Abstract
Purpose
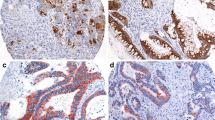
Colon mucinous carcinomas (MUCs) have two morphological patterns: (i) glands lined by mucinous epithelium with direct contact to the stroma (FIX) and (ii) carcinoma cells floating in mucin (FLO). In this study, we evaluated the prognostic value of these patterns.
Methods
Digital images were captured from the 38 MUC’s tissue sections. A grid with 140 points was laid over the computer screen. Totally, 100 points, falling on tumor cells floating in mucin (FLO patterned cells) or on cells contacting stroma (FIX patterned cells), were counted. Tumors were grouped according to the median value of the FIX patterned cells. Cases with more than this value were grouped as FIX and less were grouped as FLO cases. The prognostic value of FIX and FLO pattern was evaluated.
Results
The median for FIX patterned cells was 66%, and the cases with lower values than this were grouped as FLO (N = 18; 47.37%), while the rest were grouped as FIX cases. There was no significant difference between FIX and FLO cases for overall survival cases (p = 0.167). For FIX cases, 62.7 and 51.3% of the patients were alive at second and third years, while this was 78.9 and 72.4% for the FLO group, respectively.
Conclusions
This is the first study using a quantitative methodology depending on count pointing to evaluate FIX/FLO feature of MUCs to the best of our knowledge, although we could not observed any prognostic and clinicopathologic relationship statistically. This distinctive feature should be studied in larger cohorts with prognostic information, with a quantitative method, like the one that was applied in this study, in order to achieve strict conclusions.



Similar content being viewed by others
References
Li D, Semba S, Wu M, Yokozaki H. Molecular pathological subclassification of mucinous adenocarcinoma of the colorectum. Pathol Int. 2005;55(12):766–74. https://doi.org/10.1111/j.1440-1827.2005.01903.x.
Song W, Wu SJ, He YL, Cai SR, Zhang CH, Zhang XH, et al. Clinicopathologic features and survival of patients with colorectal mucinous, signet-ring cell or non-mucinous adenocarcinoma: experience at an institution in southern China. Chin Med J. 2009;122(13):1486–91.
Safaee A, Moghimi-Dehkordi B, Fatemi SR, Ghiasi S, Nemati-Malek F, Zali MR. Characteristics of colorectal mucinous adenocarcinoma in Iran. Asian Pac J Cancer Prev : APJCP. 2010;11(5):1373–5.
Catalano V, Loupakis F, Graziano F, Bisonni R, Torresi U, Vincenzi B, et al. Prognosis of mucinous histology for patients with radically resected stage II and III colon cancer. Ann Oncol : Off J Eur Soc Med Oncol / ESMO. 2012;23(1):135–41. https://doi.org/10.1093/annonc/mdr062.
Bosman FT, Carneiro FT, World Health Organization., International Agency for Research on Cancer (IARC). WHO classification of tumours of the digestive system. World Health Organization classification of tumours, vol. 2. 4th ed. Lyon: IARC; 2010.
Yamaguchi T, Taniguchi H, Fujita S, Sekine S, Yamamoto S, Akasu T, et al. Clinicopathological characteristics and prognostic factors of advanced colorectal mucinous adenocarcinoma. Histopathology. 2012;61(2):162–9. https://doi.org/10.1111/j.1365-2559.2012.04235.x.
Kakar S, Aksoy S, Burgart LJ, Smyrk TC. Mucinous carcinoma of the colon: correlation of loss of mismatch repair enzymes with clinicopathologic features and survival. Mod Pathol : Off J U S Can Acad Pathol Inc. 2004;17(6):696–700. https://doi.org/10.1038/modpathol.3800093.
Kanemitsu Y, Kato T, Hirai T, Yasui K, Morimoto T, Shimizu Y, et al. Survival after curative resection for mucinous adenocarcinoma of the colorectum. Dis Colon rectum. 2003;46(2):160–7. https://doi.org/10.1097/01.DCR.0000044721.76711.6D.
Kubota K, Akasu T, Fujita S, Sugihara K, Moriya Y, Yamamoto S. Clinical and pathological prognostic indicators with colorectal mucinous carcinomas. Hepato-Gastroenterology. 2004;51(55):142–6.
Akino F, Mitomi H, Nakamura T, Ohtani Y, Ichinoe M, Okayasu I. High apoptotic activity and low epithelial cell proliferation with underexpression of p21(WAF1/CIP1) and p27Kip1 of mucinous carcinomas of the colorectum: comparison with well-differentiated type. Am J Clin Pathol. 2002;117(6):908–15. https://doi.org/10.1309/D4QM-379U-E8J2-9R1M.
Wu CS, Tung SY, Chen PC, Kuo YC. Clinicopathological study of colorectal mucinous carcinoma in Taiwan: a multivariate analysis. J Gastroenterol Hepatol. 1996;11(1):77–81. https://doi.org/10.1111/j.1440-1746.1996.tb00014.x.
Mekenkamp LJ, Heesterbeek KJ, Koopman M, Tol J, Teerenstra S, Venderbosch S, et al. Mucinous adenocarcinomas: poor prognosis in metastatic colorectal cancer. Eur J Cancer. 2012;48(4):501–9. https://doi.org/10.1016/j.ejca.2011.12.004.
Chiang JM, Yeh CY, Changchien CR, Chen JS, Tang R, Chen JR. Mucinous adenocarcinoma showing different clinicopathological and molecular characteristics in relation to different colorectal cancer subgroups. Int J Color Dis. 2010;25(8):941–7. https://doi.org/10.1007/s00384-010-0958-x.
Zhang W, Huang P. Cancer-stromal interactions: role in cell survival, metabolism and drug sensitivity. Cancer Biol Ther. 2011;11(2):150–6. https://doi.org/10.4161/cbt.11.2.14623.
Yakirevich E, Sabo E, Klorin G, Alos L, Cardesa A, Ellis GL, et al. Primary mucin-producing tumours of the salivary glands: a clinicopathological and morphometric study. Histopathology. 2010;57(3):395–409. https://doi.org/10.1111/j.1365-2559.2010.03639.x.
Jass JR, Sobin LH, Morson BC, World Health Organization. (1989) Histological typing of intestinal tumours. International histological classification of tumours (Unnumbered), 2nd edn. Springer-Verlag, Berlin; New York.
Ikeda S, Shimizu Y, Fujimori M, Ishizaki Y, Kurihara T, Ojima Y, et al. Immunohistochemical and mutational analyses of beta-catenin, Ki-ras, and p53 in two subtypes of colorectal mucinous carcinoma. Clin Cancer Res : Off J Am Assoc Cancer Res. 2003;9(15):5660–5.
Leopoldo S, Lorena B, Cinzia A, Gabriella DC, Angela Luciana B, Renato C, et al. Two subtypes of mucinous adenocarcinoma of the colorectum: clinicopathological and genetic features. Ann Surg Oncol. 2008;15(5):1429–39. https://doi.org/10.1245/s10434-007-9757-1.
Purdie CA, Piris J. Histopathological grade, mucinous differentiation and DNA ploidy in relation to prognosis in colorectal carcinoma. Histopathology. 2000;36(2):121–6. https://doi.org/10.1111/j.1365-2559.2000.00826.x.
Compton CC, Fielding LP, Burgart LJ, Conley B, Cooper HS, Hamilton SR, et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 2000;124(7):979–94. https://doi.org/10.1043/0003-9985(2000)124<0979:PFICC>2.0.CO;2.
Compton C, Fenoglio-Preiser CM, Pettigrew N, Fielding LP. American Joint Committee on Cancer prognostic factors consensus conference: colorectal working group. Cancer. 2000;88(7):1739–57. https://doi.org/10.1002/(SICI)1097-0142(20000401)88:7<1739::AID-CNCR30>3.0.CO;2-T.
Catalano V, Loupakis F, Graziano F, Torresi U, Bisonni R, Mari D, et al. Mucinous histology predicts for poor response rate and overall survival of patients with colorectal cancer and treated with first-line oxaliplatin- and/or irinotecan-based chemotherapy. Br J Cancer. 2009;100(6):881–7. https://doi.org/10.1038/sj.bjc.6604955.
Negri FV, Wotherspoon A, Cunningham D, Norman AR, Chong G, Ross PJ. Mucinous histology predicts for reduced fluorouracil responsiveness and survival in advanced colorectal cancer. Ann Oncol\ : Off J Eur Soc Med Oncol / ESMO. 2005;16(8):1305–10. https://doi.org/10.1093/annonc/mdi244.
Papadopoulos VN, Michalopoulos A, Netta S, Basdanis G, Paramythiotis D, Zatagias A, et al. Prognostic significance of mucinous component in colorectal carcinoma. Tech Coloproctol. 2004;8(Suppl 1):s123–5. https://doi.org/10.1007/s10151-004-0131-z.
Courrech Staal EF, Wouters MW, van Sandick JW, Takkenberg MM, Smit VT, Junggeburt JM, et al. The stromal part of adenocarcinomas of the oesophagus: does it conceal targets for therapy? Eur J Cancer. 2010;46(4):720–8. https://doi.org/10.1016/j.ejca.2009.12.006.
Mesker WE, Junggeburt JM, Szuhai K, de Heer P, Morreau H, Tanke HJ, et al. The carcinoma-stromal ratio of colon carcinoma is an independent factor for survival compared to lymph node status and tumor stage. Cell Oncol : Off J Int Soc Cell Oncol. 2007;29(5):387–98.
Sis B, Sarioglu S, Sokmen S, Sakar M, Kupelioglu A, Fuzun M. Desmoplasia measured by computer assisted image analysis: an independent prognostic marker in colorectal carcinoma. J Clin Pathol. 2005;58(1):32–8. https://doi.org/10.1136/jcp.2004.018705.
Dingemans KP, Zeeman-Boeschoten IM, Keep RF, Das PK. Transplantation of colon carcinoma into granulation tissue induces an invasive morphotype. Int J Cancer J Int Du Cancer. 1993;54(6):1010–6. https://doi.org/10.1002/ijc.2910540625.
De Wever O, Mareel M. Role of tissue stroma in cancer cell invasion. J Pathol. 2003;200(4):429–47. https://doi.org/10.1002/path.1398.
Rafferty MA, Fenton JE, Jones AS. The history, aetiology and epidemiology of laryngeal carcinoma. Cli Otolaryngol Allied Sci. 2001;26(6):442–6. https://doi.org/10.1046/j.1365-2273.2001.00507.x.
Sert Bektas S, Inan Mamak G, Ciris IM, Bozkurt KK, Kapucuoglu N. Tumor budding in colorectal carcinomas. Turk Patoloji Dergisi. 2012;28(1):61–6. https://doi.org/10.5146/tjpath.2012.01099.
Witkiewicz AK, Kline J, Queenan M, Brody JR, Tsirigos A, Bilal E, et al. Molecular profiling of a lethal tumor microenvironment, as defined by stromal caveolin-1 status in breast cancers. Cell Cycle. 2011;10(11):1794–809. https://doi.org/10.4161/cc.10.11.15675.
Witkiewicz AK, Whitaker-Menezes D, Dasgupta A, Philp NJ, Lin Z, Gandara R, et al. Using the “reverse Warburg effect” to identify high-risk breast cancer patients: stromal MCT4 predicts poor clinical outcome in triple-negative breast cancers. Cell Cycle. 2012;11(6):1108–17. https://doi.org/10.4161/cc.11.6.19530.
Dickson JM, Weavers HM, Mitchell N, Winter EM, Wilkinson ID, VanBeek EJ, et al. Choice of cross size in stereology—a cautionary note. Neuroradiology. 2003;45(12):896–9. https://doi.org/10.1007/s00234-003-1091-0.
Amenabar JM, Martins GB, Cherubini K, Figueiredo MA. Comparison between semi-automated segmentation and manual point-counting methods for quantitative analysis of histological sections. J Oral Sci. 2006;48(3):139–43. https://doi.org/10.2334/josnusd.48.139.
Acknowledgments
The operations and follow-up of the patients in this series were performed by the general surgeons Selman Sokmen, Cem Terzi, Aras Emre Canda, and Mehmet Fuzun. Abdullah Haluk Sirin worked at the preparation of the follow-up data of the patients. The histopathological evaluation of the patients was performed by Sulen Sarioglu, Ozgul Sagol, and Mehtat Unlu. The hypothesis of the study was presented by Sulen Sarioglu. The mucinous carcinoma cases with follow-up information were selected by the whole authors. The methodology of the study was described by Sulen Sarioglu and performed mainly by Guray Akturk. The statistical analysis was performed by Hulya Ellidokuz, and the results were again discussed and analyzed by the whole group. The manuscript was written by Guray Akturk and Sulen Sarioglu and corrected according to the suggestions of all the authors.
The study did not require any funding. We appreciate the help of pathology archive workers Huseyin Dogan and Alperen Korana for their support with the tissue sections.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The project was approved by the Dokuz Eylul University Ethics Committee at 25 January 2014 (no.: 873-GOA).
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sarioglu, S., Akturk, G., Sokmen, S. et al. The Prognostic Implications of FIX and FLO Patterns in Mucinous Colon Carcinomas. J Gastrointest Canc 50, 254–259 (2019). https://doi.org/10.1007/s12029-018-0059-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-018-0059-6