Abstract
Background and aim
Non-alcoholic fatty liver disease (NAFLD) is a very common liver disease which has been associated with a number of the extrahepatic manifestations (EHMs) and healthcare expenditures. Our aim was to assess the presence and impact of these EHMs of NAFLD on mortality and healthcare expenditures.
Methods
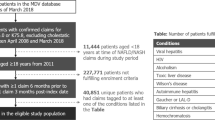
Medicare beneficiaries (2005–2016) were included. ICD-9 and ICD-10 codes were used to identify patients with NAFLD and EHMs which included cardiovascular disease (CVD), hypertension (HTN), diabetes (DM), hyperlipidemia (HL), non-hepatocellular carcinoma (HCC) cancers, and others. Temporal trends among different groups were analyzed by join point regression model. Independent predictors of outcomes were evaluated in multiple generalized linear or logistic regression models.
Results
Among 30,908,679 Medicare beneficiaries (5% sample of Medicare data from 2005–2016), 1,980,950 (6.4%) had NAFLD diagnosis. From 2005 to 2016, the prevalence of NAFLD in the Medicare population increased at an average annual increase of 3.1%. The most common diseases associated with NAFLD were DM (86.3%), followed by HTN (85.2%), HL (79.8%), and CVD (35.8%). One-year mortality rate in NAFLD patients increased from 3.55 to 6.33 per 1000 from 2005 to 2016. One-year mortality was independently associated with diagnosis of HCC, cirrhosis, DM (outpatient), depression, dementia, lung disease, renal failure, thyroid disorder (inpatient), neurological disorder as well as non-HCC cancers.
Conclusion
NAFLD is associated with a number of EHMs that increases its mortality and increased healthcare expenditure.


Similar content being viewed by others
Abbreviations
- NAFLD:
-
Non-alcoholic fatty liver disease
- MS:
-
Metabolic syndrome
- CVD:
-
Cardiovascular disease
- CKD:
-
Chronic kidney disease
- OSA:
-
Obstructive sleep apnea
- EHM:
-
Extrahepatic manifestation
- AAPC:
-
The average annual percent change
- CCI:
-
Charlson Comorbidity Index
- DM:
-
Diabetes mellitus
- HCC:
-
Hepatocellular carcinoma
- HL:
-
Hyperlipidemia
- HTN:
-
Hypertension
References
Sayiner M, Koenig A, Henry L, Younossi ZM. Epidemiology of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis in the United States and the rest of the World. Clin Liver Dis [Internet]. 2016;20:205–214. https://doi.org/10.1016/j.cld.2015.10.001
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes [Internet]. Hepatology. 2016. https://doi.org/10.1002/hep.28431
Ahmed A, Wong RJ, Harrison SA. Nonalcoholic fatty liver disease review: diagnosis, treatment, and outcomes. Clin Gastroenterol Hepatol [Internet]. 2015;13:2062–2070. https://doi.org/10.1016/j.cgh.2015.07.029
Wong RJ, Aguilar M, Cheung R, Perumpail RB, Harrison SA, Younossi ZM, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States [Internet]. Gastroenterology. 2015. https://doi.org/10.1053/j.gastro.2014.11.039
Mikolasevic I, Milic S, Turk Wensveen T, Grgic I, Jakopcic I, Stimac D, et al. Nonalcoholic fatty liver disease—a multisystem disease? World J Gastroenterol [Internet]. 2016;22:9488–9505. https://doi.org/10.3748/wjg.v22.i43.9488
Siddiqui MS, Fuchs M, Idowu MO, Luketic VA, Boyett S, Sargeant C, et al. Severity of nonalcoholic fatty liver disease and progression to cirrhosis are associated with atherogenic lipoprotein profile. Clin Gastroenterol Hepatol [Internet]. 2015;13:1000–1008. https://doi.org/10.1016/j.cgh.2014.10.008 (e3)
Mantovani A, Pernigo M, Bergamini C, Bonapace S, Lipari P, Pichiri I, et al. Nonalcoholic fatty liver disease is independently associated with early left ventricular diastolic dysfunction in patients with type 2 diabetes. PLoS One [Internet]. 2015;10:e0135329. https://doi.org/10.1371/journal.pone.0135329
Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol [Internet]. 2015;62:S47–S64. https://doi.org/10.1016/j.jhep.2014.12.012
Machado M, Marques-Vidal P, Cortez-Pinto H. Hepatic histology in obese patients undergoing bariatric surgery. J Hepatol [Internet]. 2006;45:600–606. https://doi.org/10.1016/j.jhep.2006.06.013
Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients [Internet]. 2013;5:1544–1560. https://doi.org/10.3390/nu5051544
Younossi ZM, Henry L. Economic and quality-of-life implications of non-alcoholic fatty liver disease. Pharmacoeconomics [Internet]. 2015;33:1245–1253. https://doi.org/10.1007/s40273-015-0316-5
Younossi ZM, Zheng L, Stepanova M, Henry L, Venkatesan C, Mishra A. Trends in outpatient resource utilizations and outcomes for medicare beneficiaries with nonalcoholic fatty liver disease. J Clin Gastroenterol [Internet]. 2015;49:222–227. https://doi.org/10.1097/MCG.0000000000000071
Paik JM, Henry L, Golabi P, Alqahtani SA, Trimble G, Younossi ZM. Presumed nonalcoholic fatty liver disease among medicare beneficiaries with HIV, 2006–2016. Open Forum Infect Dis [Internet]. 2020;7:ofz509. https://doi.org/10.1093/ofid/ofz509
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care [Internet]. 2005;43:1130–1139. https://www.ncbi.nlm.nih.gov/pubmed/16224307
Center of Medicare & Medicaid Services. CMS Medicare Denominator File Documentation [Internet]. Center of Medicare & Medicaid Services. 2017. https://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/LimitedDataSets/DenominatorLDS.html. Accessed 1 Apr 2018
Joinpoint Regression Program, Version 4.6.0.0—April 2018; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute [Internet]. 2018. https://surveillance.cancer.gov/joinpoint/. Accessed 7 Apr 2020
Royall RM. Model robust confidence intervals using maximum likelihood estimators. Int Stat Rev [Internet]. [Wiley, International Statistical Institute (ISI)]; 1986;54:221–6. https://www.jstor.org/stable/1403146
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol [Internet]. 2004;159:702–706. https://www.ncbi.nlm.nih.gov/pubmed/15033648
Petersen MR, Deddens JA. A comparison of two methods for estimating prevalence ratios. BMC Med Res Methodol [Internet]. 2008;8:9. https://doi.org/10.1186/1471-2288-8-9
Enderlein G, McCullagh P, Nelder JA. Generalized linear models (Chapman and Hall London, New York 1983, 261 S., £ 16). Biomed J [Internet]. 1987;37:206. https://doi.org/10.1002/bimj.4710290217
Sayiner M, Otgonsuren M, Cable R, Younossi I, Afendy M, Golabi P, et al. Variables associated with inpatient and outpatient resource utilization among medicare beneficiaries with nonalcoholic fatty liver disease with or without cirrhosis. J Clin Gastroenterol [Internet]. 2017;51:254–260. https://doi.org/10.1097/MCG.0000000000000567
Noureddin M, Vipani A, Bresee C, Todo T, Kim IK, Alkhouri N, et al. NASH leading cause of liver transplant in female: updated analysis of indications for liver transplant and ethnic and gender variances. Am J Gastroenterol [Internet]. 2018;113:1649–1659. https://doi.org/10.1038/s41395-018-0088-6
U.S. Department of Heath &Human Services Office of Minority Health [Internet]. HHS.gov. 2019. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=33. Accessed 5 Jan 2020
Golabi P, Locklear CT, Austin P, Afdhal S, Byrns M, Gerber L, et al. Effectiveness of exercise in hepatic fat mobilization in non-alcoholic fatty liver disease: systematic review. World J Gastroenterol [Internet]. 2016;22:6318–6327. https://doi.org/10.3748/wjg.v22.i27.6318
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology [Internet]. 2018;67:328–357. https://doi.org/10.1002/hep.29367
Younossi ZM, Otgonsuren M, Venkatesan C, Mishra A. In patients with non-alcoholic fatty liver disease, metabolically abnormal individuals are at a higher risk for mortality while metabolically normal individuals are not. Metabolism [Internet]. 2013;62:352–360. https://doi.org/10.1016/j.metabol.2012.08.005
Stepanova M, Rafiq N, Younossi ZM. Components of metabolic syndrome are independent predictors of mortality in patients with chronic liver disease: a population-based study. Gut [Internet]. 2010;59:1410–1415. https://doi.org/10.1136/gut.2010.213553
Golabi P, Otgonsuren M, de Avila L, Sayiner M, Rafiq N, Younossi ZM. Components of metabolic syndrome increase the risk of mortality in nonalcoholic fatty liver disease (NAFLD). Medicine [Internet]. 2018;97:e0214. https://doi.org/10.1097/MD.0000000000010214
Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol [Internet]. 2012;10:646–650. https://doi.org/10.1016/j.cgh.2011.12.039
Ballestri S, Lonardo A, Bonapace S, Byrne CD, Loria P, Targher G. Risk of cardiovascular, cardiac and arrhythmic complications in patients with non-alcoholic fatty liver disease. World J Gastroenterol [Internet]. 2014;20:1724–1745. https://doi.org/10.3748/wjg.v20.i7.1724
Lee J-M, Park Y-M, Yun J-S, Ahn Y-B, Lee K-M, Kim DB, et al. The association between nonalcoholic fatty liver disease and esophageal, stomach, or colorectal cancer: National population-based cohort study. PLoS One [Internet]. 2020;15:e0226351. https://doi.org/10.1371/journal.pone.0226351
Wu K, Zhai MZ, Weltzien EK, Cespedes Feliciano EM, Meyerhardt JA, Giovannucci E, et al. Non-alcoholic fatty liver disease and colorectal cancer survival. Cancer Causes Control [Internet]. 2019;30:165–168. https://doi.org/10.1007/s10552-018-1095-z
Weinstein G, Zelber-Sagi S, Preis SR, Beiser AS, DeCarli C, Speliotes EK, et al. Association of nonalcoholic fatty liver disease with lower brain volume in healthy middle-aged adults in the framingham study. JAMA Neurol [Internet]. 2018;75:97–104. https://doi.org/10.1001/jamaneurol.2017.3229
Seo SW, Gottesman RF, Clark JM, Hernaez R, Chang Y, Kim C, et al. Nonalcoholic fatty liver disease is associated with cognitive function in adults. Neurology [Internet]. 2016;86:1136–1142. https://doi.org/10.1212/WNL.0000000000002498
Mesarwi OA, Loomba R, Malhotra A. Obstructive sleep apnea, hypoxia, and nonalcoholic fatty liver disease. Am J Respir Crit Care Med [Internet]. 2018. https://doi.org/10.1164/rccm.201806-1109TR
Gordon S, Fraysse J, Li S, Ozbay AB, Wong RJ. Disease severity is associated with higher healthcare utilization in nonalcoholic steatohepatitis medicare patients. Am J Gastroenterol [Internet]. 2019. https://doi.org/10.14309/ajg.0000000000000484
Hester D, Golabi P, Paik J, Younossi I, Mishra A, Younossi ZM. Among medicare patients with hepatocellular carcinoma, non-alcoholic fatty liver disease is the most common etiology and cause of mortality. J Clin Gastroenterol [Internet]. 2019. https://doi.org/10.1097/MCG.0000000000001172
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Younossi is a consultant to BMS, Gilead, Intercept, NovoNordisk. Novartis, Terns, Merck, Viking, and Shinogi. All other authors have no conflict of interest to disclose. Mehmet Sayiner, Tamoore Arshad, Pegah Golabi, James Paik, Freba Farhat, Zobair M. Younossi read and approved the final version of the manuscript.
Guarantor of article
Zobair M. Younossi is the guarantor of this work, and had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. This study was approved as “exempt” by the Inova Health Systems Internal Review Board located in Falls Church, VA, prior to the start of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sayiner, M., Arshad, T., Golabi, P. et al. Extrahepatic manifestations and healthcare expenditures of non-alcoholic fatty liver disease in the Medicare population. Hepatol Int 14, 556–566 (2020). https://doi.org/10.1007/s12072-020-10038-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-020-10038-w