Abstract
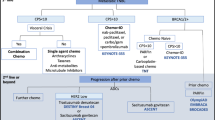
Approximately, 15% of global breast cancer cases are diagnosed as triple-negative breast cancer (TNBC), identified as the most aggressive subtype due to the simultaneous absence of estrogen receptor, progesterone receptor, and HER2. This characteristic renders TNBC highly aggressive and challenging to treat, as it excludes the use of effective drugs such as hormone therapy and anti-HER2 agents. In this review, we explore standard therapies and recent emerging approaches for TNBC, including PARP inhibitors, immune checkpoint inhibitors, PI3K/AKT pathway inhibitors, and cytotoxin-conjugated antibodies. The mechanism of action of these drugs and their utilization in clinical practice is explained in a pragmatic and prospective manner, contextualized within the current landscape of standard therapies for this pathology. These advancements present a promising frontier for tailored interventions with the potential to significantly improve outcomes for TNBC patients. Interestingly, while TNBC poses a complex challenge, it also serves as a paradigm and an opportunity for translational research and innovative therapies in the field of oncology.





Similar content being viewed by others
References
Neophytou C, Boutsikos P, Papageorgis P. Molecular mechanisms and emerging therapeutic targets of triple-negative breast cancer metastasis. Front Oncol. 2018;8:31.
Anders CK, Carey LA. Biology, metastatic patterns, and treatment of patients with triple-negative breast cancer. Clin Breast Cancer. 2009;9:S73–81.
Borri F, Granaglia A. Pathology of triple negative breast cancer. Semin Cancer Biol. 2021;72:136–45.
Petrucelli N, Daly MB, Pal T, BRCA1-and BRCA2-associated hereditary breast and ovarian cancer. 2022
Vishnubalaji R, Alajez NM. Single-cell transcriptome analysis revealed heterogeneity and identified novel therapeutic targets for breast cancer subtypes. Cells. 2023;12:1182.
Akhouayri L, Ostano P, Mello-Grand M, Gregnanin I, Crivelli F, Laurora S, et al. Identification of a minimum number of genes to predict triple-negative breast cancer subgroups from gene expression profiles. Hum Genomics. 2022;16:1–17.
Lehmann BD, Jovanović B, Chen X, Estrada MV, Johnson KN, Shyr Y, et al. Refinement of triple-negative breast cancer molecular subtypes: implications for neoadjuvant chemotherapy selection. PLoS ONE. 2016;11: e0157368.
Masuda H, Baggerly KA, Wang Y, Zhang Y, Gonzalez-Angulo AM, Meric-Bernstam F, et al. Differential response to neoadjuvant chemotherapy among 7 triple-negative breast cancer molecular subtypes. Clin Cancer Res. 2013;19:5533–40.
Burstein MD, Tsimelzon A, Poage GM, Covington KR, Contreras A, Fuqua SA, et al. Comprehensive genomic analysis identifies novel subtypes and targets of triple-negative breast cancer. Clin Cancer Res. 2015;21:1688–98.
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y, et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Investig. 2011;121:2750–67.
Yu K-D, Zhu R, Zhan M, Rodriguez AA, Yang W, Wong S, et al. Identification of prognosis-relevant subgroups in patients with chemoresistant triple-negative breast cancer. Clin Cancer Res. 2013;19:2723–33.
Prat A, Parker JS, Karginova O, Fan C, Livasy C, Herschkowitz JI, et al. Phenotypic and molecular characterization of the claudin-low intrinsic subtype of breast cancer. Breast Cancer Res. 2010;12:1–18.
Staiger C, Cadot S, Györffy B, Wessels LF, Klau GW. Current composite-feature classification methods do not outperform simple single-genes classifiers in breast cancer prognosis. Front Genet. 2013;4:289.
Xu Y, Xu Q, Yang L, Ye X, Liu F, Wu F, et al. Identification and validation of a blood-based 18-gene expression signature in colorectal cancer. Clin Cancer Res. 2013;19:3039–49.
Sabatier R, Diéras V, Pivot X, Brain E, Roche H, Extra J-M, et al. Safety results and analysis of eribulin efficacy according to previous microtubules-inhibitors sensitivity in the French prospective expanded access program for heavily pre-treated metastatic breast cancer. Cancer Res Treat. 2018;50:1226–37.
Watanabe G, Chiba N, Nomizu T, Furuta A, Sato K, Miyashita M, et al. Increased centrosome number in BRCA-related breast cancer specimens determined by immunofluorescence analysis. Cancer Sci. 2018;109:2027–35.
Kang SY, Kim YS, Kim Z, Kim HY, Kim HJ, Park S, et al. Breast cancer statistics in Korea in 2017: data from a breast cancer registry. J Breast Cancer. 2020;23:115.
Larsen NB, Rasmussen M, Rasmussen LJ. Nuclear and mitochondrial DNA repair: similar pathways? Mitochondrion. 2005;5:89–108.
Perkhofer L, Gout J, Roger E, de Almeida FK, Simões CB, Wiesmüller L, Seufferlein T, Kleger A. DNA damage repair as a target in pancreatic cancer: state-of-the-art and future perspectives. Gut. 2021;70(3):606–17.
Azim HA, Loutfy SA, Azim HA Jr, Kamal NS, Abdel Fattah NF, Elberry MH, Abdelaziz MR, Abdelsalam M, Aziz M, Shohdy KS, Kassem L. The landscape of BRCA mutations among egyptian women with breast cancer. Oncol Ther. 2023;15:1–8.
Pujol P, Barberis M, Beer P, Friedman E, Piulats JM, Capoluongo ED, et al. Clinical practice guidelines for BRCA1 and BRCA2 genetic testing. Eur J Cancer. 2021;146:30–47.
Kwong A, Chen J, Shin VY, Ho JC, Law FB, Au CH, Chan TL, Ma ES, Ford JM. The importance of analysis of long-range rearrangement of BRCA1 and BRCA2 in genetic diagnosis of familial breast cancer. Cancer Genet. 2015;208(9):448–54.
Sullivan MR, Bernstein KA. RAD-ical new insights into RAD51 regulation. Genes (Basel). 2018;9(12):629.
Qin Z, Li J, Tam B, Sinha S, Zhao B, Bhaskaran SP, Huang T, Wu X, Chian JS, Guo M, Kou SH, Lei H, Zhang L, Wang X, Lagniton PNP, Xiao F, Jiang X, Wang SM. Ethnic-specificity, evolution origin and deleteriousness of Asian BRCA variation revealed by over 7500 BRCA variants derived from Asian population. Int J Cancer. 2023;152(6):1159–73.
Kwong A, Ho CYS, Shin VY, Au CH, Luk WP, Fung LH, Chan TL, Chan KKL, Ngan HYS, Ma ESK. Germline mutations in Chinese ovarian cancer with or without breast cancer. Mol Genet Genomic Med. 2022;10(7): e1940.
Caleca L, Radice P. Refinement of the assignment to the ACMG/AMP BS3 and PS3 criteria of eight BRCA1 variants of uncertain significance by integrating available functional data with protein interaction assays. Front Oncol. 2023;13:1146604.
Cetin B, Wabl CA, Gumusay O. The DNA damaging revolution. Crit Rev Oncol Hematol. 2020;156: 103117.
Ford D, Easton D, Stratton M, Narod S, Goldgar D, Devilee P, et al. Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. Am J Hum Genet. 1998;62:676–89.
Rummel S, Varner E, Shriver CD, Ellsworth RE. Evaluation of BRCA1 mutations in an unselected patient population with triple-negative breast cancer. Breast Cancer Res Treat. 2013;137:119–25.
Ellsworth DL, Turner CE, Ellsworth RE. A review of the hereditary component of triple negative breast cancer: High-and moderate-penetrance breast cancer genes, low-penetrance loci, and the role of nontraditional genetic elements. J Oncol. 2019;25:78–96.
Melki R, Melloul M, Aissaoui S, El-Harroudi T. Increased prevalence of the founder BRCA1 c. 5309G> T and recurrent BRCA2 c. 1310_1313delAAGA mutations in breast cancer families from Northerstern region of Morocco: evidence of geographical specificity and high relevance for genetic counseling. BMC Cancer. 2023;23:339.
Abdallah N, Purrington KS, Tatineni S, Assad H, Petrucelli N, Simon MS. Racial and ethnic variation in BRCA1 and BRCA2 genetic test results among individuals referred for genetic counseling at a large urban comprehensive cancer center. Cancer Causes Control. 2023;34:141–9.
Forbes C, Fayter D, de Kock S, Quek RG. A systematic review of international guidelines and recommendations for the genetic screening, diagnosis, genetic counseling, and treatment of BRCA-mutated breast cancer. Cancer Manage Res. 2019;15:2321–37.
Maqbool M, Bekele F, Fekadu G. Treatment strategies against triple-negative breast cancer: an updated review. Breast Cancer. 2022;15:15–24.
Wang J, Zhao H, Ye L, Li J, Zhang H, Zhang C, et al., Diagnostic and prognostic nomograms for lung metastasis in triple-negative breast cancer. Comput Math Methods Med. 2022
Dieci MV, Del Mastro L, Cinquini M, Montemurro F, Biganzoli L, Cortesi L, et al. Inclusion of platinum agents in neoadjuvant chemotherapy regimens for triple-negative breast cancer patients: development of GRADE (Grades of Recommendation, Assessment, Development and Evaluation) recommendation by the Italian Association of Medical Oncology (AIOM). Cancers. 2019;11:1137.
Al-Showimi M, Al-Yousef N, Alharbi W, Alkhezayem S, Almalik O, Alhusaini H, et al. MicroRNA-126 expression in the peripheral white blood cells of patients with breast and ovarian cancer is a potential biomarker for the early prediction of cancer risk in the carriers of methylated BRCA1. Oncol Lett. 2022;24:1–9.
Biswas T, Efird JT, Prasad S, Jindal C, Walker PR. The survival benefit of neoadjuvant chemotherapy and pCR among patients with advanced stage triple negative breast cancer. Oncotarget. 2017;8: 112712.
Byrski T, Gronwald J, Huzarski T, Grzybowska E, Budryk M, Stawicka M, et al. Pathologic complete response rates in young women with BRCA1-positive breast cancers after neoadjuvant chemotherapy. J Clin Oncol. 2010;28:375–9.
Torrisi R, Zuradelli M, Agostinetto E, Masci G, Losurdo A, De Sanctis R, et al. Platinum salts in the treatment of BRCA-associated breast cancer: a true targeted chemotherapy? Crit Rev Oncol Hematol. 2019;135:66–75.
Sikov WM, Berry DA, Perou CM, Singh B, Cirrincione CT, Tolaney SM, et al. Impact of the addition of carboplatin and/or bevacizumab to neoadjuvant once-per-week paclitaxel followed by dose-dense doxorubicin and cyclophosphamide on pathologic complete response rates in stage II to III triple-negative breast cancer: CALGB 40603 (Alliance). J Clin Oncol. 2015;33:13.
Von Minckwitz G, Schneeweiss A, Loibl S, Salat C, Denkert C, Rezai M, et al. Neoadjuvant carboplatin in patients with triple-negative and HER2-positive early breast cancer (GeparSixto; GBG 66): a randomised phase 2 trial. Lancet Oncol. 2014;15:747–56.
Poggio F, Bruzzone M, Ceppi M, Pondé N, La Valle G, Del Mastro L, et al. Platinum-based neoadjuvant chemotherapy in triple-negative breast cancer: a systematic review and meta-analysis. Ann Oncol. 2018;29:1497–508.
Tutt A, Tovey H, Cheang MCU, Kernaghan S, Kilburn L, Gazinska P, et al. Carboplatin in BRCA1/2-mutated and triple-negative breast cancer BRCAness subgroups: the TNT Trial. Nat Med. 2018;24:628–37.
Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro M, André F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. 2020;31:1623–49.
Herrmann GK, Yin YW. The role of poly(ADP-ribose) polymerase 1 in nuclear and mitochondrial base excision repair. Biomolecules. 2023;13(8):1195.
Mateo J, Lord C, Serra V, Tutt A, Balmaña J, Castroviejo-Bermejo M, et al. A decade of clinical development of PARP inhibitors in perspective. Ann Oncol. 2019;30:1437–47.
Robson M, Im S-A, Senkus E, Xu B, Domchek SM, Masuda N, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377:523–33.
Litton JK, Rugo HS, Ettl J, Hurvitz SA, Gonçalves A, Lee K-H, et al. Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N Engl J Med. 2018;379:753–63.
Rugo HS, Olopade OI, DeMichele A, Yau C, van Veer LJ, Buxton MB, et al. Adaptive randomization of veliparib–carboplatin treatment in breast cancer. N Engl J Med. 2016;375:23–34.
Geyer CE, O'Shaughnessy J, Untch M, Sikov W, Rugo HS, McKee MD, et al. Phase 3 study evaluating efficacy and safety of veliparib (V) plus carboplatin (Cb) or Cb in combination with standard neoadjuvant chemotherapy (NAC) in patients (pts) with early stage triple-negative breast cancer (TNBC). In: American Society of Clinical Oncology; 2017
Litton JK, Scoggins ME, Hess KR, Adrada BE, Murthy RK, Damodaran S, et al. Neoadjuvant talazoparib for patients with operable breast cancer with a germline BRCA pathogenic variant. J Clin Oncol. 2020;38:388.
Fasching P, Link T, Hauke J, Seither F, Jackisch C, Klare P, et al. Neoadjuvant paclitaxel/olaparib in comparison to paclitaxel/carboplatinum in patients with HER2-negative breast cancer and homologous recombination deficiency (GeparOLA study). Ann Oncol. 2021;32:49–57.
Kalra M, Tong Y, Jones DR, Walsh T, Danso MA, Ma CX, et al. Cisplatin+/− rucaparib after preoperative chemotherapy in patients with triple-negative or BRCA mutated breast cancer. NPJ Breast Cancer. 2021;7:29.
Tutt A, Stephens C, Frewer P, Pierce A, Rhee J, So K, et al. VIOLETTE: A randomized phase II study to assess DNA damage response inhibitors in combination with olaparib (Ola) vs Ola monotherapy in patients (pts) with metastatic, triple-negative breast cancer (TNBC) stratified by alterations in homologous recombination repair (HRR)-related genes. In.: American Society of Clinical Oncology; 2018.
Kirova YM, Loirat D, Berger F, Rodrigues M, Bazire L, Pierga J-Y, et al. Radioparp: A phase I of olaparib with radiation therapy (RT) in patients with inflammatory, locoregionally advanced or metastatic triple-negative breast cancer (TNBC) or patient with operated TNBC with residual disease—Preliminary results. In.: American Society of Clinical Oncology; 2020.
Wang X, Collet L, Rediti M, Debien V, De Caluwé A, Venet D, et al. Predictive biomarkers for response to immunotherapy in triple negative breast cancer: promises and challenges. J Clin Med. 2023;12:953.
Sadreddini S, Baradaran B, Aghebati-Maleki A, Sadreddini S, Shanehbandi D, Fotouhi A, et al. Immune checkpoint blockade opens a new way to cancer immunotherapy. J Cell Physiol. 2019;234:8541–9.
Kuske M, Haist M, Jung T, Grabbe S, Bros M. Immunomodulatory properties of immune checkpoint inhibitors-more than boosting t-cell responses? Cancers (Basel). 2022;14(7):1710.
Kumar S, Singh SK, Srivastava P, Suresh S, Rana B, Rana A. Interplay between MAP kinases and tumor microenvironment: opportunity for immunotherapy in pancreatic cancer. Adv Cancer Res. 2023;159:113–43.
Sabatier R, Finetti P, Mamessier E, Adelaide J, Chaffanet M, Ali H, et al. Prognostic and predictive value of PDL1 expression in breast cancer. Oncotarget. 2015; 6 (7): 5449–64. Largest retrospective study analysing the mRNA expression of PD-L1 in.5.
Ni Y, Tsang JY, Shao Y, Poon IK, Tam F, Shea K-H, et al. Combining analysis of tumor-infiltrating lymphocytes (TIL) and PD-L1 refined the prognostication of breast cancer subtypes. Oncologist. 2022;27:e313–27.
Yuan Y, Lee JS, Yost SE, Frankel PH, Ruel C, Egelston CA, et al. A phase II clinical trial of pembrolizumab and enobosarm in patients with androgen receptor-positive metastatic triple-negative breast cancer. Oncologist. 2021;26:99-e217.
Sood R, Kumar S, Laroiya I, Khare S, Das A, Singh G, et al. Assessment of PD-L1 expression and tumor-infiltrating lymphocytes (TILs) across molecular subtypes of triple-negative breast cancer. Breast J. 2020;26:2424–7.
Li M, Li A, Zhou S, Xu Y, Xiao Y, Bi R, et al. Heterogeneity of PD-L1 expression in primary tumors and paired lymph node metastases of triple negative breast cancer. BMC Cancer. 2018;18:1–9.
Carter JM, Polley MYC, Leon-Ferre RA, Sinnwell J, Thompson KJ, Wang X, et al. Characteristics and spatially defined immune (micro) landscapes of early-stage PD-L1-positive Triple-negative Breast Cancer. Clin Cancer Res. 2021;27:5628–37.
Bertucci F, Gonçalves A. Immunotherapy in breast cancer: the emerging role of PD-1 and PD-L1. Curr Oncol Rep. 2017;19:1–11.
Fabozzi A, Della Sala F, di Gennaro M, Solimando N, Pagliuca M, Borzacchiello A. Polymer based nanoparticles for biomedical applications by microfluidic techniques: from design to biological evaluation. Polym Chem. 2021;12:6667–87. https://doi.org/10.1039/d1py01077h.
Marra A, Viale G, Curigliano G. Recent advances in triple negative breast cancer: the immunotherapy era. BMC Med. 2019;17:1–9.
Schmid P, Rugo HS, Adams S, Schneeweiss A, Barrios CH, Iwata H, et al. Atezolizumab plus nab-paclitaxel as first-line treatment for unresectable, locally advanced or metastatic triple-negative breast cancer (IMpassion130): updated efficacy results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2020;21:44–59.
Adams S, Schmid P, Rugo H, Winer E, Loirat D, Awada A, et al. Pembrolizumab monotherapy for previously treated metastatic triple-negative breast cancer: cohort A of the phase II KEYNOTE-086 study. Ann Oncol. 2019;30:397–404.
Nanda R, Chow LQ, Dees EC, Berger R, Gupta S, Geva R, et al. Pembrolizumab in patients with advanced triple-negative breast cancer: phase Ib KEYNOTE-012 study. J Clin Oncol. 2016;34:2460.
Gianni L, Huang C-S, Egle D, Bermejo B, Zamagni C, Thill M, et al. Pathologic complete response (pCR) to neoadjuvant treatment with or without atezolizumab in triple-negative, early high-risk and locally advanced breast cancer: NeoTRIP Michelangelo randomized study. Ann Oncol. 2022;33:534–43.
Rugo HS, Loi S, Adams S, Schmid P, Schneeweiss A, Barrios CH, et al. Performance of PD-L1 immunohistochemistry (IHC) assays in unresectable locally advanced or metastatic triple-negative breast cancer (mTNBC): Post-hoc analysis of IMpassion130. Ann Oncol. 2019;30:v858–9.
Paré L, Pascual T, Seguí E, Teixidó C, Gonzalez-Cao M, Galván P, et al. Association between PD1 mRNA and response to anti-PD1 monotherapy across multiple cancer types. Ann Oncol. 2018;29:2121–8.
Bianchini G, Huang C, Egle D, Bermejo B, Zamagni C, Thill M, et al. LBA13 Tumour infiltrating lymphocytes (TILs), PD-L1 expression and their dynamics in the NeoTRIPaPDL1 trial. Ann Oncol. 2020;31:S1145–6.
Lehmann BD, Colaprico A, Silva TC, Chen J, An H, Ban Y, et al. Multi-omics analysis identifies therapeutic vulnerabilities in triple-negative breast cancer subtypes. Nat Commun. 2021;12:6276.
Balko JM, Schwarz LJ, Luo N, Estrada MV, Giltnane JM, Dávila-González D, et al. (2016) Triple-negative breast cancers with amplification of JAK2 at the 9p24 locus demonstrate JAK2-specific dependence. Sci Transl Med. 2016;8:334.
Stanton SE, Adams S, Disis ML. Variation in the incidence and magnitude of tumor-infiltrating lymphocytes in breast cancer subtypes: a systematic review. JAMA Oncol. 2016;2:1354–60.
Savas P, Salgado R, Denkert C, Sotiriou C, Darcy PK, Smyth MJ, et al. Clinical relevance of host immunity in breast cancer: from TILs to the clinic. Nat Rev Clin Oncol. 2016;13:228–41.
Bareche Y, Buisseret L, Gruosso T, Girard E, Venet D, Dupont F, et al. Unraveling triple-negative breast cancer tumor microenvironment heterogeneity: towards an optimized treatment approach. JNCI. 2020;112:708–19.
Ochi T, Bianchini G, Ando M, Nozaki F, Kobayashi D, Criscitiello C, et al. Predictive and prognostic value of stromal tumour-infiltrating lymphocytes before and after neoadjuvant therapy in triple negative and HER2-positive breast cancer. Eur J Cancer. 2019;118:41–8.
Gao ZH, Li CX, Liu M, Jiang JY. Predictive and prognostic role of tumour-infiltrating lymphocytes in breast cancer patients with different molecular subtypes: a meta-analysis. BMC Cancer. 2020;20:1–14.
Denkert C, von Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE, et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018;19:40–50.
Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol. 2014;32:2959.
Manzo E, Fioretto L, Gallo C, Ziaco M, Nuzzo G, D’Ippolito G, et al. Preparation, supramolecular aggregation and immunological activity of the bona fide vaccine adjuvant sulfavant s. Mar Drugs. 2020;18:451.
Loi S, Drubay D, Adams S, Pruneri G, Francis PA, Lacroix-Triki M, et al. Tumor-infiltrating lymphocytes and prognosis: a pooled individual patient analysis of early-stage triple-negative breast cancers. J Clin Oncol. 2019;37:559.
Park J, Jonas S, Bataillon G, Criscitiello C, Salgado R, Loi S, et al. Prognostic value of tumor-infiltrating lymphocytes in patients with early-stage triple-negative breast cancers (TNBC) who did not receive adjuvant chemotherapy. Ann Oncol. 2019;30:1941–9.
Loi S, Michiels S, Adams S, Loibl S, Budczies J, Denkert C, et al. The journey of tumor-infiltrating lymphocytes as a biomarker in breast cancer: clinical utility in an era of checkpoint inhibition. Ann Oncol. 2021;32:1236–44.
Sasaki R, Horimoto Y, Yanai Y, Kurisaki-Arakawa A, Arakawa A, Nakai K, et al. Molecular characteristics of lymphocyte-predominant triple-negative breast cancer. Anticancer Res. 2021;41:2133–40.
Criscitiello C, Bayar M, Curigliano G, Symmans F, Desmedt C, Bonnefoi H, et al. A gene signature to predict high tumor-infiltrating lymphocytes after neoadjuvant chemotherapy and outcome in patients with triple-negative breast cancer. Ann Oncol. 2018;29:162–9.
Fabozzi A, Della Sala F, di Gennaro M, Borzacchiello A. Synthesis of hyaluronic acid core–shell nanoparticles via simple microfluidic-assisted nanoprecipitation method for active tumor targeting. New J Chem. 2022;46:19763–72.
Loi S, Adams S, Schmid P, Cortés J, Cescon D, Winer E, et al. Relationship between tumor infiltrating lymphocyte (TIL) levels and response to pembrolizumab (pembro) in metastatic triple-negative breast cancer (mTNBC): results from KEYNOTE-086. Ann Oncol. 2017;28: v608.
Loi S, Schmid P, Aktan G, Karantza V, Salgado R. Relationship between tumor infiltrating lymphocytes (TILs) and response to pembrolizumab (pembro)+ chemotherapy (CT) as neoadjuvant treatment (NAT) for triple-negative breast cancer (TNBC): phase Ib KEYNOTE-173 trial. Ann Oncol. 2019;30:32.
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio I, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30:1194–220.
Sporikova Z, Koudelakova V, Trojanec R, Hajduch M. Genetic markers in triple-negative breast cancer. Clin Breast Cancer. 2018;18:e841–50.
Jin J, He J, Li X, Ni X, Jin X. The role of ubiquitination and deubiquitination in PI3K/AKT/mTOR pathway: a potential target for cancer therapy. Gene. 2023;889: 147807.
Bang J, Jun M, Lee S, Moon H, Ro SW. Targeting EGFR/PI3K/AKT/mTOR signaling in hepatocellular carcinoma. Pharmaceutics. 2023;15(8):2130.
Álvarez-Garcia V, Tawil Y, Wise HM, Leslie NR. Mechanisms of PTEN loss in cancer: It’s all about diversity. Semin Cancer Biol. 2019;59:66–79.
Zhang H, Cohen AL, Krishnakumar S, Wapnir IL, Veeriah S, Deng G, et al. Patient-derived xenografts of triple-negative breast cancer reproduce molecular features of patient tumors and respond to mTOR inhibition. Breast Cancer Res. 2014;16:1–16.
Martín M, Chan A, Dirix L, O’Shaughnessy J, Hegg R, Manikhas A, et al. A randomized adaptive phase II/III study of buparlisib, a pan-class I PI3K inhibitor, combined with paclitaxel for the treatment of HER2–advanced breast cancer (BELLE-4). Ann Oncol. 2017;28:313–20.
Kim S-B, Dent R, Im S-A, Espié M, Blau S, Tan AR, et al. Ipatasertib plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer (LOTUS): a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2017;18:1360–72.
Schmid P, Abraham J, Chan S, Wheatley D, Brunt AM, Nemsadze G, et al. Capivasertib plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer: the PAKT trial. J Clin Oncol. 2020;38:423–33.
Lehmann BD, Abramson VG, Sanders ME, Mayer EL, Haddad TC, Nanda R, et al. TBCRC 032 IB/II multicenter study: molecular insights to AR antagonist and PI3K inhibitor efficacy in patients with AR+ metastatic triple-negative breast cancer. Clin Cancer Res. 2020;26:2111–23.
Sussman D, Smith LM, Anderson ME, Duniho S, Hunter JH, Kostner H, et al. SGN–LIV1A: a novel antibody–drug conjugate targeting LIV-1 for the treatment of metastatic breast cancer. Mol Cancer Ther. 2014;13:2991–3000.
Saravanan R, Balasubramanian V, Swaroop Balamurugan SS, Ezhil I, Afnaan Z, John J, et al. Zinc transporter LIV1: A promising cell surface target for triple negative breast cancer. J Cell Physiol. 2022;237:4132–56.
Fabozzi A, Della Sala F, di Gennaro M, Barretta M, Longobardo G, Solimando N, et al. Design of functional nanoparticles by microfluidic platforms as advanced drug delivery systems for cancer therapy. Lab Chip. 2023;23:1389–409.
Vessella G, Casillo A, Fabozzi A, Traboni S, Iadonisi A, Corsaro MM, et al. Synthesis of the tetrasaccharide repeating unit of the cryoprotectant capsular polysaccharide from Colwellia psychrerythraea 34H. Org Biomol Chem. 2019;17:3129–40.
Shi D, Li Y, Liang X, Chen L. Cost-effectiveness of sacituzumab govitecan in hormone receptor-positive/human epidermal growth factor receptor 2-negative metastatic breast cancer. Front Oncol. 2023;13:1162360.
Goldenberg DM, Stein R, Sharkey RM. The emergence of trophoblast cell-surface antigen 2 (TROP-2) as a novel cancer target. Oncotarget. 2018;9:28989.
Shastry M, Jacob S, Rugo HS, Hamilton E. Antibody-drug conjugates targeting TROP-2: clinical development in metastatic breast cancer. The Breast. 2022;66:169–77.
Li J, Goh EL, He J, Li Y, Fan Z, Yu Z, et al. Emerging intrinsic therapeutic targets for metastatic breast cancer. Biology. 2023;12:697.
McGuinness JE, Kalinsky K. Antibody-drug conjugates in metastatic triple negative breast cancer: a spotlight on sacituzumab govitecan, ladiratuzumab vedotin, and trastuzumab deruxtecan. Expert Opin Biol Ther. 2021;21:903–13.
Fabozzi A, Barretta M, Valente T, Borzacchiello A. Preparation and optimization of hyaluronic acid decorated irinotecan-loaded poly (lactic-co-glycolic acid) nanoparticles by microfluidics for cancer therapy applications. Colloids Surf A. 2023;15:131790.
Bardia A, Mayer IA, Diamond JR, Moroose RL, Isakoff SJ, Starodub AN, et al. Efficacy and safety of anti-trop-2 antibody drug conjugate sacituzumab govitecan (IMMU-132) in heavily pretreated patients with metastatic triple-negative breast cancer. J Clin Oncol. 2017;35:2141.
Bardia A, Mayer IA, Vahdat LT, Tolaney SM, Isakoff SJ, Diamond JR, et al. Sacituzumab govitecan-hziy in refractory metastatic triple-negative breast cancer. N Engl J Med. 2019;380:741–51.
Bardia A, Tolaney S, Loirat D, Punie K, Oliveira M, Rugo H, et al. LBA17 ASCENT: a randomized phase III study of sacituzumab govitecan (SG) vs treatment of physician’s choice (TPC) in patients (pts) with previously treated metastatic triple-negative breast cancer (mTNBC). Ann Oncol. 2020;31:S1149–50.
Rose AA, Grosset A-A, Dong Z, Russo C, MacDonald PA, Bertos NR, et al. Glycoprotein nonmetastatic B is an independent prognostic indicator of recurrence and a novel therapeutic target in breast cancer. Clin Cancer Res. 2010;16:2147–56.
Yao L, Hao Q, Wang M, Chen Y, Cao H, Zhang Q, Yu K, Jiang Y, Shao Z, Zhou X, Xu Y. KLHL29-mediated DDX3X degradation promotes chemosensitivity by abrogating cell cycle checkpoint in triple-negative breast cancer. Oncogene. 2023. https://doi.org/10.1038/s41388-023-02858-5.
Byers HA, Brooks AN, Vangala JR, Grible JM, Feygin A, Clevenger CV, Harrell JC, Radhakrishnan SK. Evaluation of the NRF1-proteasome axis as a therapeutic target in breast cancer. Sci Rep. 2023;13(1):15843. https://doi.org/10.1038/s41598-023-43121-x.
Cen S, Peng X, Deng J, Jin H, Deng Z, Lin X, Zhu DI, Jin M, Zhu Y, Zhang P, Luo Y, Huang H. The role of AFAP1-AS1 in mitotic catastrophe and metastasis of triple-negative breast cancer cells by activating the PLK1 signaling pathway. Oncol Res. 2023;31(3):375–88. https://doi.org/10.32604/or.2023.028256.
Raute K, Strietz J, Parigiani MA, Andrieux G, Thomas OS, Kistner KM, Zintchenko M, Aichele P, Hofmann M, Zhou H, Weber W, Boerries M, Swamy M, Maurer J, Minguet S. Breast cancer stem cell-derived tumors escape from γδ T-cell immunosurveillance in vivo by modulating γδ T-cell ligands. Cancer Immunol Res. 2023;11(6):810–29. https://doi.org/10.1158/2326-6066.CIR-22-0296.
Psilopatis I, Mantzari A, Vrettou K, Theocharis S. The role of patient-derived organoids in triple-negative breast cancer drug screening. Biomedicines. 2023;11(3):773. https://doi.org/10.3390/biomedicines11030773.
Usary J, Darr DB, Pfefferle AD, Perou CM. Overview of genetically engineered mouse models of distinct breast cancer subtypes. Curr Protoc Pharmacol. 2016;72:14. https://doi.org/10.1002/0471141755.ph1438s72.
Holen I, Speirs V, Morrissey B, Blyth K. In vivo models in breast cancer research: progress, challenges and future directions. Dis Model Mech. 2017;10(4):359–71. https://doi.org/10.1242/dmm.028274.
Doha ZO, Wang X, Calistri NL, Eng J, Daniel CJ, Ternes L, Kim EN, Pelz C, Munks M, Betts C, Kwon S, Bucher E, Li X, Waugh T, Tatarova Z, Blumberg D, Ko A, Kirchberger N, Pietenpol JA, Sanders ME, Langer EM, Dai MS, Mills G, Chin K, Chang YH, Coussens LM, Gray JW, Heiser LM, Sears RC. MYC deregulation and PTEN loss model tumor and stromal heterogeneity of aggressive triple-negative breast cancer. Nat Commun. 2023;14(1):5665. https://doi.org/10.1038/s41467-023-40841-6.
Houthuijzen JM, de Bruijn R, van der Burg E, Drenth AP, Wientjens E, Filipovic T, Bullock E, Brambillasca CS, Pulver EM, Nieuwland M, de Rink I, van Diepen F, Klarenbeek S, Kerkhoven R, Brunton VG, Scheele CLGJ, Boelens MC, Jonkers J. CD26-negative and CD26-positive tissue-resident fibroblasts contribute to functionally distinct CAF subpopulations in breast cancer. Nat Commun. 2023;14(1):183. https://doi.org/10.1038/s41467-023-35793-w.
Acknowledgements
We thank Daniela Capobianco for her technical editing and writing assistance. We also acknowledge the “Lega Italiana per la Lotta contro I Tumori (LILT)-sezione di Napoli” and the TRIAL scientific association (CF: 92088670622) for their invaluable and unwavering collaboration on this work.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: MC and AO; methodology; FP, VC, and Marco Cascella; software: Mariachiara Santorsola; validation: FF, VG, AB, and FS; investigation: MC and AO; resources: OG and GS; data curation: OG, LL, AF, and GS; writing—original draft preparation: all authors; writing—review and editing: AO, AF, and MC. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Institutional review board
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Capuozzo, M., Celotto, V., Santorsola, M. et al. Emerging treatment approaches for triple-negative breast cancer. Med Oncol 41, 5 (2024). https://doi.org/10.1007/s12032-023-02257-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-023-02257-6