Abstract
Purpose
To investigate endocrine function changes after non-functioning pituitary adenomas (NFPA) transsphenoidal surgery and to search for predictors of hypopituitarism resolution and development.
Methods
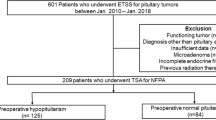
We included 117 patients with NFPA who underwent endoscopic transsphenoidal surgery from 2005 to 2019 by two neurosurgeons. Twenty-one patients were excluded because of previous pituitary surgery or radiotherapy. We assessed symptoms at diagnosis, tumour volume, tumour removal, hormonal status at diagnosis, hormonal outcomes at 2- and 12-month follow-up, and complications. Pituitary stalk and gland MRI status (visible or not) were included, and it theirs association to hormonal function was studied for the first time, to our knowledge.
Results
Pituitary gland visualization was more frequent in those patients who showed a smaller number of axes affected at 12 months (p = 0.011). Pituitary stalk status showed no association to hormonal function. The hormonal normalization rate at 12 months was 13%. The endocrine improvement rate at 12 months was 16.7%. Worsening of hormonal function occurred in 19.8% of patients. Younger age was associated to hormonal improvement (p = 0.004). Higher preoperative tumour volume (p = 0.015) and absence of gross total resection (GTR) (p = 0.049) were associated with worsening in at least one hormonal axis after surgery.
Conclusions
Pituitary gland visibility was higher in those patients who showed better hormonal outcomes. Assessment of initial hormonal function and outcome after surgery regarding pituitary stalk status showed no significant association. Higher preoperative tumour volumes and absence of GTR were associated to postoperative endocrine function worsening, while younger age was associated to its improvement.





Similar content being viewed by others
Data availability
All data are available under request.
Abbreviations
- NFPA:
-
non-functioning pituitary adenomas
- DI:
-
diabetes Insipidus
- SIADH:
-
syndrome of inappropriate antidiuretic hormone secretion
- MRI:
-
magnetic resonance imaging
- GTR:
-
gross total resection
- GH:
-
growth hormone
- IGF-1:
-
insulin-like growth factor 1
- TSH:
-
thyroid-stimulating hormone
- T4:
-
thyroxine
- ACTH:
-
adrenocorticotropic hormone
- FSH:
-
follicle-stimulating hormone
- LH:
-
luteinizing hormone
- CI:
-
confidence interval
References
S. Wang, B. Li, C. Ding et al. A novel “total pituitary hormone index” as an indicator of postoperative pituitary function in patients undergoing resection of pituitary adenomas. Oncotarget 8 (2017). https://doi.org/10.18632/oncotarget.15978
M.G. Lake, L.S. Krook, S.V. Cruz, Pituitary adenomas: an overview. Am. Fam. Physician 88, 319–327 (2013).
M.L.C. Cury, A.R. de, J.C. Fernandes, H.R. Machado et al. Non-functioning pituitary adenomas: clinical feature, laboratorial and imaging assessment, therapeutic management and outcome. Arq. Bras. Endocrinol. Metab. 53, 31–39 (2009). https://doi.org/10.1590/s0004-27302009000100006
D. Esposito, D.S. Olsson, O. Ragnarsson, et al. Non-functioning pituitary adenomas: indications for pituitary surgery and post-surgical management. Pituitary 22, 422–434 (2019).
G. Ntali, J.A. Wass, Epidemiology, clinical presentation and diagnosis of non-functioning pituitary adenomas. Pituitary 21, 111–118 (2018)
J.H. Kim, J.H. Lee, J.H. Lee et al. Endoscopic transsphenoidal surgery outcomes in 331 nonfunctioning pituitary adenoma cases after a single surgeon learning curve. World Neurosurg. 109, e409–e416 (2018). https://doi.org/10.1016/j.wneu.2017.09.194
A. Jahangiri, J.R. Wagner, S.W. Han et al. Improved versus worsened endocrine function after transsphenoidal surgery for nonfunctional pituitary adenomas: rate, time course, and radiological analysis. J. Neurosurg. 124, 589–595 (2016). https://doi.org/10.3171/2015.1.JNS141543
M.R. Drange, N.R. Fram, V. Herman-Bonert, S. Melmed, Pituitary tumor registry: a novel clinical resource. J. Clin. Endocrinol. Metab. 85, 168–174 (2000). https://doi.org/10.1210/jcem.85.1.6309
K. Kovacs, B.W. Scheithauer, E. Horvath, R.V. Lloyd, The world health organization classification of adenohypophysial neoplasms: a proposed five-tier scheme. Cancer 78, 502–510 (1996). https://doi.org/10.1002/(SICI)1097-0142(19960801)78:3<502::AID-CNCR18>3.0.CO;2-2
M. Fleseriu, M.E. Bodach, L.M. Tumialan et al. Guidelines: congress of neurological surgeons systematic review and evidence-based guideline for pretreatment endocrine evaluation of patients with nonfunctioning pituitary adenomas. Neurosurgery 79, E527–E529 (2016). https://doi.org/10.1227/NEU.0000000000001387
C.E. Higham, G. Johannsson, S.M. Shalet, Hypopituitarism. Lancet 388, 2403–2415 (2016).
P. Nayak, A.S. Montaser, J. Hu et al. Predictors of postoperative diabetes insipidus following endoscopic resection of pituitary adenomas. J. Endocr. Soc. 2, 1010–1019 (2018). https://doi.org/10.1210/js.2018-00121
A.H. Sam, S. Shah, K. Saleh et al. Clinical outcomes in patients with nonfunctioning pituitary adenomas managed conservatively. Clin. Endocrinol. 83, 861–865 (2015). https://doi.org/10.1111/cen.12860
N. Karavitaki, K. Collison, J. Halliday et al. What is the natural history of nonoperated nonfunctioning pituitary adenomas? Clin. Endocrinol. 67, 938–943 (2007). https://doi.org/10.1111/j.1365-2265.2007.02990.x
M.M. Fernández-Balsells, M.H. Murad, A. Barwise et al. Natural history of nonfunctioning pituitary adenomas and incidentalomas: a systematic review and metaanalysis. J. Clin. Endocrinol. Metab. 96, 905–912 (2011). https://doi.org/10.1210/jc.2010-1054
M.H. Murad, M.M. Fernández-Balsells, A. Barwise et al. Outcomes of surgical treatment for nonfunctioning pituitary adenomas: a systematic review and meta-analysis. Clin. Endocrinol. 73, 777–791 (2010). https://doi.org/10.1111/j.1365-2265.2010.03875.x
P.U. Freda, A.M. Beckers, L. Katznelson et al. Pituitary incidentaloma: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 96, 894–904 (2011). https://doi.org/10.1210/jc.2010-1048
W.H.A. Ryu, S. Tam, B. Rotenberg et al. Conservative management of pituitary macroadenoma contacting the optic apparatus. Can. J. Neurol. Sci. 37, 837–842 (2010). https://doi.org/10.1017/s0317167100051532
O.M. Dekkers, S. Hammer, R.J.W. de Keizer et al. The natural course of non-functioning pituitary macroadenomas. Eur. J. Endocrinol. 156, 217–224 (2007). https://doi.org/10.1530/eje.1.02334
A.S. Little, D.F. Kelly, W.L. White et al. Results of a prospective multicenter controlled study comparing surgical outcomes of microscopic versus fully endoscopic transsphenoidal surgery for nonfunctioning pituitary adenomas: the Transsphenoidal Extent of Resection (TRANSSPHER) Study. J. Neurosurg. 1–11 (2019). https://doi.org/10.3171/2018.11.jns181238
J.K. Goudakos, K.D. Markou, C. Georgalas, Endoscopic versus microscopic trans-sphenoidal pituitary surgery: a systematic review and meta-analysis. Clin. Otolaryngol. 36, 212–220 (2011). https://doi.org/10.1111/j.1749-4486.2011.02331.x
H.A. Zaidi, A.W. Awad, M.A. Bohl et al. Comparison of outcomes between a less experienced surgeon using a fully endoscopic technique and a very experienced surgeon using a microscopic transsphenoidal technique for pituitary adenoma. J. Neurosurg. 124 (2016). https://doi.org/10.3171/2015.4.JNS15102
M. Zhu, J. Yang, Y. Wang, et al. Endoscopic transsphenoidal surgery versus microsurgery for the resection of pituitary adenomas: a systematic review. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 49, 236–239 (2014).
A. Karppinen, L. Kivipelto, S. Vehkavaara et al. Transition from microscopic to endoscopic transsphenoidal surgery for nonfunctional pituitary adenomas. World Neurosurg. 84 (2015). https://doi.org/10.1016/j.wneu.2015.02.024
T. Česák, P. Póczoš, J. Adamkov et al. Microsurgical versus endoscopic surgery for non-functioning pituitary adenomas: a retrospective study. Croat. Med. J. 61 (2020). https://doi.org/10.3325/CMJ.2020.61.410
Y. Esquenazi, W.I. Essayed, H. Singh, et al. Endoscopic endonasal versus microscopic transsphenoidal surgery for recurrent and/or residual pituitary adenomas. World Neurosurg 101, 186–195 (2017).
E. von Elm, D.G. Altman, M. Egger et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 12 (2014). https://doi.org/10.1016/j.ijsu.2014.07.013
E. Knosp, E. Steiner, K. Kitz, C. Matula, Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33 (1993). https://doi.org/10.1227/00006123-199310000-00008
C.R. Ku, J.W. Hong, E.H. Kim et al. Clinical predictors of GH deficiency in surgically cured acromegalic patients. Eur. J. Endocrinol. 171 (2014). https://doi.org/10.1530/EJE-14-0304
A. Spina, M. Losa, P. Mortini pituitary adenomas in elderly patients: clinical and surgical outcome analysis in a large series. Endocrine 65 (2019). https://doi.org/10.1007/s12020-019-01959-0
E.R. Laws, S.L. Iuliano, D.J. Cote et al. A benchmark for preservation of normal pituitary function after endoscopic transsphenoidal surgery for pituitary macroadenomas. World Neurosurg. 91 (2016). https://doi.org/10.1016/j.wneu.2016.04.059
N. Fatemi, J.R. Dusick, C. Mattozo et al. Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 63, 709–718 (2008). https://doi.org/10.1227/01.NEU.0000325725.77132.90
M. Cappelletti, A.G. Ruggeri, L. Spizzichino et al. Fibrous pituitary macroadenomas: predictive role of preoperative radiologic investigations for proper surgical planning in a cohort of 66 patients. World Neurosurg. 121 (2019). https://doi.org/10.1016/j.wneu.2018.09.137
M.M. Gerges, K. Rumalla, S.S. Godil et al. Long-term outcomes after endoscopic endonasal surgery for nonfunctioning pituitary macroadenomas. J. Neurosurg. (2020). https://doi.org/10.3171/2019.11.jns192457
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by C.V.S., C.P.L. and A.P.F. The first draft of the manuscript was written by C.V.S. and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study has been approved by the institutional Ethics Committee.
Informed consent
All patients signed the informed consent for participating in the study and publishing images and data under anonymization.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vivancos Sánchez, C., Palpán Flores, A., Rodríguez Domínguez, V. et al. Role of pituitary stalk and gland radiological status on endocrine function and outcome after endoscopic transsphenoidal surgery for non-functioning pituitary adenomas. Endocrine 73, 416–423 (2021). https://doi.org/10.1007/s12020-021-02726-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02726-w