Abstract
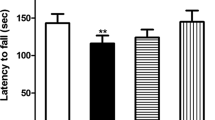
Lead (Pb) toxicity is a worldwide significant public health challenge causing several neurological disorders. Reports indicate that plants rich in antioxidants, such as Rosmarinus officinalis (RO), can counteract Pb accumulation and its toxicity in the brain. Due to a dearth of literature evidence demonstrating the protective activity of RO against Pb toxicity, this study investigated such activity in Wistar rats. Thirty-six Wistar rats were allocated into six groups (n=6), namely I (control), II (lead acetate [Pb]; 100 mg/kg b.w.), III (100 mg/kg of RO and 100 mg/kg of Pb), IV (200 mg/kg of RO and 100 mg/kg of Pb), V (100 mg/kg b.w. of RO) and VI (200 mg/kg b.w. of RO). After 28 days, neurobehavioural, antioxidant, lipid peroxidation, apoptotic and inflammatory activities as well as the histology of the cerebellum were evaluated. Body weight, locomotion and exploration as well as antioxidant enzymes were significantly (p < 0.05) decreased in Pb-exposed rats when compared to control. Conversely, lipid peroxidation, nitric oxide, tumour necrosis factor-alpha and caspase-3 activities were significantly (p < 0.05) upregulated in the Pb-exposed rats when compared to control. These parameters were, however, significantly (p<0.05) attenuated in the RO-pretreated rats when compared to Pb-exposed rats. Cerebellar histology of the Pb-exposed rats showed severe degeneration of the Purkinje cells whereas the RO-pretreated rats showed better cerebellar architecture. These findings demonstrate that the neuroprotective activity of RO is facilitated via its effective antioxidant, anti-inflammatory and anti-apoptotic effects.





Similar content being viewed by others
Data Availability
The datasets for study are available from the corresponding author on reasonable request.
References
World Health Organization W (2010) Childhood lead poisoning https://wwwwhoint/news-room/fact-sheets/detail/lead-poisoning-and-health.
Ab Latif Wani A, Usmani J (2015) Lead toxicity: a review. Interdiscip Toxicol 8:55–64
Sridevi Sangeetha K, Umamaheswari S (2020) Human exposure to lead, mechanism of toxicity and treatment strategy-a review. J Clin Diagn Res 14(12)
Sarkar O, Dey KK, Islam S, Chattopadhyay A (2022) Lead and aquatic ecosystems, biomarkers, and implications for humankind. In: Biomarkers in Toxicology. Springer, pp 1–28
Kumar P, Singh R, Nazmi A, Lakhanpal D, Kataria H, Kaur G (2014) Glioprotective effects of Ashwagandha leaf extract against lead induced toxicity. Biomed Res Int 2014
Sharma P, Chambial S, Shukla KK (2015) Lead and neurotoxicity. Indian J Clin Biochem 30(1):1–2
Sanders T, Liu Y, Buchner V, Tchounwou PB (2009) Neurotoxic effects and biomarkers of lead exposure: a review. Rev Environ Health 24(1):15–46
Xu D-P, Li Y, Meng X, Zhou T, Zhou Y, Zheng J et al (2017) Natural antioxidants in foods and medicinal plants: extraction, assessment and resources. Int J Mol Sci 18(1):96
Lobo V, Patil A, Phatak A, Chandra N (2010) Free radicals, antioxidants and functional foods: impact on human health. Pharmacogn Rev 4(8):118
Yuan H, Ma Q, Ye L, Piao G (2016) The traditional medicine and modern medicine from natural products. Molecules 21(5):559
Enogieru A, Momodu O (2021) The developing cerebellum as a target for toxic substances: protective role of antioxidants. The Cerebellum:1–17
De Oliveira JR, Camargo SEA, De Oliveira LD (2019) Rosmarinus officinalis L.(rosemary) as therapeutic and prophylactic agent. J Biomed Sci 26(1):1–22
Habtemariam S (2016) The therapeutic potential of rosemary (Rosmarinus officinalis) diterpenes for Alzheimer’s disease. Evid Based Complement Alternat Med 2016
UK Food Standards Agency U (2011) Current EU approved additives and their E Numbers https://wwwfoodgovuk/business-guidance/approved-additives-and-e-numbers.
Rahbardar MG, Hosseinzadeh H (2020) Therapeutic effects of rosemary (Rosmarinus officinalis L.) and its active constituents on nervous system disorders. Iran J Basic Med Sci 23(9):1100
Rašković A, Milanović I, Pavlović N, Ćebović T, Vukmirović S, Mikov M (2014) Antioxidant activity of rosemary (Rosmarinus officinalis L.) essential oil and its hepatoprotective potential. BMC Complement Altern Med 14(1):1–9
Ngo SN, Williams DB, Head RJ (2011) Rosemary and cancer prevention: preclinical perspectives. Crit Rev Food Sci Nutr 51(10):946–954
Ezeigwe OC, Nzekwe FA, Nworji OF, Ezennaya CF, Iloanya EL, Asogwa KK (2020) Effect of aqueous extract of F. capensis leaves and its combination with C. aconitifolius leaves on essential biochemical parameters of phenylhydrazine-induced anemic rats. J Exp Pharmacol 12:191–201
Sofowora A (1993) Phytochemical screening of medicinal plants and traditional medicine in Africa. Spectrum Books Limited, Nigeria, pp 150–156
Trease G, Evans W (1983) Text book of Pharmacognosy London Bailliare Tindall 12(193):336.
Senguttuvan J, Paulsamy S, Karthika K (2014) Phytochemical analysis and evaluation of leaf and root parts of the medicinal herb, Hypochaeris radicata L. for in vitro antioxidant activities. Asian Pac J Trop Biomed 4:S359–SS67
Lorke D (1983) A new approach to practical acute toxicity testing. Arch Toxicol 54(4):275–287
Enogieru A, Omoruyi S (2022) Exploration of aqueous Phyllanthus amarus leaf extract as a protective agent in mercury chloride-exposed Wistar rats: a neurobehavioural study. J Appl Sci Environ Manag 26(4):629–637
Enogieru A, Momodu O (2022) Neuroprotective effects of Zingiber officinale against lead-induced toxicity in Wistar rats. Nutrire 48(1):2
Kim H-J, Kong M-K, Kim Y-C (2008) Beneficial effects of Phellodendri Cortex extract on hyperglycemia and diabetic nephropathy in streptozotocin-induced diabetic rats. BMB Rep 41(10):710–715
Guttridge J, Wilkins C (1982) Copper dependent hydroxyl radical damage to ascorbic acid. Formation of thiobarbituric acid reactive products. FEBS Lett 137:327–340
Cohen G, Dembiec D, Marcus J (1970) Measurement of catalase activity in tissue extracts. Anal Biochem 34(1):30–38
Misra HP, Fridovich I (1972) The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. J Biol Chem 247(10):3170–3175
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82(1):70–77
Nyman M (1959) Serum hatoglobin; methodological and clinical studies. Scand J Clin Lab Invest 11:1–169
Montogomery H, Dymock J (1961) The determination of nitrite in water: colorimetric method of nitric oxide assay. Analyst 86:414
Koracevic D, Koracevic G, Djordjevic V, Andrejevic S, Cosic V (2001) Method for the measurement of antioxidant activity in human fluids. J Clin Pathol 54(5):356–361
Drury R, Wallington E (1980) Carleton’s histological technique, 5th edn. Churchill Livingstone, New York
Rafique M, Perveen K, Khan N, Nigar S (2008) Lead intoxication causing loss of body weight and loss of absolute weight of testes in albino rats. Hamdard Med 51:123–128
Amjad Z, Iqbal M, Shoro A (2013) Lead-induced reduction in body and kidney weight of Wistar albino rats ameliorated by Ginkgo biloba extract (EGb 761). Biochem Physiol 2(113):2
van Berlo D, Woutersen M, Muller A, Pronk M, Vriend J, Hakkert B (2022) 10% Body weight (gain) change as criterion for the maximum tolerated dose: a critical analysis. Regul Toxicol Pharmacol 134:105235
Klaassen CD (2006) Heavy metals and heavy-metal antagonists Goodman and Gilman’s the pharmacological basis of therapeutics, 11th edn. McGraw-Hill, New York, pp 1753–1775
Cecil KM, Brubaker CJ, Adler CM, Dietrich KN, Altaye M, Egelhoff JC et al (2008) Decreased brain volume in adults with childhood lead exposure. PLoS Med 5(5):e112
Stewart W, Schwartz B, Davatzikos C, Shen D, Liu D, Wu X et al (2006) Past adult lead exposure is linked to neurodegeneration measured by brain MRI. Neurology 66(10):1476–1484
Kraeuter A-K, Guest PC, Sarnyai Z (2019) The open field test for measuring locomotor activity and anxiety-like behavior. In: Pre-clinical models: techniques and protocols, pp 99–103
Davies KG, Ekpennyong C, Green O, Antai A, Osim E (2013) Locomotor and exploratory behaviour in mice treated with oral artesunate. British Journal of Science 8(1):47–57
Owoeye O, Onwuka SK (2016) Lead toxicity: effect of Launaea taraxacifolia on the histological and oxidative alterations in Rat Regio III Cornu ammonis and cerebellum. Anatomy Journal of Africa 5(1):783–794
Kalueff AV, Stewart AM, Song C, Berridge KC, Graybiel AM, Fentress JC (2016) Neurobiology of rodent self-grooming and its value for translational neuroscience. Nat Rev Neurosci 17(1):45–59
Berridge KC, Whishaw IQ (1992) Cortex, striatum and cerebellum: control of serial order in a grooming sequence. Exp Brain Res 90:275–290
Watson P (1978) Behavior maintained by electrical stimulation of the rat cerebellum. Physiol Behav 21(5):749–755
Amel B, Omar K, Faiza F, Miloud S, Abdelkader A (2016) Behavior and glutamate transaminase changes in rat exposed to lead and treated by wormwood extract. Int J Pharm Pharm 8:208–213
Enogieru A, Egbon F (2022) Neurobehavioural and histological alterations in lead acetate-exposed rats pretreated with aqueous leaf extract of Vernonia amygdalina. Afr J Biomed Res 25(2):205–213
Roelofs K (2017) Freeze for action: neurobiological mechanisms in animal and human freezing. Philos Trans R Soc B: Biol Sci 372(1718):20160206
Apps R, Strata P (2015) Neuronal circuits for fear and anxiety—the missing link. Nat Rev Neurosci 16(10):642
Koutsikou S, Crook JJ, Earl EV, Leith JL, Watson TC, Lumb BM et al (2014) Neural substrates underlying fear-evoked freezing: the periaqueductal grey–cerebellar link. J Physiol 592(10):2197–2213
Vaaga CE, Brown ST, Raman IM (2020) Cerebellar modulation of synaptic input to freezing-related neurons in the periaqueductal gray. elife 9:e54302
Sacchetti B, Scelfo B, Tempia F, Strata P (2004) Long-term synaptic changes induced in the cerebellar cortex by fear conditioning. Neuron 42(6):973–982
Udefa AL, Amama EA, Archibong EA, Nwangwa JN, Adama S, Inyang VU et al (2020) Antioxidant, anti-inflammatory and anti-apoptotic effects of hydro-ethanolic extract of Cyperus esculentus L.(tigernut) on lead acetate-induced testicular dysfunction in Wistar rats. Biomed Pharmacother 129:110491
El-Nekeety AA, El-Kady AA, Soliman MS, Hassan NS, Abdel-Wahhab MA (2009) Protective effect of Aquilegia vulgaris (L.) against lead acetate-induced oxidative stress in rats. Food Chem Toxicol 47(9):2209–2215
Weydert CJ, Cullen JJ (2010) Measurement of superoxide dismutase, catalase and glutathione peroxidase in cultured cells and tissue. Nat Protoc 5(1):51–66
Ighodaro O, Akinloye O (2018) First line defence antioxidants-superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): their fundamental role in the entire antioxidant defence grid. Alexandria J Med 54(4):287–293
Fan Y, Zhao X, Yu J, Xie J, Li C, Liu D et al (2020) Lead-induced oxidative damage in rats/mice: a meta-analysis. J Trace Elem Med Biol 58:126443
Hamadouche NA, Lazeb H, Kaddouri A, Guellil H, Slimani M, Aoues A (2015) Ameliorated effects of green tea extract on lead induced kidney toxicity in rats Algerian. J Nat Prod 3:130–137
Jozefczak M, Remans T, Vangronsveld J, Cuypers A (2012) Glutathione is a key player in metal-induced oxidative stress defenses. Int J Mol Sci 13(3):3145–3175
Shaban NZ, Abd El-Kader SE, Mogahed FA, El-Kersh MA, Habashy NH (2021) Synergistic protective effect of Beta vulgaris with meso-2, 3-dimercaptosuccinic acid against lead-induced neurotoxicity in male rats. Sci Rep 11(1):252
Ito F, Sono Y, Ito T (2019) Measurement and clinical significance of lipid peroxidation as a biomarker of oxidative stress: oxidative stress in diabetes, atherosclerosis, and chronic inflammation. Antioxidants 8(3):72
Shahid M, Khalid S, Abbas G, Shahid N, Nadeem M, Sabir M et al (2015) Heavy metal stress and crop productivity. In: Crop production and global environmental issues. Springer, Cham, pp 1–25
Oyem JC, Chris-Ozoko LE, Enaohwo MT, Otabor FO, Okudayo VA, Udi OA (2021) Antioxidative properties of Ocimum gratissimum alters lead acetate induced oxidative damage in lymphoid tissues and hematological parameters of adult Wistar rats. Toxicol Rep 8:215–222
Kumar Singh P, Kumar Singh M, Singh Yadav R, Kumar Dixit R, Mehrotra A, Nath R (2018) Attenuation of lead-induced neurotoxicity by omega-3 fatty acid in rats. Ann Neurosci 24(4):221–232
Gąssowska-Dobrowolska M, Chlubek M, Kolasa A, Tomasiak P, Korbecki J, Skowrońska K et al (2023) Microglia and astroglia—the potential role in neuroinflammation induced by pre-and neonatal exposure to lead (Pb). Int J Mol Sci 24(12):9903
Zelickson B, Ballinger S, Dell’Italia L, Zhang J, Darley-Usmar V (2013) Reactive oxygen and nitrogen species: interactions with mitochondria and pathophysiology.
Lubos E, Handy DE, Loscalzo J (2008) Role of oxidative stress and nitric oxide in atherothrombosis. Front Biosci 13:5323
Kuhad A, Chopra K (2007) Curcumin attenuates diabetic encephalopathy in rats: behavioral and biochemical evidences. Eur J Pharmacol 576(1-3):34–42
Baty RS, Hassan K, Alsharif KF, El-Hennamy R, Elmahallawy E, Hafez M et al (2020) Neuroprotective role of luteolin against lead acetate-induced cortical damage in rats. Hum Exp Toxicol 39(9):1200–1212
Othman MS, Obeidat ST, Aleid GM, Abdel-Daim MM, Habotta OA, Schwartz L et al (2022) Pergularia tomentosa coupled with selenium nanoparticles salvaged lead acetate-induced redox imbalance, inflammation, apoptosis, and disruption of neurotransmission in rats’ brain. Open Chemistry 20(1):1313–1326
Kannan K, Jain SK (2000) Oxidative stress and apoptosis. s 7(3):153–163
El-Tantawy WH (2016) Antioxidant effects of Spirulina supplement against lead acetate-induced hepatic injury in rats. J Tradit Complement Med 6(4):327–331
Galal MK, Elleithy EM, Abdrabou MI, Yasin NA, Shaheen YM (2019) Modulation of caspase-3 gene expression and protective effects of garlic and spirulina against CNS neurotoxicity induced by lead exposure in male rats. Neurotoxicology 72:15–28
Wang C, Youle RJ (2009) The role of mitochondria in apoptosis. Annu Rev Genet 43:95–118
Augustine I, Gertrude O, Martin E, Obinna U, Uchenna E, Ogugua E (2021) Cerebellar and hypocampal changes induced by lead in Wistar rats: the role of Ocimium gratissimium leaves extract J Bio. Med Sci 10(3):56
Ajibade A, Ogundero S (2021) Neurohistological changes in the cerebellar cortex of adult Wistar rats following lead acetate induced cortical damage. GSC Biol Pharm Sci 15(3):182–188
Funding
This work was funded by the TETfund Institutional Based Research Fund (2021/2022).
Author information
Authors and Affiliations
Contributions
Adaze Bijou Enogieru conceived, designed and analysed the study. Nathan Etinosa Iyoha performed the experiments. The first draft of the manuscript was written by Adaze Bijou Enogieru. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the College of Medical Sciences, University of Benin (CMS/REC/2021/172).
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Enogieru, A.B., Iyoha, E.N. Role of Nitric Oxide, TNF–α and Caspase-3 in Lead Acetate-Exposed Rats Pretreated with Aqueous Rosmarinus officinalis Leaf Extract. Biol Trace Elem Res (2023). https://doi.org/10.1007/s12011-023-03974-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12011-023-03974-9