Abstract
Background
Concomitant chronic hepatitis B infection (CHB) and non-alcoholic fatty liver disease (NAFLD) is common, but the implications of NAFLD on clinical outcomes of CHB, including hepatocellular carcinoma (HCC), are not well-investigated.
Methods
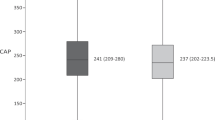
CHB patients were recruited for transient elastography assessment for liver stiffness (LS), and controlled attenuation parameter (CAP), a non-invasive quantification of hepatic steatosis, and were prospectively followed up for development of HCC. Steatosis and severe steatosis were diagnosed by CAP ≥ 248 dB/m and ≥ 280 dB/m respectively, and advanced fibrosis/cirrhosis was diagnosed by LS ≥ 9 kPa. The independent effect of hepatic steatosis on HCC was examined via propensity score matching (PSM) of LS and other significant clinical variables.
Results
Forty-eight patients developed HCC among 2403 CHB patients (55.6% male, median age 55.6 years, 57.1% antiviral-treated, median ALT 26 U/L) during a median follow-up of 46.4 months. Multivariate Cox regression analysis showed age (HR 1.063), male (HR 2.032), Albumin-Bilirubin score (HR 2.393) and CAP (HR 0.993) were associated with HCC development. The cumulative probability of HCC was 2.88%, 1.56% and 0.71%, respectively for patients with no steatosis, mild-to-moderate steatosis, and severe steatosis, respectively (p = 0.01). The risk of HCC increased from 1.56 to 8.89% in patients without severe steatosis if advanced fibrosis/cirrhosis was present (p < 0.001). PSM yielded 957 pairs of CHB patients and hepatic steatosis was independently associated with HCC (HR 0.41).
Conclusion
Reduced hepatic steatosis was significantly associated with a higher risk of incident HCC in CHB infection. Routine CAP and LS measurements are important for risk stratification.




Similar content being viewed by others
Data availability
Data available within the article or its supplementary materials.
Abbreviations
- CHB:
-
Chronic hepatitis B
- NAFLD:
-
Non-alcoholic fatty liver disease
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- HBV:
-
Hepatitis B virus
- HBsAg:
-
Hepatitis B surface antigen
- NA:
-
Nucleos(t)ide analogue
- CAP:
-
Controlled attenuation parameter
- HbA1c:
-
Glycated hemoglobin
- FG:
-
Fasting glucose
- TG:
-
Triglyceride
- LDL:
-
Low density lipoprotein
- HDL:
-
High density lipoprotein
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- HBeAg:
-
Hepatitis B e antigen
- LS:
-
Liver stiffness
- F0/F1:
-
No/minimal fibrosis
- F3:
-
Advanced fibrosis
- F4:
-
Cirrhosis
- dB/m:
-
Decibel/ meter
- IQR:
-
Interquartile range
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- NASH:
-
Non-alcoholic steatohepatitis
- HBcAg:
-
Hepatitis B core antigen
References
Polaris OC. Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol. 2018;3:383–403.
Li J, Zou B, Yeo YH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4:389–98.
Fattovich G, Bortolotti F, Donato F. Natural history of chronic hepatitis B: special emphasis on disease progression and prognostic factors. J Hepatol. 2008;48:335–52.
Mak LY, Cruz-Ramon V, Chinchilla-Lopez P, et al. Global epidemiology, prevention, and management of hepatocellular carcinoma. Am Soc Clin Oncol Educ Book. 2018;38:262–79.
Shi JP, Fan JG, Wu R, et al. Prevalence and risk factors of hepatic steatosis and its impact on liver injury in Chinese patients with chronic hepatitis B infection. J Gastroenterol Hepatol. 2008;23:1419–25.
Yun JW, Cho YK, Park JH, et al. Hepatic steatosis and fibrosis in young men with treatment-naive chronic hepatitis B. Liver Int. 2009;29:878–83.
Zhang C, Wang J, Zhang H, et al. Hepatitis C virus core protein induces hepatic steatosis via Sirt1-dependent pathway. Liver Int. 2018;38:803–12.
Perlemuter G, Sabile A, Letteron P, et al. Hepatitis C virus core protein inhibits microsomal triglyceride transfer protein activity and very low density lipoprotein secretion: a model of viral-related steatosis. FASEB J. 2002;16:185–94.
Joo EJ, Chang Y, Yeom JS, et al. Hepatitis B virus infection and decreased risk of nonalcoholic fatty liver disease: a cohort study. Hepatology. 2017;65:828–35.
Machado MV, Oliveira AG, Cortez-Pinto H. Hepatic steatosis in hepatitis B virus infected patients: meta-analysis of risk factors and comparison with hepatitis C infected patients. J Gastroenterol Hepatol. 2011;26:1361–7.
Hui RWH, Seto WK, Cheung KS, et al. Inverse relationship between hepatic steatosis and hepatitis B viremia: results of a large case-control study. J Viral Hepat. 2018;25:97–104.
Chu CM, Lin DY, Liaw YF. Clinical and virological characteristics post HBsAg seroclearance in hepatitis B virus carriers with hepatic steatosis versus those without. Dig Dis Sci. 2013;58:275–81.
Fung J, Yuen MF, Lai CL. The role of steatosis in HBsAg seroclearance for patients with chronic hepatitis B infection: fact or fiction? Dig Dis Sci. 2013;58:20–2.
Seto WK, Hui RWH, Mak LY, et al. Association Between Hepatic Steatosis, Measured by Controlled Attenuation Parameter, and Fibrosis Burden in Chronic Hepatitis B. Clin Gastroenterol Hepatol. 2018;16:575-583 e2.
Mak LY, Seto WK, Hui RW, et al. Fibrosis evolution in chronic hepatitis B e antigen-negative patients across a 10-year interval. J Viral Hepat. 2019;26:818–27.
Lim JK, Flamm SL, Singh S, et al. American gastroenterological association institute guideline on the role of elastography in the evaluation of liver fibrosis. Gastroenterology. 2017;152:1536–43.
Friedrich-Rust M, Ong MF, Martens S, et al. Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology. 2008;134:960–74.
Castera L, Forns X, Alberti A. Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol. 2008;48:835–47.
Karlas T, Petroff D, Sasso M, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66:1022–30.
Petroff D, Blank V, Newsome PN, et al. Assessment of hepatic steatosis by controlled attenuation parameter using the M and XL probes: an individual patient data meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:185–98.
Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33:550–8.
Mak LY, Cloherty G, Wong DK, et al. HBV RNA profiles in chronic hepatitis B patients under different disease phases and anti-viral therapy. Hepatology. 2020. https://doi.org/10.1002/hep.31616.
Lam YF, Seto WK, Wong D, et al. Seven-year treatment outcome of entecavir in a real-world cohort: effects on clinical parameters, HBsAg and HBcrAg levels. Clin Transl Gastroenterol. 2017;8:e125.
European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236.
Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the american association for the study of liver diseases. Hepatology. 2018;68:723–50.
European Association for Study of Liver. Asociacion Latinoamericana para el Estudio del Higado clinical practice guidelines: non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63:237–64.
Wong VW, Petta S, Hiriart JB, et al. Validity criteria for the diagnosis of fatty liver by M probe-based controlled attenuation parameter. J Hepatol. 2017;67:577–84.
Hu D, Wang H, Wang H, et al. Non-alcoholic hepatic steatosis attenuates hepatitis B virus replication in an HBV-immunocompetent mouse model. Hepatol Int. 2018;12:438–46.
Zhang Z, Pan Q, Duan XY, et al. Fatty liver reduces hepatitis B virus replication in a genotype B hepatitis B virus transgenic mice model. J Gastroenterol Hepatol. 2012;27:1858–64.
Mak LY, Hui RW, Fung J, et al. Diverse effects of hepatic steatosis on fibrosis progression and functional cure in virologically quiescent chronic hepatitis B. J Hepatol. 2020;73:800–6.
Wang MM, Wang GS, Shen F, et al. Hepatic steatosis is highly prevalent in hepatitis B patients and negatively associated with virological factors. Dig Dis Sci. 2014;59:2571–9.
Powell EE, Cooksley WG, Hanson R, et al. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatology. 1990;11:74–80.
van der Poorten D, Samer CF, Ramezani-Moghadam M, et al. Hepatic fat loss in advanced nonalcoholic steatohepatitis: are alterations in serum adiponectin the cause? Hepatology. 2013;57:2180–8.
Fattovich G. Natural history of hepatitis B. J Hepatol. 2003;39(Suppl 1):S50–8.
Yuen MF, Chen DS, Dusheiko GM, et al. Hepatitis B virus infection. Nat Rev Dis Primers. 2018;4:18035.
Sarin SK, Kumar M, Lau GK, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10:1–98.
Kraja AT, Borecki IB, North K, et al. Longitudinal and age trends of metabolic syndrome and its risk factors: the Family Heart Study. Nutr Metab (Lond). 2006;3:41.
Kuk JL, Ardern CI. Age and sex differences in the clustering of metabolic syndrome factors: association with mortality risk. Diabetes Care. 2010;33:2457–61.
Ozaki R, Qiao Q, Wong GW, et al. Overweight, family history of diabetes and attending schools of lower academic grading are independent predictors for metabolic syndrome in Hong Kong Chinese adolescents. Arch Dis Child. 2007;92:224–8.
Fung J, Lee CK, Chan M, et al. High prevalence of non-alcoholic fatty liver disease in the Chinese—results from the Hong Kong liver health census. Liver Int. 2015;35:542–9.
Singh S, Allen AM, Wang Z, et al. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 2015;13:643–54-e19 (Quiz e39–40).
Fung J, Lai CL, But D, et al. Reduction of liver stiffness following resolution of acute flares of chronic hepatitis B. Hepatol Int. 2010;4:716–22.
Shen F, Mi YQ, Xu L, et al. Moderate to severe hepatic steatosis leads to overestimation of liver stiffness measurement in chronic hepatitis B patients without significant fibrosis. Aliment Pharmacol Ther. 2019;50:93–102.
Millonig G, Reimann FM, Friedrich S, et al. Extrahepatic cholestasis increases liver stiffness (FibroScan) irrespective of fibrosis. Hepatology. 2008;48:1718–23.
Colli A, Pozzoni P, Berzuini A, et al. Decompensated chronic heart failure: increased liver stiffness measured by means of transient elastography. Radiology. 2010;257:872–8.
Hopper I, Kemp W, Porapakkham P, et al. Impact of heart failure and changes to volume status on liver stiffness: non-invasive assessment using transient elastography. Eur J Heart Fail. 2012;14:621–7.
Wong GL, Vergniol J, Lo P, et al. Non-invasive assessment of liver fibrosis with transient elastography (FibroScan(R)): applying the cut-offs of M probe to XL probe. Ann Hepatol. 2013;12:570–80.
Fujimori N, Tanaka N, Shibata S, et al. Controlled attenuation parameter is correlated with actual hepatic fat content in patients with non-alcoholic fatty liver disease with none-to-mild obesity and liver fibrosis. Hepatol Res. 2016;46:1019–27.
Eddowes PJ, Sasso M, Allison M, et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156:1717–30.
Wong VW, Vergniol J, Wong GL, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology. 2010;51:454–62.
de Ledinghen V, Vergniol J, Foucher J, et al. Non-invasive diagnosis of liver steatosis using controlled attenuation parameter (CAP) and transient elastography. Liver Int. 2012;32:911–8.
Pu K, Wang Y, Bai S, et al. Diagnostic accuracy of controlled attenuation parameter (CAP) as a non-invasive test for steatosis in suspected non-alcoholic fatty liver disease: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19:51.
Yuen MF, Tanaka Y, Fong DY, et al. Independent risk factors and predictive score for the development of hepatocellular carcinoma in chronic hepatitis B. J Hepatol. 2009;50:80–8.
Acknowledgements
The interim results of this study was presented in the Digital Liver Meeting 2020 as a poster (Hepatology 2020; volume 72, issue number 1 supplementary, P.658A; poster number 1084). The authors would like to thank Ms. Carmen Chan, Ms. Carol Chu and Mr. Justin Ma for the logistical arrangement of patients.
Funding
This study was supported by the General Research Fund, Research Grants Council, The Government of the Hong Kong Special Administrative Region (ref no: 17125916); Innovative Research Fund of the State Key Laboratory of Liver Research, The University of Hong Kong (Ref no: SKLLR/IRF/2018/08); and the Outstanding Young Researcher Award, The University of Hong Kong.
Author information
Authors and Affiliations
Contributions
The authors declare they have participated in the preparation of the manuscript and have seen and approved the final version. LYM was involved in data acquisition, data analysis and interpretation, and drafting of manuscript. RWHH and KSC were involved in data acquisition and analysis. FL and DKHW were involved in data acquisition. BL was responsible for analysis of data. JF and MFY was involved in critical revision of manuscript. WKS was involved in study concept and design, analysis and interpretation of data, critical revision of manuscript and overall study supervision.
Corresponding authors
Ethics declarations
Conflict of interest
J Fung has been a consultant for Gilead Sciences. MF Yuen received speaker fees and received research funding from Bristol-Myers Squibb and Gilead Sciences. WKS received speaker fees from Mylan and is an advisory board member, received speaker fees and research funding from Gilead Sciences. All other authors: none to declare.
Ethical approval
The present study was approved by the Institutional Review Board/Ethics Committee of the University of Hong Kong and the Hong Kong West Cluster of Hospital Authority.
Informed consent
Written informed consent was obtained from all study subjects prior to any study-related procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mak, LY., Hui, R.WH., Fung, J. et al. Reduced hepatic steatosis is associated with higher risk of hepatocellular carcinoma in chronic hepatitis B infection. Hepatol Int 15, 901–911 (2021). https://doi.org/10.1007/s12072-021-10218-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10218-2