Abstract
Background
Postinterventional cerebral hyperdensities are common on non-contrast-enhanced computed tomography (CT) after endovascular thrombectomy in patients with acute ischemic stroke, which may reflect blood–brain barrier damage. The disruption of the blood–brain barrier may lead to malignant brain edema. The relationship between the extent of postinterventional cerebral hyperdensities and malignant brain edema is unclear.
Methods
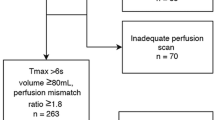
Patients with middle cerebral artery territory infarction and successful recanalization were consecutively enrolled. Postinterventional non-contrast-enhanced CT was performed to evaluate postinterventional cerebral hyperdensities within 24 h after endovascular thrombectomy. On the basis of the areas of the Alberta Stroke Program Early CT Score, we devised the Hyperdensity on CT Score to evaluate the extent of postinterventional cerebral hyperdensities. The primary outcome was malignant brain edema, defined as the development of clinical signs of herniation (including a decrease in consciousness and/or anisocoria), accompanied by imaging evidence of brain swelling. The component of postinterventional cerebral hyperdensities was divided into contrast staining and hemorrhage on the basis of persistency.
Results
Three hundred sixty patients were included (50.6% male, mean age 67.9 years), of whom 247 (68.6%) developed postinterventional cerebral hyperdensities and 66 (18.3%) developed malignant brain edema. After adjustment for confounders, including the component of postinterventional cerebral hyperdensities, the extent of postinterventional cerebral hyperdensities assessed by the Hyperdensity on CT Score was significantly associated with malignant brain edema (odds ratio 1.46, 95% confidence interval 1.20–1.77, p < 0.001). A Hyperdensity on CT Score greater than 3 had a sensitivity of 0.73 and a specificity of 0.87 for predicting malignant brain edema.
Conclusions
The extent of postinterventional cerebral hyperdensities on postinterventional non-contrast-enhanced CT was associated with malignant brain edema. The Hyperdensity on CT Score could be used to predict malignant brain edema regardless of the component of postinterventional cerebral hyperdensities.





Similar content being viewed by others
Change history
11 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12028-021-01419-6
References
Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723–31.
Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-418.
Kim JM, Bae JH, Park KY, et al. Incidence and mechanism of early neurological deterioration after endovascular thrombectomy. J Neurol. 2019;266(3):609–15.
Huang X, Yang Q, Shi X, et al. Predictors of malignant brain edema after mechanical thrombectomy for acute ischemic stroke. J Neurointerv Surg. 2019;11(10):994–8.
Thorén M, Dixit A, Escudero-Martínez I, et al. Effect of recanalization on cerebral edema in ischemic stroke treated with thrombolysis and/or endovascular therapy. Stroke. 2020;51(1):216–23.
White OB, Norris JW, Hachinski VC, Lewis A. Death in early stroke, causes and mechanisms. Stroke. 1979;10(6):743.
Huttner HB, Schwab S. Malignant middle cerebral artery infarction: clinical characteristics, treatment strategies, and future perspectives. Lancet Neurol. 2009;8(10):949–58.
Berrouschot J, Sterker M, Bettin S, Köster J, Schneider D. Mortality of space-occupying ('malignant’) middle cerebral artery infarction under conservative intensive care. Intensive Care Med. 1998;24(6):620–3.
Wijdicks EF, Diringer MN. Middle cerebral artery territory infarction and early brain swelling: progression and effect of age on outcome. Mayo Clin Proc. 1998;73(9):829–36.
Ropper AH. Lateral displacement of the brain and level of consciousness in patients with an acute hemispheral mass. N Engl J Med. 1986;314(15):953–8.
Vahedi K, Hofmeijer J, Juettler E, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2007;6(3):215–22.
Dekeyzer S, Nikoubashman O, Lutin B, et al. Distinction between contrast staining and hemorrhage after endovascular stroke treatment: one CT is not enough. J Neurointerv Surg. 2017;9(4):394–8.
Yoon W, Seo JJ, Kim JK, et al. Contrast enhancement and contrast extravasation on computed tomography after intra-arterial thrombolysis in patients with acute ischemic stroke. Stroke. 2004;35(4):876–81.
Yedavalli V, Sammet S. Contrast extravasation versus hemorrhage after thrombectomy in patients with acute stroke. J Neuroimaging. 2017;27(6):570–6.
Xu C, Zhou Y, Zhang R, et al. Metallic hyperdensity sign on noncontrast ct immediately after mechanical thrombectomy predicts parenchymal hemorrhage in patients with acute large-artery occlusion. AJNR Am J Neuroradiol. 2019;40(4):661–7.
Nakano S, Iseda T, Kawano H, et al. Parenchymal hyperdensity on computed tomography after intra-arterial reperfusion therapy for acute middle cerebral artery occlusion: incidence and clinical significance. Stroke. 2001;32(9):2042–8.
Parrilla G, García-Villalba B, Espinosa de Rueda M, et al. Hemorrhage/contrast staining areas after mechanical intra-arterial thrombectomy in acute ischemic stroke: imaging findings and clinical significance. AJNR Am J Neuroradiol. 2012;33(9):1791–6.
Nikoubashman O, Reich A, Gindullis M, et al. Clinical significance of post-interventional cerebral hyperdensities after endovascular mechanical thrombectomy in acute ischaemic stroke. Neuroradiology. 2014;56(1):41–50.
Kim JT, Heo SH, Cho BH, et al. Hyperdensity on non-contrast CT immediately after intra-arterial revascularization. J Neurol. 2012;259(5):936–43.
Kim JM, Park KY, Lee WJ, et al. The cortical contrast accumulation from brain computed tomography after endovascular treatment predicts symptomatic hemorrhage. Eur J Neurol. 2015;22(11):1453–8.
Puntonet J, Richard ME, Edjlali M, et al. Imaging findings after mechanical thrombectomy in acute ischemic stroke. Stroke. 2019;50(6):1618–25.
Simard JM, Kent TA, Chen M, Tarasov KV, Gerzanich V. Brain oedema in focal ischaemia: molecular pathophysiology and theoretical implications. Lancet Neurol. 2007;6(3):258–68.
Zaidat OO, Yoo AJ, Khatri P, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44(9):2650–63.
Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Higashida RT, Furlan AJ, Roberts H, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003;34(8):e109–37.
Lummel N, Schulte-Altedorneburg G, Bernau C, et al. Hyperattenuated intracerebral lesions after mechanical recanalization in acute stroke. AJNR Am J Neuroradiol. 2014;35(2):345–51.
Hacke W, Kaste M, Fieschi C, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet. 1998;352(9136):1245–51.
Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000;355(9216):1670–4.
Wu S, Yuan R, Wang Y, et al. Early prediction of malignant brain edema after ischemic stroke. Stroke. 2018;49(12):2918–27.
Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-110.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45.
Payabvash S, Qureshi MH, Khan SM, et al. Differentiating intraparenchymal hemorrhage from contrast extravasation on post-procedural noncontrast CT scan in acute ischemic stroke patients undergoing endovascular treatment. Neuroradiology. 2014;56(9):737–44.
Jang YM, Lee DH, Kim HS, et al. The fate of high-density lesions on the non-contrast CT obtained immediately after intra-arterial thrombolysis in ischemic stroke patients. Korean J Radiol. 2006;7(4):221–8.
Lun R, Walker GB, Guenego A, et al. Is this contrast? Is this blood? An agreement study on post-thrombectomy computed tomography scans. Front Neurol. 2020;11:593098.
Tijssen MP, Hofman PA, Stadler AA, et al. The role of dual energy CT in differentiating between brain haemorrhage and contrast medium after mechanical revascularisation in acute ischaemic stroke. Eur Radiol. 2014;24(4):834–40.
Liu K, Jiang L, Ruan J, et al. The role of dual energy ct in evaluating hemorrhagic complications at different stages after thrombectomy. Front Neurol. 2020;11:583411.
Kimberly WT, Dutra BG, Boers AMM, et al. Association of reperfusion with brain edema in patients with acute ischemic stroke: a secondary analysis of the MR CLEAN Trial. JAMA Neurol. 2018;75(4):453–61.
Song SY, Ahn SY, Rhee JJ, et al. Extent of contrast enhancement on non-enhanced computed tomography after intra-arterial thrombectomy for acute infarction on anterior circulation: as a predictive value for malignant brain edema. J Korean Neurosurg Soc. 2015;58(4):321–7.
van der Worp HB, Hofmeijer J, Juttler E, et al. European Stroke Organisation (ESO) guidelines on the management of space-occupying brain infarction. Eur Stroke J. 2021;6(2):XC–CX.
Funding
BW, FH, ZH, and SW obtained public funding. This work was supported by the National Key Development Plan for Precision Medicine Research (2017YFC0910004), the National Natural Science Foundation of China (81671146, 81870937, 82171285, 81371281), the Science and Technology Department of Sichuan Province (2021YJ0433, 2017SZ0007), and the 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYGD18009).
Author information
Authors and Affiliations
Contributions
BW and FH conceived and designed the study. CW, QZ, TC and TY acquired the data, which CW, ZH and SW analyzed. CW, LW, ZH and SW aided in data interpretation and wrote the manuscript. All authors were involved in revising the article and approved the final version.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical Approval/Informed Consent
This study was approved by the Scientific Research Department of West China Hospital. Informed consent was obtained from patients or their next of kin.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, C., Zhu, Q., Cui, T. et al. Early Prediction of Malignant Edema After Successful Recanalization in Patients with Acute Ischemic Stroke. Neurocrit Care 36, 822–830 (2022). https://doi.org/10.1007/s12028-021-01380-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01380-4