Abstract
Objectives
Nonfunctionning pituitary macroadenomas (NFPMA) are benign tumors that cause symptoms of mass effects including hypopituitarism. Their primary treatment is transsphenoidal surgery. We aimed to determine the outcome of pituitary hormone deficits after surgical treatment of NFPMA and to identify factors predicting hormonal recovery.
Design
We retrospectively included 246 patients with NFPMA diagnosed and operated in one of the two participating centers. All hormonal axes were evaluated except growth hormone (GH). Postoperative improvement of pituitary endocrine function was considered if at least one hormonal deficit had recovered and a lower total number of deficits was observed 1 year after surgery.
Results
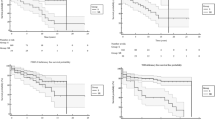
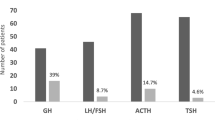
80% (n = 197) of patients had one or more pituitary deficits and 28% had complete anterior hypopituitarism. Besides GH, the gonadotropic and thyrotropic axes were the most commonly affected (68% and 62%, respectively). The number of hypopituitary patients dropped significantly to 61% at 1 year (p < 0.001) and a significant improvement was observed for all hormonal axes, except central diabetes insipidus. Among patients with preoperative hypopituitarism, 88/175 (50%) showed improved pituitary function at 1 year. Both hyperprolactinemia at diagnosis and a lower tumor diameter independently predicted favorable endocrine outcome.
Conclusions
Hypopituitarism is present in 80% of patients with NFPMA and nearly half of them will benefit from sustained improvement after surgery. Hyperprolactinaemia at diagnosis and lower tumor dimensions are associated with favorable endocrine prognosis. This supports the option of early surgery in NFPMA patients with pituitary deficits independent of the presence of visual disturbances.


Similar content being viewed by others
Data availability
Data and code for statistical analyses are available upon request.
References
M.E. Molitch, Diagnosis and treatment of pituitary adenomas. A review. JAMA 317, 516–524 (2017). https://doi.org/10.1001/jama.2016.19699
Y. Greenman, N. Stern, Non-functioning pituitary adenomas. Best. Pract. Res. Clin. Endocrinol. Metab. 23, 625–638 (2009). https://doi.org/10.1016/j.beem.2009.05.005
C.A. Jaffe, Clinically non-functioning pituitary adenoma. Pituitary 9, 317–321 (2006). https://doi.org/10.1007/s11102-006-0412-9
G. Ntali, C. Capatina, V. Fazal-Sanderson, J.V. Byrne, S. Cudlip, A.B. Grossman, J.A. Wass, N. Karavitaki, Mortality in patients with non-functioning pituitary adenoma is increased: systematic analysis of 546 cases with long follow-up. Eur. J. Endocrinol. 174, 137–145 (2016). https://doi.org/10.1530/EJE-15-0967
P. Chanson, G. Raverot, F. Castinetti, C. Cortet-Rudelli, F. Galland, S. Salenave, French Endocrinology Society non-functioning pituitary adenoma work-group. Management of clinically non-functioning pituitary adenoma. Ann. Endocrinol. 76, 239–247 (2015). https://doi.org/10.1016/j.ando.2015.04.002
P.U. Freda, J.N. Bruce, A.G. Khandji, Z. Jin, R.A. Hickman, E. Frey, C. Reyes-Vidal, M. Otten, S.L. Wardlaw, K.D. Post, Presenting features in 269 patients with clinically non functioning pituitary adenomas enrolled in a prospective study. J. Endocr. Soc. 4, 1–13 (2020). https://doi.org/10.1210/jendso/bvaa021
M.R. Drange, N.R. Fram, V. Herman-Bonert, S. Melmed, Pituitary tumor registry: a novel clinical resource. J. Clin. Endocrinol. Metab. 85, 168–174 (2000). https://doi.org/10.1210/jcem.85.1.6309
N. Fatemi, J.R. Dusick, C. Mattozo, D.L. McArthur, P. Cohan, J. Boscardin, C. Wang, R.S. Swerdloff, D.F. Kelly, Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 63, 709–718 (2008). https://doi.org/10.1227/01.NEU.0000325725.77132.90
S.M. Webb, M. Rigla, A. Wägner, B. Oliver, F. Bartumeus, Recovery of hypopituitarism after neurosurgical treatment of pituitary adenomas. J. Clin. Endocrinol. Metab. 84, 3696–3700 (1999). https://doi.org/10.1210/jcem.84.10.6019
O.M. Dekkers, A.M. Pereira, J.A. Romijn, Treatment and follow-up of clinically nonfunctioning pituitary macroadenomas. J. Clin. Endocrinol. Metab. 93, 3717–3726 (2008). https://doi.org/10.1210/jc.2008-0643
G. Raverot, G. Assié, F. Cotton, M. Cogne, A. Boulin, M. Dherbomez, J.F. Bonneville, C. Massart, Biological and radiological exploration and management of non-functioning pituitary adenoma. Ann. Endocrinol. 76, 201–209 (2015). https://doi.org/10.1016/j.ando.2015.04.005
P.U. Freda, A.M. Beckers, L. Katznelson, M.E. Molitch, V.M. Montori, K.D. Post, M.L. Vance, Endocrine Society.Pituitary incidentaloma: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 96, 894–904 (2011). https://doi.org/10.1210/jc.2010-1048
J.W. Lucas, M.E. Bodach, L.M. Tumialan, N.M. Oyesiku, C.G. Patil, Z. Litvack, M.K. Aghi, G. Zada,, Congress of neurological surgeons systematic review and evidence-based guideline on primary management of patients with nonfunctioning pituitary adenomas. Neurosurgery 79, 533–535 (2016). https://doi.org/10.1227/NEU.0000000000001389
P. Mortini, R. Barzaghi, M. Losa, N. Boari, M. Giovanelli, Surgical treatment of giant pituitary adenomas: strategies and results in a series of 95 consecutive patients. Neurosurgery 60, 993–1002 (2007). https://doi.org/10.1227/01.NEU.0000255459.14764.BA
O.M. Dekkers, A.M. Pereira, F. Roelfsema, J.H. Voormolen, K.J. Neelis, M.A. Schroijen, J.W. Smit, J.A. Romijn, Observation alone after transsphenoidal surgery for nonfunctioning pituitary macroadenoma. J. Clin. Endocrinol. Metab. 91, 1796–1801 (2006). https://doi.org/10.1210/jc.2005-2552
D.L. Penn, W.T. Burke, E.R. Laws, Management of non-functioning pituitary adenomas: surgery. Pituitary 21, 145–153 (2018). https://doi.org/10.1007/s11102-017-0854-2
P. Nomikos, C. Ladar, R. Fahlbusch, M. Buchfelder, Impact of primary surgery on pituitary function in patients with non-functioning pituitary adenomas—a study on 721 patients. Acta Neurochir. 146, 27–35 (2004). https://doi.org/10.1007/s00701-003-0174-3
A. Jahangiri, J.R. Wagner, S.W. Han, M.T. Tran, L.M. Miller, R. Chen, M.W. Tom, L.R. Ostling, S. Kunwar, L. Blevins, M.K. Aghi, Improved versus worsened endocrine function after transsphenoidal surgery for non functional pituitary adenomas: rate, time course, and radiological analysis. J. Neurosurg. 124, 589–595 (2016). https://doi.org/10.3171/2015.1.JNS141543
J.H. Kim, J.H. Lee, J.H. Lee, A.R. Hong, Y.J. Kim, Y.H. Kim, Endoscopic transsphenoidal surgery outcomes in 331 nonfunctioning pituitary adenoma cases after a single surgeon learning curve. World Neurosurg. 109, 409–416 (2018). https://doi.org/10.1016/j.wneu.2017.09.194
S. Brochier, F. Galland, M. Kujas, F. Parker, S. Gaillard, C. Raftopoulos, J. Young, O. Alexopoulou, D. Maiter, P. Chanson, Factors predicting relapse of nonfunctioning pituitary macroadenomas after neurosurgery: a study of 142 patients. Eur. J. Endocrinol. 163, 193–200 (2010). https://doi.org/10.1530/EJE-10-0255
L. Persani, G. Brabant, M. Dattani, M. Bonomi, U. Feldt-Rasmussen, E. Fliers, A. Gruters, D. Maiter, N. Schoenmakers, A.S.P. van Trotsenburg, 2018 European Thyroid Association (ETA) guidelines on the diagnosis and management of central hypothyroidism. Eur. Thyroid J. 7, 225–237 (2018). https://doi.org/10.1159/000491388
R. Kazlauskaite, A.T. Evans, C.V. Villabona, T.A.M. Abdu, B. Ambrosi, A.B. Atkinson, C.H. Choi, R.N. Clayton, C.H. Courtney, E.N. Gonc, M. Maghnie, S.R. Rose, D.G. Soule, K. Tordjman, Corticotropin tests for hypothalamic-pituitary- adrenal Insufficiency: a metaanalysis. J. Clin. Endocrinol. Metab. 93, 4245–4253 (2008)
E. Knosp, E. Steiner, K. Kitz, C. Matula, Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33, 610–617 (1993). https://doi.org/10.1227/00006123-199310000-00008
A.S. Micko, A. Wöhrer, S. Wolfsberger, E. Knosp,, Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J. Neurosurg. 122, 803–811 (2015). https://doi.org/10.3171/2014.12.JNS141083
N. Karavitaki, G. Thanabalasingham, H.C. Shore, R. Trifanescu, O. Ansorge, N. Meston, H.E. Turner, J.A. Wass, Do the limits of serum prolactin in disconnection hyperprolactinaemia need re-definition? A study 226 patients histologically verified non-functioning pituitary macroadenoma. Eur. J. Endocrinol. 65, 524–529 (2006). https://doi.org/10.1111/j.1365-2265.2006.02627.x
M.E. Molitch, Nonfunctioning pituitary tumors. Handb. Clin. Neurol. 124, 167–184 (2014). https://doi.org/10.1016/B978-0-444-59602-4.00012-5
B.M. Arafah, Reversible hypopituitarism in patients with large nonfunctioning pituitary adenomas. J. Clin. Endocrinol. Metab. 62, 1173–1179 (1986). https://doi.org/10.1210/jcem-62-6-1173
M. Losa, C.A. Donofrio, R. Barzaghi, P. Mortini, Presentation and surgical results of incidentally discovered nonfunctioning pituitary adenomas: evidence for a better outcome independently of other patients’ characteristics. Eur. J. Endocrinol. 169, 735–742 (2013). https://doi.org/10.1530/EJE-13-0515
R. Zhang, Z. Wang, L. Gao, X. Guo, C. Feng, K. Deng, W. Lian, Y. Yao, M. Feng, X. Bao, R. Wang, B. Xing, Clinical characteristics and postoperative recovery of hypopituitarism in patients with nonfunctional pituitary adenoma. World Neurosurg. 126, 1183–1189 (2019). https://doi.org/10.1016/j.wneu.2019.03.062
M. Marazuela, B. Astigarraga, A. Vicente, J. Estrada, C. Cuerda, J. García-Uría, T. Lucas, Recovery of visual and endocrine function following transsphenoidal surgery of large nonfunctioning pituitary adenomas. J. Endocrinol. Investig. 17, 703–707 (1994). https://doi.org/10.1007/BF03347763
G. Alzhrani, W. Sivakumar, M.S. Park, P. Taussky, W.T. Couldwell, Delayed complications after transsphenoidal surgery for pituitary adenomas. World Neurosurg. 109, 233–241 (2018). https://doi.org/10.1016/j.wneu.2017.09.192
M.H. Murad, M.M. Fernández-Balsells, A. Barwise, J.F. Gallegos-Orozco, A. Paul, M.A. Lane, J.F. Lampropulos, I. Natividad, L. Perestelo-Pérez, P.G. Ponce de León-Lovatón, F.N. Albuquerque, J. Jantey Carey, P.J. Erwin, V.M. Montori, Outcomes of surgical treatment for nonfunctioning pituitary adenomas: a systematic review and meta-analysis. Clin. Endocrinol. 73, 777–791 (2010). https://doi.org/10.1111/j.1365-2265.2010.03875.x
H. Halvorsen, J. Ramm-Pettersen, R. Josefsen, P. Rønning, S. Reinlie, T. Meling, J. Berg-Johnsen, J. Bollerslev, E. Helseth, Surgical complications after transsphenoidal microscopic and endoscopic surgery for pituitary adenoma: a consecutive series of 506 procedures. Acta Neurochir. 156, 441–449 (2014). https://doi.org/10.1007/s00701-013-1959-7
F. Roelfsema, N.R. Biermasz, A.M. Pereira, Clinical factors involved in the recurrence of pituitary adenomas after surgical remission: a structured review and meta-analysis. Pituitary 15, 71–83 (2012). https://doi.org/10.1007/s11102-011-0347-7
R. Comtois, H. Beauregard, M. Somma, O. Serri, N. Aris-Jilwan, J. Hardy, The clinical and endocrine outcome to trans-sphenoidal microsurgery of nonsecreting pituitary adenomas. Cancer 68, 860–866 (1991). https://doi.org/10.1002/1097-0142(19910815)68:4<860::aid-cncr2820680431>3.0.co;2-4
A.T. Nelson Jr, H.S. Tucker Jr, D.P. Becker, Residual anterior pituitary function following transsphenoidal resection of pituitary macroadenomas. J. Neurosurg. 61, 577–580 (1984). https://doi.org/10.3171/jns.1984.61.3.0577
K. I. Lampropoulos, G. Samonis, P. Nomikos, Factors influencing the outcome of microsurgical transsphenoidal surgery for pituitary adenomas: a study on 184 patients. Hormones 12, 254–264 (2013) https://doi.org/10.14310/horm.2002.1409
J.Y. Hwang, D.J. Aum, M.R. Chicoine, R.G. Dacey Jr, J.W. Osbun, K.M. Rich, G.J. Zipfel, C.N. Klatt-Cromwell, J.L. McJunkin, P. Pipkorn, J.S. Schneider, J.M. Silverstein, A.H. Kim, Axis-specific analysis and predictors of endocrine recovery and deficits for non-functioning pituitary adenomas undergoing endoscopic transsphenoidal surgery. Pituitary 23, 389–399 (2020). https://doi.org/10.1007/s11102-020-01045-z
E.P. O’Sullivan, C. Woods, N. Glynn, L.A. Behan, R. Crowley, P. O’Kelly, D. Smith, C.J. Thompson, A. Agha, The natural history of surgically treated but radiotherapy-naïve nonfunctioning pituitary adenomas. Clin. Endocrinol. 71, 709–714 (2009). https://doi.org/10.1111/j.1365-2265.2009.03583.x
E.R. Laws Jr, S.L. Iuliano, D.J. Cote, W. Woodmansee, L. Hsu, C.H. Cho, A benchmark for preservation of normal pituitary function after endoscopic transsphenoidal surgery for pituitary macroadenomas. World Neurosurg. 91, 371–375 (2016). https://doi.org/10.1016/j.wneu.2016.04.059
S. Berkmann, J. Fandino, B. Müller, K.F. Kothbauer, C. Henzen, H. Landolt, Pituitary surgery: experience from a large network in Central Switzerland. Swiss Med. Wkly. 142, w13680 (2012). https://doi.org/10.4414/smw.2012.13680
E. Magro, T. Graillon, J. Lassave, F. Castinetti, S. Boissonneau, E. Tabouret, S. Fuentes, L. Velly, R. Gras, H. Dufour, Complications related to the endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary macroadenomas in 300 consecutive patients. World Neurosurg. 89, 442–453 (2016). https://doi.org/10.1016/j.wneu.2016.02.059
A. Watts, A. Easwaran, P. McNeill, Y.Y. Wang, W. Inder, C. Caputo, Younger age is a risk factor for regrowth and recurrence of nonfunctioning pituitary macroadenomas: Results from a single Australian centre. Clin. Endocrinol. 87, 264–271 (2017). https://doi.org/10.1111/cen.13365. 2017
Acknowledgements
We thank Dr. Sylvie Salenave for her help in the collection of data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Consent for publication
All authors approve the submission.
Ethical approval
The study was approved by the Ethics Committee of the Cliniques Universitaires Saint Luc (UCL) and no informed consent was requested as it was a retrospective study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alexopoulou, O., Everard, V., Etoa, M. et al. Outcome of pituitary hormone deficits after surgical treatment of nonfunctioning pituitary macroadenomas. Endocrine 73, 166–176 (2021). https://doi.org/10.1007/s12020-021-02701-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02701-5