Abstract
Purpose
Distant metastasis develops in approximately one-third of patients with colorectal cancer (CRC) who undergo radical surgery, and colorectal liver metastasis (CRLM) is the most common form of distant metastasis in CRC. Hepatectomy is the only potentially curative treatment for CRLM, but few patients with metastatic CRC meet the criteria for this radical resection, and the 5-year survival rate is poor. Identifying risk factors for CRLM is critical. Non-alcoholic fatty liver disease (NAFLD) is an independent risk factor for CRC. However, the effect of NAFLD on CRC liver metastasis after radical surgery remains unclear. Therefore, we examined the impact of NAFLD-associated hepatic fibrosis on liver metastasis after radical surgery for CRC.
Methods
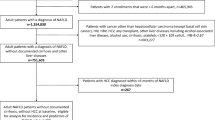
We retrospectively analyzed data from 388 patients who underwent curative surgery for CRC at our hospital between April 2008 and March 2015. The patients’ clinical results, surgical procedures, postoperative course, and pathological and survival data were collected from the hospital records. The NAFLD fibrosis score was calculated and used to divide the patients into two groups (NAFLD and non-NAFLD).
Results
Recurrence was observed in 83/388 (21.4%) patients after a mean follow-up of 65.6 ± 15.1 months. Twenty-five patients had liver metastasis: 8 in the NAFLD group (8/45; 17.8%) and 17 in the non-NALFD group (17/343; 5.0%) (p = 0.004). Liver metastasis-free survival was significantly worse in the NAFLD than non-NAFLD group (p < 0.001). NAFLD and cancer stage were independent risk factors for liver metastasis recurrence.
Conclusion
NAFLD may be a risk factor for liver metastasis in patients with CRC who undergo curative surgery.

Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Manfredi S, Lepage C, Hatem C, Coatmeur O, Faivre J, Bouvier AM. Epidemiology and management of liver metastases from colorectal cancer. Ann Surg. 2006;244:254–9. https://doi.org/10.1097/01.sla.0000217629.94941.cf.
Eichler K, Dufas T, Hammerstingl R, Gruber-Rouh T, Vogl TJ, Zangos S. Hepatic arterial infusion with irinotecan in patients with liver metastases of colorectal cancer: results of an extended phase I study. Chemotherapy. 2013;59:66–73. https://doi.org/10.1159/000348579.
Waisberg J, Ivankovics IG. Liver-first approach of colorectal cancer with synchronous hepatic metastases: a reverse strategy. World J Hepatol. 2015;7:1444–9. https://doi.org/10.4254/wjh.v7.i11.1444.
Wanebo HJ, Chu QD, Avradopoulos KA, Vezeridis MP. Current perspectives on repeat hepatic resection for colorectal carcinoma: a review. Surgery. 1996;119:361–71. https://doi.org/10.1016/s0039-6060(96)80133-4.
Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, Swain MG, Congly SE, Kaplan GG, Shaheen AA. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2022;7:851–61. https://doi.org/10.1016/S2468-1253(22)00165-0.
Marchesini G, Babini M. Nonalcoholic fatty liver disease and the metabolic syndrome. Minerva Cardioangiol. 2006;54:229–39.
van der Bilt JD, Kranenburg O, Borren A, van Hillegersberg R, Borel Rinkes IH. Ageing and hepatic steatosis exacerbate ischemia/reperfusion-accelerated outgrowth of colorectal micrometastases. Ann Surg Oncol. 2008;15:1392–8. https://doi.org/10.1245/s10434-007-9758-0.
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–76. https://doi.org/10.1053/j.gastro.2007.04.061.
Lv Y, Zhang HJ. Effect of non-alcoholic fatty liver disease on the risk of synchronous liver metastasis: analysis of 451 consecutive patients of newly diagnosed colorectal cancer. Front Oncol. 2020;10:251. https://doi.org/10.3389/fonc.2020.00251.
Mantovani A, Dauriz M, Byrne CD, Lonardo A, Zoppini G, Bonora E, Targher G. Association between nonalcoholic fatty liver disease and colorectal tumours in asymptomatic adults undergoing screening colonoscopy: a systematic review and meta-analysis. Metabolism. 2018;87:1–12. https://doi.org/10.1016/j.metabol.2018.06.004.
Chen J, Bian D, Zang S, Yang Z, Tian G, Luo Y, Yang J, Xu B, Shi J. The association between nonalcoholic fatty liver disease and risk of colorectal adenoma and cancer incident and recurrence: a meta-analysis of observational studies. Expert Rev Gastroenterol Hepatol. 2019;13:385–95. https://doi.org/10.1080/17474124.2019.1580143.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL. Trotti A (2010) AJCC cancer staging manual. 7th ed. France: Springer; 2010.
Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, Enders F, Saksena S, Burt AD, Bida JP, Lindor K, Sanderson SO, Lenzi M, Adams LA, Kench J, Therneau TM, Day CP. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–54. https://doi.org/10.1002/hep.21496.
Lieber MM. The rare occurrence of metastatic carcinoma in the cirrhotic liver. Am J Med Sci. 1957;233:145–52. https://doi.org/10.1097/00000441-195702000-00005.
Langley RR, Fidler IJ. The seed and soil hypothesis revisited–the role of tumor-stroma interactions in metastasis to different organs. Int J Cancer. 2011;128:2527–35. https://doi.org/10.1002/ijc.26031.
VanSaun MN, Lee IK, Washington MK, Matrisian L, Gorden DL. High fat diet induced hepatic steatosis establishes a permissive microenvironment for colorectal metastases and promotes primary dysplasia in a murine model. Am J Pathol. 2009;175:355–64. https://doi.org/10.2353/ajpath.2009.080703.
Wang Z, Kim SY, Tu W, Kim J, Xu A, Yang YM, Matsuda M, Reolizo L, Tsuchiya T, Billet S, Gangi A, Noureddin M, Falk BA, Kim S, Fan W, Tighiouart M, You S, Lewis MS, Pandol SJ, Vizio DD, Merchant A, Posadas EM, Bhowmick NA, Lu SC, Seki E. Extracellular vesicles in fatty liver promote a metastatic tumor microenvironment. Cell Metab. 2023;35:1209–26. https://doi.org/10.1016/j.cmet.
Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut. 2017;66:1138–53. https://doi.org/10.1136/gutjnl-2017-313884.
Chakraborty D, Wang J. Nonalcoholic fatty liver disease and colorectal cancer: correlation and missing links. Life Sci. 2020;262:118507. https://doi.org/10.1016/j.lfs.2020.118507.
Rector RS, Thyfault JP, Wei Y, Ibdah JA. Non-alcoholic fatty liver disease and the metabolic syndrome: an update. World J Gastroenterol. 2008;14:185–92. https://doi.org/10.3748/wjg.14.185.
Goyal A, Terry MB, Jin Z, Siegel AB. C-reactive protein and colorectal cancer mortality in U.S. adults. Cancer Epidemiol Biomarkers Prev. 2014;23:1609–18. https://doi.org/10.1158/1055-9965.EPI-13-0577.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, Harrison SA, Brunt EM, Sanyal AJ. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–57. https://doi.org/10.1002/hep.29367.
Murono K, Kitayama J, Tsuno NH, Nozawa H, Kawai K, Sunami E, Akahane M, Watanabe T. Hepatic steatosis is associated with lower incidence of liver metastasis from colorectal cancer. Int J Colorectal Dis. 2013;28:1065–72. https://doi.org/10.1007/s00384-013-1656-2.
Acknowledgements
We thank Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript. A preprint version is available (https://doi.org/https://doi.org/10.21203/rs.3.rs-2145570/v1).
Author information
Authors and Affiliations
Contributions
Takashi M and Hiroyuki T designed the study. Takashi M, Yuki S, SM, Yuta S, Hozumi T, TN, HN, AH, DK, HF, and NU collected and analyzed the data. Takashi M wrote the paper. Hiroyuki T revised the paper critically. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study protocol was approved by the Institutional Review Committee for the Department of General and Digestive Surgery, Kanazawa Medical University Hospital, Ishikawa, Japan (No. I457), and the study was conducted in accordance with the ethical criteria outlined in the World Medical Association Declaration of Helsinki.
Consent to Participate
Written informed consent to participate in this study was obtained from all patients.
Consent for Publication
Written informed consent for the publication of this study was obtained from all patients.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miyata, T., Shinden, Y., Motoyama, S. et al. Non-Alcoholic Fatty Liver Disease May Be a Risk Factor for Liver Metastasis After Radical Surgery for Colorectal Cancer: A Retrospective Study. J Gastrointest Canc (2024). https://doi.org/10.1007/s12029-024-01042-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s12029-024-01042-6