Abstract
Background
Metabolic associated fatty liver disease (MAFLD) is the most common chronic liver disease worldwide. The important role of urid acid (UA) in MAFLD has been widely investigated. Our previous studies unveiled the elevation of serum UA levels independently predicts an increased risk of incident MAFLD. However, the role of intrahepatic UA in MAFLD has not been investigated yet. Glucose transporter 9 (GLUT9) is a key transporter that mediates the uptake of UA in hepatocytes.
Methods
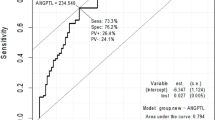
In this study, we first explored the clinical association between GLUT9 polymorphism and MAFLD. Blood samples of 247 male Chinese (127 were MAFLD patients) were collected and tested for the blood UA levels and genotype of the single nucleotide polymorphism (SNP) of GLUT9 (rs1014290). Next, Glut9 hepatic-specific knockout mice (Glut9Hep−ko) were generated to investigate the role of hepatic GLUT9 in MAFLD in male mice.
Results
We found that the GA/AA genotypes (rs1014290) were associated with elevated serum UA levels in MAFLD patients. Meanwhile, we found that Glut9Hep−ko mice displayed lower intrahepatic UA levels, down-regulated lipogenesis genes expressions, and attenuated MAFLD symptoms after 12 weeks of high-fat diet feeding, compared with Glut9Fl/Fl littermates. However, Glut9Hep−ko mice and wild-type littermates showed no significant difference on hepatic fatty acid oxidation or inflammation.
Conclusions
Our results suggested that GLUT9 polymorphism was significantly associated with MAFLD, and hepatic-specific knockout of Glut9 significantly decreased intrahepatic contents and ameliorated diet-induced MAFLD in mice.




Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this article.
Abbreviations
- MAFLD:
-
Metabolic-associated fatty liver disease
- GLUT9:
-
Glucose transporter 9
- SNP:
-
Single nucleotide polymorphism
- UA:
-
Uric acid
- BMI:
-
Body mass index
- WBC:
-
White blood cell
- HB:
-
Hemoglobin
- PLT:
-
Platelet
- GGT:
-
Gamma-glutamyl transferase
- TG:
-
Triglyceride
- TC:
-
Total cholesterol
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- GLU:
-
Glucose
- PA:
-
Palmitate
- OA:
-
Oleic acid
- FFA:
-
Free fatty acid
- MSU:
-
Monosodium urate
- SCD:
-
Standard chow diet
- HFD:
-
High-fat diet
- MCD:
-
Methionine- and choline-deficient diet
- H&E:
-
Hematoxylin and eosin
- GTT:
-
Glucose tolerance test
- ITT:
-
Insulin tolerance test
- DEME:
-
Dulbecco’s modified eagle medium
- FBS:
-
Fetal bovine serum
References
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209
Younossi ZM, Rinella ME, Sanyal AJ, Harrison SA, Brunt EM, Goodman Z, et al. From NAFLD to MAFLD: implications of a premature change in terminology. Hepatology 2021;73:1194–1198.
Tilg H, Effenberger M. From NAFLD to MAFLD: when pathophysiology succeeds. Nat Rev Gastroenterol Hepatol. 2020;17:387–388
Lee YJ, Lee HR, Lee JH, Shin YH, Shim JY. Association between serum uric acid and non-alcoholic fatty liver disease in Korean adults. Clin Chem Lab Med. 2010;48:175–180
Ryu S, Chang Y, Kim SG, Cho J, Guallar E. Serum uric acid levels predict incident nonalcoholic fatty liver disease in healthy Korean men. Metabolism. 2011;60:860–866
Huang F, Liu A, Fang H, Geng X. Serum uric acid levels in non-alcoholic steatosis patients: a meta-analysis. Asia Pac J Clin Nutr. 2017;26:334–342
Xu C, Yu C, Xu L, Miao M, Li Y. High serum uric acid increases the risk for nonalcoholic Fatty liver disease: a prospective observational study. PLoS ONE. 2010;5:e11578
Wan X, Xu C, Lin Y, Lu C, Li D, Sang J, et al. Uric acid regulates hepatic steatosis and insulin resistance through the NLRP3 inflammasome-dependent mechanism. J Hepatol. 2016;64:925–32.
Wan X, Xu C, Yu C. Role of the NLRP3 inflammasome in the progression of nonalcoholic fatty liver disease to nonalcoholic steatohepatitis. Can J Gastroenterol Hepatol. 2016;2016:6489012.
Nishikawa T, Nagata N, Shimakami T, Shirakura T, Matsui C, Ni Y, et al. Xanthine oxidase inhibition attenuates insulin resistance and diet-induced steatohepatitis in mice. Sci Rep. 2020;10:815
Lv Y, Gao X, Luo Y, Fan W, Shen T, Ding C, et al. Apigenin ameliorates HFD-induced NAFLD through regulation of the XO/NLRP3 pathways. J Nutr Biochem. 2019;71:110–121
Xu C, Wan X, Xu L, Weng H, Yan M, Miao M, et al. Xanthine oxidase in non-alcoholic fatty liver disease and hyperuricemia: one stone hits two birds. J Hepatol. 2015;62:1412–1419
So A, Thorens B. Uric acid transport and disease. J Clin Invest. 2010;120:1791–1799
Augustin R, Carayannopoulos MO, Dowd LO, Phay JE, Moley JF, Moley KH. Identification and characterization of human glucose transporter-like protein-9 (GLUT9): alternative splicing alters trafficking. J Biol Chem. 2004;279:16229–16236
Li S, Sanna S, Maschio A, Busonero F, Usala G, Mulas A, et al. The GLUT9 gene is associated with serum uric acid levels in Sardinia and Chianti cohorts. PLOS Genet. 2007;3:e194
Parsa A, Brown E, Weir MR, Fink JC, Shuldiner AR, Mitchell BD, et al. Genotype-based changes in serum uric acid affect blood pressure. Kidney Int. 2012;81:502–507
Testa A, Mallamaci F, Spoto B, Pisano A, Sanguedolce MC, Tripepi G, et al. Association of a polymorphism in a gene encoding a urate transporter with CKD Progression. Clin J Am Soc Nephrol. 2014;9:1059–1065
Mallamaci F, Testa A, Leonardis D, Tripepi R, Pisano A, Spoto B, et al. A genetic marker of uric acid level, carotid atherosclerosis, and arterial stiffness: a family-based study. Am J Kidney Dis. 2015;65:294–302
Das GE, Sakthiswary R, Lee SL, Wong SF, Hussein H, Gun SC. Clinical significance of SLC2A9/GLUT9 rs11722228 polymorphisms in gout. Int J Rheum Dis. 2018;21:705–709
Fujikawa H, Sakamoto Y, Masuda N, Oniki K, Kamei S, Nohara H, et al. Higher blood uric acid in female humans and mice as a protective factor against pathophysiological decline of lung function. Antioxidants (Basel) 2020;9:387
Stark K, Reinhard W, Neureuther K, Wiedmann S, Sedlacek K, Baessler A, et al. Association of common polymorphisms in GLUT9 gene with gout but not with coronary artery disease in a large case-control study. PLoS ONE. 2008;3:e1948
Zhang X, Yang X, Wang M, Li X, Xia Q, Xu S, et al. Association between SLC2A9 (GLUT9) gene polymorphisms and gout susceptibility: an updated meta-analysis. Rheumatol Int. 2016;36:1157–1165
Polasek O, Gunjaca G, Kolcic I, Zgaga L, Dzijan S, Smolic R, et al. Association of nephrolithiasis and gene for glucose transporter type 9 (SLC2A9): study of 145 patients. Croat Med J. 2010;51:48–53
Preitner F, Bonny O, Laverriere A, Rotman S, Firsov D, Da CA, et al. Glut9 is a major regulator of urate homeostasis and its genetic inactivation induces hyperuricosuria and urate nephropathy. Proc Natl Acad Sci USA. 2009;106:15501–15506
Preitner F, Laverriere-Loss A, Metref S, Da Costa A, Moret C, Rotman S, et al. Urate-induced acute renal failure and chronic inflammation in liver-specific Glut9 knockout mice. Am J Physiol-Renal. 2013;305:F786–F795
Fan JG, Farrell GC. Epidemiology of non-alcoholic fatty liver disease in China. J Hepatol. 2009;50:204–210
Zhang X, Lin Y, Lin S, Li C, Gao J, Feng Z, et al. Silencing of functional p53 attenuates NAFLD by promoting HMGB1-related autophagy induction. Hepatol Int. 2020;14:828–841
Speliotes EK, Yerges-Armstrong LM, Wu J, Hernaez R, Kim LJ, Palmer CD, et al. Genome-wide association analysis identifies variants associated with nonalcoholic fatty liver disease that have distinct effects on metabolic traits. PLOS Genet. 2011;7:e1001324
Liu W, Hung C, Chen S, Lin M, Chen L, Hwang D, et al. The rs1014290 polymorphism of the SLC2A9 gene is associated with type 2 diabetes mellitus in Han Chinese. Exp Diabetes Res. 2011;2011:527520
Lu J, Dalbeth N, Yin H, Li C, Merriman TR, Wei WH. Mouse models for human hyperuricaemia: a critical review. Nat Rev Rheumatol. 2019;15:413–426
Eng JM, Estall JL. Diet-induced models of non-alcoholic fatty liver disease: food for thought on sugar, fat, and cholesterol. Cells-Basel. 2021;10:1805
Funding
This work was supported by the National Natural Science Foundation of China [Grants 82030019].
Author information
Authors and Affiliations
Contributions
HZ and CY contributed to the study conception and design. Material preparation, data collection and analysis were performed by HZ, CT, BL. The first draft of the manuscript was written by HZ and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Animal research (ethics)
All procedures performed in studies involving animals were in accordance with the ethical standards of the Animal Care and Use Committee of the First Affiliated Hospital, Zhejiang University School of Medicine (reference number: 2021–133).
Consent to participate (ethics)
The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Ethic Committee of the First Affiliated Hospital, Zhejiang University School of Medicine (reference number: 2021-190). Informed consent was obtained from individual or guardian participants.
Consent to publish (ethics)
Not applicable.
Clinical trials registration
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zeng, H., Tang, C., Lin, B. et al. The regulation effect of GLUT9/SLC2A9 on intrahepatic uric acid level and metabolic associated fatty liver disease. Hepatol Int 16, 1064–1074 (2022). https://doi.org/10.1007/s12072-022-10371-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-022-10371-2