/SCS.0000000000004148.
Sharma S, Chandra S, Gupta S, Srivastava S. Heterogeneous conceptualization of etiopathogenesis: oral pyogenic granuloma. Natl J Maxillofac Surg. 2019;10(1):3–7. https://doi.org/10.4103/njms.NJMS_55_18.
Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci. 2006;48(4):167–75.
Fujiwara C, Motegi SI, Sekiguchi A, Amano H, Ishikawa O. Pyogenic granuloma possibly associated with capecitabine therapy. J Dermatol. 2017;44(11):1329–31. https://doi.org/10.1111/1346-8138.13691.
Inoue A, Sawada Y, Nishio D, Nakamura M. Pyogenic granuloma caused by afatinib: case report and review of the literature. Australas J Dermatol. 2017;58(1):61–2. https://doi.org/10.1111/ajd.12423.
Neville BW, Damm DD, Allen CM, Chi AC. Oral & maxillofacial pathology. 4th ed. St. Louis, MO: Elsevier; 2016.
Mortazavi H, Safi Y, Baharvand M, Rahmani S, Jafari S. Peripheral exophytic oral lesions: a clinical decision tree. Int J Dent. 2017;2017:9193831. https://doi.org/10.1155/2017/9193831.
Mergoni G, Meleti M, Magnolo S, Giovannacci I, Corcione L, Vescovi P. Peripheral ossifying fibroma: a clinicopathologic study of 27 cases and review of the literature with emphasis on histomorphologic features. J Indian Soc Periodontol. 2015;19:83–7.
Effiom OA, Adeyemo WL, Soyele OO. Focal reactive lesions of the gingiva: an analysis of 314 cases at a tertiary health institution in Nigeria. Niger Med J. 2011;52(1):35–40.
Lázare H, Peteiro A, Pérez Sayáns M, Gándara-Vila P, Caneiro J, García-García A, et al. Clinicopathological features of peripheral ossifying fibroma in a series of 41 patients. Br J Oral Maxillofac Surg. 2019;57(10):1081–5. https://doi.org/10.1016/j.bjoms.2019.09.020.
Regezi JA, Sciubba JJ, Jordan RCK. Oral pathology clinical pathologic correlations. 5th ed. St. Louis, MO: Saunders/Elsevier; 2008.
Ritwik P, Brannon RB. Peripheral odontogenic fibroma: a clinicopathologic study of 151 cases and review of the literature with special emphasis on recurrence. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(3):357–63. https://doi.org/10.1016/j.tripleo.2010.04.018.
Brierley DJ, Crane H, Hunter KD. Lumps and bumps of the gingiva: a pathological miscellany. Head Neck Pathol. 2019;13(1):103–13. https://doi.org/10.1007/s12105-019-01000-w.
Manabe K, Yakeishi M, Sakaguchi W, Saruta J, Tsukinoki K. Histopathological analysis of the differential diagnosis of peripheral odontogenic fibroma from fibrous epulis. J Oral Biosci. 2019;61(4):221–5. https://doi.org/10.1016/j.job.2019.10.003.
Solomon M. The histological spectrum of myxoma, myxofibroma/fibromyxoma and odontogenic fibroma—“a chicken and egg situation.” IOSR J Dent Med Sci. 2012;1(1):03–5. https://doi.org/10.9790/0853-0120305.
Bodner L, Peist M, Gatot A, Fliss DM. Growth potential of peripheral giant cell granuloma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83(5):548–51.
Lester SR, Cordell KG, Rosebush MS, Palaiologou AA, Maney P. Peripheral giant cell granulomas: a series of 279 cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118(4):475–82. https://doi.org/10.1016/j.oooo.2014.06.004.
Chrcanovic BR, Gomes CC, Gomez RS. Peripheral giant cell granuloma: an updated analysis of 2824 cases reported in the literature. J Oral Pathol Med. 2018;47(5):454–9. https://doi.org/10.1111/jop.12706.
Funding
No financial support was provided for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Ethical Committee: Health Center Institutional Review Board of University of Florida.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bawazir, M., Islam, M.N., Cohen, D.M. et al. Gingival Fibroma: An Emerging Distinct Gingival Lesion with Well-Defined Histopathology. Head and Neck Pathol 15, 917–922 (2021). https://doi.org/10.1007/s12105-021-01315-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-021-01315-7