Abstract
Background and purpose
Radiofrequency ablation (RFA) is the standard of care for early stage hepatocellular carcinoma (HCC). However, the clinical outcomes of iodized oil computed tomography (IoCT) versus ultrasound (US)-guided RFA for HCC remain unclear.
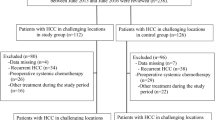
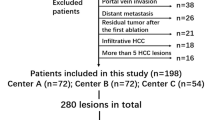
Methods
We retrospectively analyzed consecutive treatment-naïve patients who received curative RFA for HCC within Milan criteria from January 2016 to December 2018. Patients who underwent either IoCT-guided RFA (IoCT group) or US-guided RFA (US group) were included. Various clinical factors, including tumor location, were adjusted with a 1:1 propensity score matching. Subsequently, the cumulative incidence rates for recurrence and hazard ratios for survival were calculated.
Results
We included 184 (37.9%) and 301 (62.1%) patients who received IoCT- and US-guided RFA, respectively. Before propensity score matching, IoCT guidance was significantly associated with multiple tumors, higher body mass index, lower albumin level, and tumors located at S8. After matching, the 1-, 2-, and 3-year local tumor progression rates of the IoCT group were significantly lower than those of the US group (4.4%, 6.9%, and 7.5% vs. 14.4%, 16.3%, and 16.3%, respectively, at p = 0.002, 0.009, and 0.016, respectively). In univariate analyses and multivariate analyses that adjusted for clinical and tumor location-related parameters, the IoCT group had better recurrence-free survival (hazard ratio = 0.581, 95% confidence interval 0.375–0.899) than those with US guidance but not overall survival.
Conclusion
IoCT-guided RFA had a lower local tumor progression rate and better recurrence-free survival than did US-guided RFA for HCC within the Milan criteria.
Graphic abstract
-
CT-guide RFA is a safe and effective alternative to US-guided with similar overall survival.
-
IoCT-guided RFA might have a better local tumor control than US-guided.
-
IoCT-guided RFA may be more suitable for male patients, aged < 70 years, a single tumor measuring 2–5 cm, and a tumor located at the subdiaphragmatic/subcardiac region.




Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
European Association for the Study of the Liver, European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2012;56:908–943
Llovet JM, Bruix J. Novel advancements in the management of hepatocellular carcinoma in 2008. J Hepatol 2008;48(Suppl 1):S20-S37
Surveillance Group, Diagnosis Group, Staging Group, Surgery Group, Local ablation Group, TACE/TARE/HAI Group, et al. Management consensus guideline for hepatocellular carcinoma: 2016 updated by the Taiwan liver cancer association and the gastroenterological society of Taiwan. J Formos Med Assoc 2016;2018(117):381–403
Wong J, Lee KF, Yu CH, Lee SF, Cheung YS, Chong CN, et al. Percutaneous radiofrequency ablation versus surgical radiofrequency ablation for malignant liver tumours: the long-term results. HPB (Oxford). 2013;15:595–601
Kim YS, Lim HK, Rhim H, Lee MW, Choi D, Lee WJ, et al. Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: analysis of prognostic factors. J Hepatol 2013;58:89–97
Shiina S, Tateishi R, Arano T, Uchino K, Enooku K, Nakagawa H, et al. Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol 2012;107:569–577
Song I, Rhim H, Lim HK, Kim YS, Choi D. Percutaneous radiofrequency ablation of hepatocellular carcinoma abutting the diaphragm and gastrointestinal tracts with the use of artificial ascites: safety and technical efficacy in 143 patients. Eur Radiol 2009;19:2630–2640
Minami Y, Kudo M, Kawasaki T, Chung H, Ogawa C, Inoue T, et al. Percutaneous ultrasound-guided radiofrequency ablation with artificial pleural effusion for hepatocellular carcinoma in the hepatic dome. J Gastroenterol 2003;38:1066–1070
Song KD, Lee MW, Rhim H, Cha DI, Chong Y, Lim HK. Fusion imaging-guided radiofrequency ablation for hepatocellular carcinomas not visible on conventional ultrasound. Am J Roentgenol 2013;201:1141–1147
Ahn SJ, Lee JM, Lee DH, Lee SM, Yoon JH, Kim YJ, et al. Real-time US-CT/MR fusion imaging for percutaneous radiofrequency ablation of hepatocellular carcinoma. J Hepatol 2017;66:347–354
Teratani T, Yoshida H, Shiina S, Obi S, Sato S, Tateishi R, et al. Radiofrequency ablation for hepatocellular carcinoma in so-called high-risk locations. Hepatology 2006;43:1101–1108
Lee MW, Rhim H, Cha DI, Kim YJ, Choi D, Kim Y, et al. Percutaneous radiofrequency ablation of hepatocellular carcinoma: fusion imaging guidance for management of lesions with poor conspicuity at conventional sonography. Am J Roentgenol 2012;198:1438–1444
Park BJ, Byun JH, Jin YH, Won HJ, Shin YM, Kim KW, et al. CT-guided radiofrequency ablation for hepatocellular carcinomas that were undetectable at US: therapeutic effectiveness and safety. J Vasc Interv Radiol 2009;20:490–499
Laspas F, Sotiropoulou E, Mylona S, Manataki A, Tsagouli P, Tsangaridou I, et al. Computed tomography-guided radiofrequency ablation of hepatocellular carcinoma: treatment efficacy and complications. J Gastrointest Liver Dis 2009;18:323–328
Huo J, Aloia TA, Xu Y, Chung TH, Sheu T, Shih YC. comparative effectiveness of computed tomography- versus ultrasound-guided percutaneous radiofrequency ablation among medicare patients 65 years of age or older with hepatocellular carcinoma. Value Health 2019;22:284–292
Lee LH, Hwang JI, Cheng YC, Wu CY, Lee SW, Yang SS, et al. Comparable outcomes of ultrasound versus computed tomography in the guidance of radiofrequency ablation for hepatocellular carcinoma. PLOS ONE 2017. https://doi.org/10.1371/journal.pone.0169655
Kitamoto M, Imagawa M, Yamada H, Watanabe C, Sumioka M, Satoh O, et al. Radiofrequency ablation in the treatment of small hepatocellular carcinomas: comparison of the radiofrequency effect with and without chemoembolization. Am J Roentgenol 2003;181:997–1003
Nishikawa H, Inuzuka T, Takeda H, Nakajima J, Sakamoto A, Henmi S, et al. Percutaneous radiofrequency ablation therapy for hepatocellular carcinoma: a proposed new grading system for the ablative margin and prediction of local tumor progression and its validation. J Gastroenterol 2011;46:1418–1426
Kim W, Cho SK, Shin SW, Hyun D, Lee MW, Rhim H. Combination therapy of transarterial chemoembolization (TACE) and radiofrequency ablation (RFA) for small hepatocellular carcinoma: comparison with TACE or RFA monotherapy. Abdom Radiol (NY) 2019;44:2283–2292
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 2015;33:550–558
Ahmed M, Solbiati L, Brace CL, Breen DJ, Callstrom MR, Charboneau JW, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria–a 10-year update. Radiology 2014;273:241–260
Khalilzadeh O, Baerlocher MO, Shyn PB, Connolly BL, Devane AM, Morris CS, et al. Proposal of a new adverse event classification by the society of interventional radiology standards of practice committee. J Vasc Interv Radiol 2017;28:1432–1437
Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Randomised controlled trial comparing percutaneous radiofrequency thermal ablation, percutaneous ethanol injection, and percutaneous acetic acid injection to treat hepatocellular carcinoma of 3 cm or less. Gut 2005;54:1151–1156
Gandhi S, Iannitti DA, Mayo-Smith WW, Dupuy DE. Technical report: lipiodol-guided computed tomography for radiofrequency ablation of hepatocellular carcinoma. Clin Radiol 2006;61:888–891
Paul SB, Vidyasagar R, Dhamija E, Gamanagatti SR, Shalimar S, Acharya SK. Utility of lipiodol CT for treating small hepatocellular carcinoma. J Clin Exp Hepatol 2017;7:S80
Veltri A, Moretto P, Doriguzzi A, Pagano E, Carrara G, Gandini G. Radiofrequency thermal ablation (RFA) after transarterial chemoembolization (TACE) as a combined therapy for unresectable non-early hepatocellular carcinoma (HCC). Eur Radiol 2006;16:661–669
Kim JH, Won HJ, Shin YM, Kim SH, Yoon H-K, Sung K-B, et al. Medium-sized (3.1-5.0 cm) hepatocellular carcinoma: transarterial chemoembolization plus radiofrequency ablation versus radiofrequency ablation alone. Ann Surg Oncol 2011;18:1624–1629
Shibata T, Isoda H, Hirokawa Y, Arizono S, Shimada K, Togashi K. Small hepatocellular carcinoma: is radiofrequency ablation combined with transcatheter arterial chemoembolization more effective than radiofrequency ablation alone for treatment? Radiology. Radiol Soc N Am 2009;252:905–913
Rossi S, Garbagnati F, Lencioni R, Allgaier H-P, Marchianò A, Fornari F, et al. Percutaneous radio-frequency thermal ablation of nonresectable hepatocellular carcinoma after occlusion of tumor blood supply. Radiology. Radiol Soc N Am 2000;217:119–126
Kao W-Y, Su C-W, Chiou Y-Y, Chiu N-C, Liu C-A, Fang K-C, et al. Hepatocellular carcinoma: nomograms based on the albumin-bilirubin grade to assess the outcomes of radiofrequency ablation. Radiology. Radiol Soc N Am 2017;285:670–680
Acknowledgements
The study was financially sponsored by National Taiwan University Hospital (108-M4430, 109-M4557), Industrial Technology Research Institute cooperation research project (PC1231-108, PC1281-109) and 2020 scholarship of Taiwan Health Foundation. Part of this study was presented as oral presentations at the 6th Asian Conference on Tumor Ablation in Taiwan (ACTA 2019), October 26-27, 2019, Chiayi County, Taiwan and at the 15th Annual Scientific Meeting of Asia Pacific Society of Cardiovascular and Interventional Radiology (APSCVIR 2021), February 26-28, 2021, virtual congress, Taipei, Taiwan.
Funding
The study was financially sponsored by National Taiwan University Hospital (108-M4430, 109-M4557), Industrial Technology Research Institute cooperation research project (PC1231-108, PC1281-109) and 2020 scholarship of Taiwan Health Foundation.
Author information
Authors and Affiliations
Contributions
All authors were aware of and agree to the submission and that they had all contributed to the work described sufficiently to be named as authors. C-HW was responsible for manuscript writing, statistical analysis. T-HS was contributed clinical data collection. P-CL and M-CL gave help to the image collecting and RFA technique. Y-HC illustrated Fig. 1 and gave help to the data analysis. TT-TS and J-HK designed the study and revise the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors Chih-Horng Wu, Po-Chin Liang, Tung-Hung Su, Ming-Chi Lin, Yu-Hsuan Chang, Tiffany Ting-Fang Shih, Jia-Horng Kao declare that they have no conflict of interest.
Ethics approval
All clinical information, laboratory data, and images were collected under routine workup. This study followed the Health Insurance Portability and Accountability Act guidelines, Declaration of Helsinki of 1975, as revised in 2008 and Institutional Review Board of National Taiwan University Hospital approval was obtained (NTUH-201904025RINA).
Consent to participate
Written informed consent was waived for this study because this is a retrospective study.
Consent to publication
All authors were aware of and agree to the submission and that they had all contributed to the work described sufficiently to be named as authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, CH., Liang, PC., Su, TH. et al. Iodized oil computed tomography versus ultrasound-guided radiofrequency ablation for early hepatocellular carcinoma. Hepatol Int 15, 1247–1257 (2021). https://doi.org/10.1007/s12072-021-10236-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10236-0