Abstract
Purpose
This study aimed at analyzing and comparing the perioperative results and long-term oncological outcomes of hepatocellular carcinoma (HCC) patients with type 2 diabetes mellitus (T2DM) treated with laparoscopic (LLR) versus open liver resection (OLR).
Methods
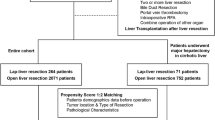
Clinicopathological data of HCC patients with T2DM who underwent LLR or OLR as initial treatment from four medical centers were retrospectively reviewed. The survival outcomes of patients who underwent laparoscopic liver resection (LLR) were compared with those of patients who underwent open liver resection (OLR). Using the Kaplan–Meier method, survival curves for the two groups of patients were generated, and the log-rank test was used to compare survival differences. Propensity score matching (PSM) analysis was used to match patients of the LLR and OLR groups in a 1:1 ratio.
Results
230 HCC patients with T2DM were enrolled, including 101 patients in the LLR group and 129 patients in the OLR group. After PSM, 90 patients were matched in each of the study group. Compared with the OLR group, the LLR group had less blood loss, a shorter hospitalization and fewer postoperative complications. The LLR group had a significantly better overall survival (OS) and recurrence-free survival (RFS) than the OLR group before and after PSM. Subgroup analysis demonstrated that HCC patients with T2DM had survival benefits from LLR regardless of the course of T2DM.
Conclusions
Laparoscopic liver resection for HCC patients with T2DM can be safely performed with favorable perioperative and long-term oncological outcomes at high-volume liver cancer centers, regardless of the course of T2DM.




Similar content being viewed by others
References
Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94(2):153–156
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132(7):2557–2576
Han HS, Shehta A, Ahn S, Yoon YS, Cho JY, Choi Y. Laparoscopic versus open liver resection for hepatocellular carcinoma: case-matched study with propensity score matching. J Hepatol. 2015;63(3):643–650
Coelho FF, Kruger JA, Fonseca GM, Araújo RL, Jeismann VB, Perini MV, et al. Laparoscopic liver resection: experience based guidelines. World J Gastrointest Surg. 2016;8(1):5–26
Vogel A, Cervantes A, Chau I, Daniele B, Llovet JM, Meyer T, et al. Hepatocellular carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30(5):871–873
Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991;78(5 Pt 2):956–958
Yoshida H, Taniai N, Yoshioka M, Hirakata A, Kawano Y, Shimizu T, et al. Current status of laparoscopic hepatectomy. J Nippon Med School = Nippon Ika Daigaku zasshi. 2019;86(4):201–206
Topal B, Fieuws S, Aerts R, Vandeweyer H, Penninckx F. Laparoscopic versus open liver resection of hepatic neoplasms: comparative analysis of short-term results. Surg Endosc. 2008;22(10):2208–2213
Belli G, Limongelli P, Fantini C, D’Agostino A, Cioffi L, Belli A, et al. Laparoscopic and open treatment of hepatocellular carcinoma in patients with cirrhosis. Br J Surg. 2009;96(9):1041–1048
Castaing D, Vibert E, Ricca L, Azoulay D, Adam R, Gayet B. Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg. 2009;250(5):849–855
Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2804 patients. Ann Surg. 2009;250(5):831–841
Croome KP, Yamashita MH. Laparoscopic vs open hepatic resection for benign and malignant tumors: an updated meta-analysis. Arch surg. 2010;145(11):1109–1118
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: the Louisville statement, 2008. Ann Surg. 2009;250(5):825–830
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261(4):619–629
Yin Z, Fan X, Ye H, Yin D, Wang J. Short- and long-term outcomes after laparoscopic and open hepatectomy for hepatocellular carcinoma: a global systematic review and meta-analysis. Ann Surg Oncol. 2013;20(4):1203–1215
Goh EL, Chidambaram S, Ma S. Laparoscopic vs open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a meta-analysis of the long-term survival outcomes. Int J Surg (London, England). 2018;50:35–42
Jiang S, Wang Z, Ou M, Pang Q, Fan D, Cui P. Laparoscopic versus open hepatectomy in short- and long-term outcomes of the hepatocellular carcinoma patients with cirrhosis: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A. 2019;29(5):643–654
Xiangfei M, Yinzhe X, Yingwei P, Shichun L, Weidong D. Open versus laparoscopic hepatic resection for hepatocellular carcinoma: a systematic review and meta-analysis. Surg Endosc. 2019;33(8):2396–2418
DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers. 2015;23(1):15019
Schlesinger S, Aleksandrova K, Pischon T, Jenab M, Fedirko V, Trepo E, et al. Diabetes mellitus, insulin treatment, diabetes duration, and risk of biliary tract cancer and hepatocellular carcinoma in a European cohort. Ann Oncol. 2013;24(9):2449–2455
Yang WS, Shu XO, Gao J, Li HL, Cai H, Yang G, et al. Prospective evaluation of type 2 diabetes mellitus on the risk of primary liver cancer in Chinese men and women. Ann Oncol. 2013;24(6):1679–1685
Kawamura Y, Ikeda K, Arase Y, Yatsuji H, Sezaki H, Hosaka T, et al. Diabetes mellitus worsens the recurrence rate after potentially curative therapy in patients with hepatocellular carcinoma associated with nonviral hepatitis. J Gastroenterol Hepatol. 2008;23(11):1739–1746
Wang WM, Xu Y, Yang XR, Wang YH, Sun HX, Fan J. Prognostic role of diabetes mellitus in hepatocellular carcinoma patients after curative treatments: a meta-analysis. Hepatobiliary Pancreat Dis Int. 2011;10(4):346–355
Martin ET, Kaye KS, Knott C, Nguyen H, Santarossa M, Evans R, et al. Diabetes and risk of surgical site infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2016;37(1):88–99
Luo J, Xu L, Li L, Zhang J, Zhang M, Xu M. Diabetes mellitus and postoperative blood glucose value help predict posthepatectomy liver failure in patients with hepatocellular carcinoma. J Gastrointest Oncol. 2021;12(5):2377–2387
Shen GL, Lu Y, Liang L, Lu WF, Diao YK, Xiao ZQ, et al. Impact of diabetes mellitus on the long-term prognosis of patients with hepatocellular carcinoma after hepatectomy. Expert Rev Gastroenterol Hepatol. 2022;15:1–6
Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American association for the study of liver diseases. Hepatology (Baltimore, MD). 2018;68(2):723–750
Reig M, Forner A, Rimola J, Ferrer-Fàbrega J, Burrel M, Garcia-Criado Á, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 2022;76(3):681–693
Roayaie S, Blume IN, Thung SN, Guido M, Fiel MI, Hiotis S, et al. A system of classifying microvascular invasion to predict outcome after resection in patients with hepatocellular carcinoma. Gastroenterology. 2009;137(3):850–855
Lim KC, Chow PK, Allen JC, Chia GS, Lim M, Cheow PC, et al. Microvascular invasion is a better predictor of tumor recurrence and overall survival following surgical resection for hepatocellular carcinoma compared to the Milan criteria. Ann Surg. 2011;254(1):108–113
Classification and Diagnosis of Diabetes. Standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17-s38
Yoshida N, Takayama T, Midorikawa Y, Higaki T, Nakayama H, Moriguchi M, et al. Surgical outcomes in patients with hepatocellular carcinoma associated with metabolic syndrome. World J Surg. 2015;39(2):471–477
Liu YW, Yen YH, Li WF, Wang CC, Lu SN, Kee KM, et al. Minimally invasive surgery versus percutaneous radiofrequency ablation for early-stage hepatocellular carcinoma: results from a high-volume liver surgery center in East Asia. Surg Oncol. 2022;19(42): 101769
Aoki T, Kubota K, Hasegawa K, Kubo S, Izumi N, Kokudo N, et al. Significance of the surgical hepatic resection margin in patients with a single hepatocellular carcinoma. Br J Surg. 2020;107(1):113–120
Nitta H, Allard MA, Sebagh M, Golse N, Ciacio O, Pittau G, et al. Ideal surgical margin to prevent early recurrence after hepatic resection for hepatocellular carcinoma. World J Surg. 2021;45(4):1159–1167
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213
EASL Clinical Practice Guidelines. Management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236
Vogel A, Cervantes A, Chau I, Daniele B, Llovet JM, Meyer T, et al. Hepatocellular carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Suppl 4):iv238–iv255
Li T, Fan J, Qin LX, Zhou J, Sun HC, Qiu SJ, et al. Risk factors, prognosis, and management of early and late intrahepatic recurrence after resection of primary clear cell carcinoma of the liver. Ann Surg Oncol. 2011;18(7):1955–1963
Kabir T, Tan ZZ, Syn NL, Wu E, Lin JD, Zhao JJ, et al. Laparoscopic versus open resection of hepatocellular carcinoma in patients with cirrhosis: meta-analysis. Br J Surg. 2021;109(1):21–29
Abu Hilal M, Aldrighetti L, Dagher I, Edwin B, Troisi RI, Alikhanov R, et al. The southampton consensus guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg. 2018;268(1):11–18
Cheung TT, Han HS, She WH, Chen KH, Chow PKH, Yoong BK, et al. The Asia Pacific consensus statement on laparoscopic liver resection for hepatocellular carcinoma: a report from the 7th Asia-Pacific primary liver cancer expert meeting held in Hong Kong. Liver cancer. 2018;7(1):28–39
Coletta D, De Padua C, Parrino C, De Peppo V, Oddi A, Frigieri C, et al. Laparoscopic liver surgery: what are the advantages in patients with cirrhosis and portal hypertension? Systematic review and meta-analysis with personal experience. J Laparoendosc Adv Surg Tech A. 2020;30(10):1054–1065
Pennel L, Quesada JL, Dematteis M. Neuroticism and anxious attachment as potential vulnerability factors of repeat suicide attempts. Psychiatry Res. 2018;264:46–53
Yang SY, Yan ML, Duan YF, Feng JK, Ye JZ, Xiang YJ, et al. Perioperative and long-term survival outcomes of laparoscopic versus laparotomic hepatectomy for BCLC stages 0-A hepatocellular carcinoma patients associated with or without microvascular invasion: a multicenter, propensity score matching analysis. Hep Intl. 2022;16(4):892–905
Funding
Meng Chao Talent Training Program (EHBH2019YC112); the Clinical Research Plan of Shanghai Hospital Development Center (SHDC2020CR1004A); the State Key Program of National Natural Science Foundation of China (81730097); National Natural Science Foundation of China (82172846; 82072618).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
The study was approved by the Clinical Research Ethics Committees of each center and was in line with the 2013 Helsinki Declaration.
Informed consent
Written informed consent was obtained from all patients prior to enrollment for this study.
Conflict of interest
Shi-Ye Yang, Jin-Kai Feng, Mao-Lin Yan, Lei Guo, Yun-Fei Duan, Jia-Zhou Ye, Zong-Han Liu, Yan-Jun Xiang, Li Xu, Jie Xue, Jie Shi, Wan Yee Lau, Shu-Qun Cheng, Wei-Xing Guo who participate in this study have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12072_2023_10492_MOESM1_ESM.tif
Supplementary file1 Overall survival (OS) and recurrence-free survival (RFS) of non-cirrhotic HCC patients with T2DM treated with LLR or OLR before and after PSM. OS (A) and RFS (B) of non-cirrhotic HCC patients with T2DM before PSM. OS (C) and RFS (D) of non-cirrhotic HCC patients with T2DM after PSM. Abbreviations: HCC, hepatocellular carcinoma; LLR, laparoscopic liver resection; OLR, open liver resection; PSM, propensity score matching (TIF 1703 KB)
12072_2023_10492_MOESM2_ESM.tif
Supplementary file2 Overall survival (OS) and recurrence-free survival (RFS) of cirrhotic HCC patients with T2DM treated with LLR or OLR before and after PSM. OS (A) and RFS (B) of cirrhotic HCC patients with T2DM before PSM. OS (C) and RFS (D) of cirrhotic HCC patients with T2DM after PSM. Abbreviations: HCC, hepatocellular carcinoma; LLR, laparoscopic liver resection; OLR, open liver resection; PSM, propensity score matching (TIF 1682 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, SY., Feng, JK., Yan, ML. et al. Laparoscopic and open liver resection for hepatocellular carcinoma with type 2 diabetes mellitus: multicenter propensity score-matched study. Hepatol Int 17, 1251–1264 (2023). https://doi.org/10.1007/s12072-023-10492-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-023-10492-2