Abstract
Objective
To estimate and compare sex-specific differences between metabolically healthy overweight/obesity (MHOO) and the risk of hypertension among Dong, Bouyei, and Miao adults in southwest China.
Methods
MHOO was diagnosed when the patient had a body mass index ≥24 kg/m2 and the presence of ≤1 component of metabolic syndrome. The main outcome was the occurrence of hypertension after the diagnosis or measurement by a physician at the baseline survey. Multivariate logistic regression models were used to estimate odds ratios (ORs) and 95% confidence intervals (CIs) between MHOO and the risk of hypertension.
Results
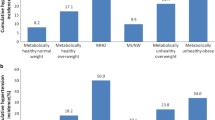
We enrolled 16,433 Chinese Dong, Bouyei, and Miao adults. Using the metabolically healthy normal weight (MHNW) as a reference and after adjusting for confounders, the association between MHOO and the risk of hypertension was stronger in Dong (OR = 1.46, 95% CI: 1.07–2.00) and Miao (OR = 2.05, 95% CI: 1.48–2.85) men and did not exist in Bouyei men (OR = 1.14, 95% CI: 0.81–1.60). After adjusting for the age, the association between MHOO and the risk of hypertension was stronger in men than in women among Dong adults aged 30–59 years (OR = 1.64, 95% CI: 1.12–2.40) and did not differ between men and women among Dong adults aged 60–79 years or among Miao or Bouyei adults.
Conclusion
The results of this study demonstrated sex-specific differences in the association between MHOO and the risk of hypertension and that sex-specific differences further differed among Dong, Bouyei, and Miao adults.

Similar content being viewed by others
References
NCD Risk Factor Collaboration (NCD-RisC), Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 398(10304), 957–980 (2019). https://doi.org/10.1016/S0140-6736(21)01330-1
J.F. Reckelhoff, Gender differences in hypertension. Curr. Opin. Nephrol. Hypertens. 27(3), 176–181 (2018). https://doi.org/10.1097/MNH.0000000000000404
J. Lu, Y. Lu, X. Wang, X. Li, G.C. Linderman, C. Wu, X. Cheng, L. Mu, H. Zhang, J. Liu, M. Su, H. Zhao, E.S. Spatz, J.A. Spertus, F.A. Masoudi, H.M. Krumholz, L. Jiang, Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 390(10112), 2549–2558 (2017). https://doi.org/10.1016/S0140-6736(17)32478-9
S.S. Virani, A. Alonso, H.J. Aparicio, E.J. Benjamin, M.S. Bittencourt, C.W. Callaway, A.P. Carson, A.M. Chamberlain, S. Cheng, F.N. Delling, M. Elkind, K.R. Evenson, J.F. Ferguson, D.K. Gupta, S.S. Khan, B.M. Kissela, K.L. Knutson, C.D. Lee, T.T. Lewis, J. Liu; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee, Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation 143(8), e254–e743 (2021). https://doi.org/10.1161/CIR.0000000000000950
S. Lewington, B. Lacey, R. Clarke, Y. Guo, X.L. Kong, L. Yang, Y. Chen, Z. Bian, J. Chen, J. Meng, Y. Xiong, T. He, Z. Pang, S. Zhang, R. Collins, R. Peto, L. Li, Z. Chen; China Kadoorie Biobank Consortium, The Burden of Hypertension and Associated Risk for Cardiovascular Mortality in China. JAMA Intern. Med. 176(4), 524–532 (2016). https://doi.org/10.1001/jamainternmed.2016.0190
M.H. Forouzanfar, P. Liu, G.A. Roth, M. Ng, S. Biryukov, L. Marczak, L. Alexander, K. Estep, K. Hassen Abate, T.F. Akinyemiju, R. Ali, N. Alvis-Guzman, P. Azzopardi, A. Banerjee, T. Bärnighausen, A. Basu, T. Bekele, D.A. Bennett, S. Biadgilign, F. Catalá-López, C.J. Murray, Global Burden of Hypertension and Systolic Blood Pressure of at Least 110 to 115 mm Hg, 1990-2015. JAMA 317(2), 165–182 (2017). https://doi.org/10.1001/jama.2016.19043
K.T. Mills, A. Stefanescu, J. He, The global epidemiology of hypertension. Nat. Rev. Nephrol. 16(4), 223–237 (2020). https://doi.org/10.1038/s41581-019-0244-2
D. Susic, J. Varagic, Obesity: A Perspective from Hypertension. Med. Clin. North Am. 101(1), 139–157 (2017). https://doi.org/10.1016/j.mcna.2016.08.008
A. Engin, The Definition and Prevalence of Obesity and Metabolic Syndrome. Adv. Exp. Med. Biol. 960, 1–17 (2017). https://doi.org/10.1007/978-3-319-48382-5_1
M. Blüher, Metabolically Healthy Obesity. Endocr. Rev. 41(3), bnaa004 (2020). https://doi.org/10.1210/endrev/bnaa004
D. Samocha-Bonet, V.D. Dixit, C.R. Kahn, R.L. Leibel, X. Lin, M. Nieuwdorp, K.H. Pietiläinen, R. Rabasa-Lhoret, M. Roden, P.E. Scherer, S. Klein, E. Ravussin, Metabolically healthy and unhealthy obese–the 2013 Stock Conference report. Obes. Rev. 15(9), 697–708 (2014). https://doi.org/10.1111/obr.12199
R.P. Wildman, P. Muntner, K. Reynolds, A.P. McGinn, S. Rajpathak, J. Wylie-Rosett, M.R. Sowers, The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch. Intern. Med. 168(15), 1617–1624 (2008). https://doi.org/10.1001/archinte.168.15.1617
N. Stefan, K. Kantartzis, J. Machann, F. Schick, C. Thamer, K. Rittig, B. Balletshofer, F. Machicao, A. Fritsche, H.U. Häring, Identification and characterization of metabolically benign obesity in humans. Arch. Intern. Med. 168(15), 1609–1616 (2008). https://doi.org/10.1001/archinte.168.15.1609
N. Stefan, Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 8(7), 616–627 (2020). https://doi.org/10.1016/S2213-8587(20)30110-8
A. Mirzababaei, H. Mozaffari, S. Shab-Bidar, A. Milajerdi, K. Djafarian, Risk of hypertension among different metabolic phenotypes: a systematic review and meta-analysis of prospective cohort studies. J. Hum. Hypertens. 33(5), 365–377 (2019). https://doi.org/10.1038/s41371-018-0146-y
S.Y. Jae, A.S. Babu, E.S. Yoon, S. Kurl, J.A. Laukkanen, Y.H. Choi, B.A. Franklin, Impact of Cardiorespiratory Fitness and Risk of Systemic Hypertension in Nonobese Versus Obese Men Who Are Metabolically Healthy or Unhealthy. Am. J. Cardiol. 120(5), 765–768 (2017). https://doi.org/10.1016/j.amjcard.2017.05.054
S.K. Lee, S.H. Kim, G.Y. Cho, I. Baik, H.E. Lim, C.G. Park, J.B. Lee, Y.H. Kim, S.Y. Lim, H. Kim, C. Shin, Obesity phenotype and incident hypertension: a prospective community-based cohort study. J. Hypertens. 31(1), 145–151 (2013). https://doi.org/10.1097/HJH.0b013e32835a3637
M. Kuwabara, R. Kuwabara, I. Hisatome, K. Niwa, C.A. Roncal-Jimenez, P. Bjornstad, A. Andres-Hernando, Y. Sato, T. Jensen, G. Garcia, M. Ohno, J.O. Hill, M.A. Lanaspa, R.J. Johnson, “Metabolically Healthy” Obesity and Hyperuricemia Increase Risk for Hypertension and Diabetes: 5-year Japanese Cohort Study. Obes. (Silver Spring). 25(11), 1997–2008 (2017). https://doi.org/10.1002/oby.22000
M. Fujita, A. Hata, Sex and age differences in the effect of obesity on incidence of hypertension in the Japanese population: A large historical cohort study. J. Am. Soc. Hypertens. 8(1), 64–70 (2014). https://doi.org/10.1016/j.jash.2013.08.001
K. Colafella, K.M. Denton, Sex-specific differences in hypertension and associated cardiovascular disease. Nat. Rev. Nephrol. 14(3), 185–201 (2018). https://doi.org/10.1038/nrneph.2017.189
M. Kabootari, S. Akbarpour, F. Azizi, F. Hadaegh, Sex specific impact of different obesity phenotypes on the risk of incident hypertension: Tehran lipid and glucose study. Nutr. Metab. (Lond.) 16, 16 (2019). https://doi.org/10.1186/s12986-019-0340-0
J.K. Yoo, Q. Fu, Impact of sex and age on metabolism, sympathetic activity, and hypertension. FASEB J. 34(9), 11337–11346 (2020). https://doi.org/10.1096/fj.202001006RR
J.M. Raison, A.M. Achimastos, M.E. Safar, Sex-dependence of body fat distribution in patients with obesity and hypertension. Clin. Exp. Hypertens. A 14(3), 505–525 (1992). https://doi.org/10.3109/10641969209036203
X. Zhao, F. Hong, J. Yin, W. Tang, G. Zhang, X. Liang, J. Li, C. Cui, X. Li; China Multi-Ethnic Cohort (CMEC) collaborative group, Cohort Profile: the China Multi-Ethnic Cohort (CMEC) study. Int J. Epidemiol. 50(3), 721–7211 (2021). https://doi.org/10.1093/ije/dyaa185
B.F. Zhou, Cooperative Meta-Analysis Group of the Working Group on Obesity in China, Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. 15(1), 83–96 (2002)
K.G. Alberti, R.H. Eckel, S.M. Grundy, P.Z. Zimmet, J.I. Cleeman, K.A. Donato, J.C. Fruchart, W.P. James, C.M. Loria, S.C. Smith Jr, International Diabetes Federation Task Force on Epidemiology and Prevention, Hational Heart, Lung, and Blood Institute, American Heart Association, World Heart Federation, International Atherosclerosis Society, International Association for the Study of Obesity, Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16), 1640–1645 (2009). https://doi.org/10.1161/CIRCULATIONAHA.109.192644
M.B. Schulze, Metabolic health in normal-weight and obese individuals. Diabetologia 62(4), 558–566 (2019). https://doi.org/10.1007/s00125-018-4787-8
S. Tian, Y. Xu, H. Dong, The effect of metabolic health and obesity phenotypes on risk of hypertension: a nationwide population-based study using 5 representative definitions of metabolic health. Med. (Baltim.) 97(38), e12425 (2018). https://doi.org/10.1097/MD.0000000000012425
Y. Zhao, P. Qin, H. Sun, Y. Liu, D. Liu, Q. Zhou, C. Guo, Q. Li, G. Tian, X. Wu, D. Hu, X. Sun, M. Zhang, Metabolically healthy general and abdominal obesity are associated with increased risk of hypertension. Br. J. Nutr. 123(5), 583–591 (2020). https://doi.org/10.1017/S0007114519003143
D.R. Young, H. Fischer, D. Arterburn, D. Bessesen, L. Cromwell, M.F. Daley, J. Desai, A. Ferrara, S.L. Fitzpatrick, M.A. Horberg, C. Koebnick, C.L. Nau, C. Oshiro, B. Waitzfelder, A. Yamamoto, Associations of overweight/obesity and socioeconomic status with hypertension prevalence across racial and ethnic groups. J. Clin. Hypertens. (Greenwich) 20(3), 532–540 (2018). https://doi.org/10.1111/jch.13217
R.J. Wong, C. Chou, S.R. Sinha, A. Kamal, A. Ahmed, Ethnic disparities in the association of body mass index with the risk of hypertension and diabetes. J. Community Health 39(3), 437–445 (2014). https://doi.org/10.1007/s10900-013-9792-8
H. Fan, X. Zhang, Effects of smoking intensity trajectory, cumulative smoking exposure, and the number of years since quitting on the subsequent risk of hypertension. J. Clin. Hypertens. (Greenwich) 24(7), 937–944 (2022). https://doi.org/10.1111/jch.14534
H.E. Badr, S. Rao, F. Manee, Gender differences in quality of life, physical activity, and risk of hypertension among sedentary occupation workers. Qual. Life Res. 30(5), 1365–1377 (2021). https://doi.org/10.1007/s11136-020-02741-w
F. Zhao, Q. Liu, Y. Li, X. Feng, H. Chang, J. Lyu, Association between alcohol consumption and hypertension in Chinese adults: Findings from the CHNS. Alcohol 83, 83–88 (2020). https://doi.org/10.1016/j.alcohol.2019.09.004
G. Navarro, C. Allard, W. Xu, F. Mauvais-Jarvis, The role of androgens in metabolism, obesity, and diabetes in males and females. Obes. (Silver Spring) 23(4), 713–719 (2015). https://doi.org/10.1002/oby.21033
J.L. Faulkner, E.J. Belin de Chantemèle, Sex Differences in Mechanisms of Hypertension Associated With Obesity. Hypertension 71(1), 15–21 (2018). https://doi.org/10.1161/HYPERTENSIONAHA.117.09980
A.M. Kaneva, E.R. Bojko, Sex differences in the association between obesity and hypertension. Arch. Physiol. Biochem. 1–8 (2021). https://doi.org/10.1080/13813455.2020.1861027
G. Seravalle, G. Grassi, Obesity and hypertension. Pharm. Res. 122, 1–7 (2017). https://doi.org/10.1016/j.phrs.2017.05.013
M.T. Schütten, A.J. Houben, P.W. de Leeuw, C.D. Stehouwer, The Link Between Adipose Tissue Renin-Angiotensin-Aldosterone System Signaling and Obesity-Associated Hypertension. Physiol. (Bethesda) 32(3), 197–209 (2017). https://doi.org/10.1152/physiol.00037.2016
G.F. DiBona, Sympathetic nervous system and hypertension. Hypertension 61(3), 556–560 (2013). https://doi.org/10.1161/HYPERTENSIONAHA.111.00633
Q. Fu, Sex differences in sympathetic activity in obesity and its related hypertension. Ann. N. Y Acad. Sci. 1454(1), 31–41 (2019). https://doi.org/10.1111/nyas.14095
L.J. Briant, N. Charkoudian, E.C. Hart, Sympathetic regulation of blood pressure in normotension and hypertension: when sex matters. Exp. Physiol. 101(2), 219–229 (2016). https://doi.org/10.1113/EP085368
L.E. Taylor, J.C. Sullivan, Sex differences in obesity-induced hypertension and vascular dysfunction: a protective role for estrogen in adipose tissue inflammation? Am. J. Physiol. Am. J. Physiol. Regul. Integr. Comp. Physiol. 311(4), R714–R720 (2016). https://doi.org/10.1152/ajpregu.00202.2016
S.C. Chen, T.C. Lo, J.H. Chang, H.W. Kuo, Variations in aging, gender, menopause, and obesity and their effects on hypertension in taiwan. Int J. Hypertens. 2014, 515297 (2014). https://doi.org/10.1155/2014/515297
J.H. Ryoo, S.K. Park, C.M. Oh, Y.J. Choi, J.Y. Chung, W.T. Ham, T. Jung, Evaluating the risk of hypertension according to the metabolic health status stratified by degree of obesity. J. Am. Soc. Hypertens. 11(1), 20–27.e4 (2017). https://doi.org/10.1016/j.jash.2016.10.006
Y.M. Kang, C.H. Jung, J.E. Jang, J.Y. Hwang, E.H. Kim, J.Y. Park, H.K. Kim, W.J. Lee, The association of incident hypertension with metabolic health and obesity status: definition of metabolic health does not matter. Clin. Endocrinol. (Oxf.) 85(2), 207–215 (2016). https://doi.org/10.1111/cen.13074
S.K. Lee, S.H. Kim, G.Y. Cho, I. Baik, H.E. Lim, C.G. Park, J.B. Lee, Y.H. Kim, S.Y. Lim, H. Kim, C. Shin, Obesity phenotype and incident hypertension: a prospective community-based cohort study. J. Hypertens. 31(1), 145–151 (2013). https://doi.org/10.1097/HJH.0b013e32835a3637
C. Iacobini, G. Pugliese, C. Blasetti Fantauzzi, M. Federici, S. Menini, Metabolically healthy versus metabolically unhealthy obesity. Metabolism 92, 51–60 (2019). https://doi.org/10.1016/j.metabol.2018.11.009
Acknowledgements
The investigators are grateful to the dedicated participants and all research staff of the study. The project was supported with the National Key R&D Program of China, Grant/Award Number: 2017YFC0907301 and the Science and Technology Plan Project of Guizhou Province, China: QKHPTRC [2018]5403.
Funding
This work was supported by the National Key R&D Program of China, Grant/Award Number: 2017YFC0907301 and the Science and Technology Plan Project of Guizhou Province, China: QKHPTRC [2018]5403.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by X.W., Q.Z., N.M., L.P., L.L. The first draft of the paper was written by X.W., and all authors commented on previous versions of the paper. The authors have read and approved the final paper.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
Approvals were given by the following organizations and institutes: the Sichuan University Medical Ethical Review Board (K2016038) and the research ethics committee of the Affiliated Hospital of Guizhou Medical University (2018[094]). Prior to the study, all the participants had read and signed informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Zeng, Q., Ma, N. et al. Sex-specific differences in the association between metabolically healthy overweight/obesity and the risk of hypertension in Chinese ethnic minorities. Endocrine 80, 317–327 (2023). https://doi.org/10.1007/s12020-023-03308-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03308-8