Abstract
Objective
Baicalin (BC) is a flavonoid reported to have various pharmacological activities, including antioxidant, anti-cancer, anti-inflammatory, anti-allergy, immune regulation, and anti-diabetic. This study examines the probable mechanism for gestational diabetes mellitus (GDM) brought on by streptozotocin (STZ) and the impact of BC on fetal development via AGEs (advanced serum glycation end products) and RAGE (the role of advanced glycation end products).
Material and Method
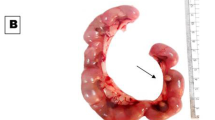
STZ has been used in the current experimental study to induce diabetes mellitus in pregnant animals (gestational diabetes mellitus). GDM pregnant animals were separated into five groups and were treated with BC in a dose-dependent pattern for 19 days. At the end of the experiment, the fetus and blood samples were drawn from all the pregnant rats to assess the biochemical parameter as well as AGE-RAGE.
Result
Administration of BC at varying doses leads to enhancement in the weight of the fetus body and placenta while gestational diabetic pregnant animals induced by STZ had a lower weight of the fetus body and placenta. The dose-dependent pattern of BC also enhanced fasting insulin (FINS), high-density lipoprotein (HDL), serum insulin, and hepatic glycogen. It also significantly enhanced the content of the antioxidant profile and pro-inflammatory cytokines and modulated the gene expression (VCAM- 1, p65, EGFR, MCP-1, 1NOX2, and RAGE) in various tissues in gestational diabetes mellitus pregnant rats.
Conclusion
Baicalin demonstrated the potential impact on the embryo’s development via the AGE-RAGE signaling pathway in STZ-induced GDM pregnant animals.
Graphical Abstract










Similar content being viewed by others
Data Availability
All data is available.
Abbreviations
- BC :
-
Baicalin
- STZ :
-
Streptozotocin
- T2DM :
-
Type 2 diabetes mellitus
- GDM :
-
Gestational diabetes mellitus
- SOD :
-
Superdioxide mutase
- CAT :
-
Catalase
- RT-PCR :
-
Real-time polymerase chain reaction
- GPx :
-
Glutathione peroxidase
- GST :
-
Glutathione S-transferase
- AGE :
-
Advanced glycation end products
- RAGE :
-
Receptor for advanced glycation end products
- NC :
-
Normal control
- PC :
-
Positive control
- ROS :
-
Reactive oxygen species
- LPO :
-
Lipid peroxidation
References
Buchanan, T. A., Xiang, A. H., & Page, K. A. (2012). Gestational diabetes mellitus: Risks and management during and after pregnancy. Nature Reviews Endocrinology, 8(11), 639–649. https://doi.org/10.1038/nrendo.2012.96
Tikkanen, M. (2011). Placental abruption: Epidemiology, risk factors and consequences: Placental abruption, epidemiology. Acta Obstetricia et Gynecologica Scandinavica, 90(2), 140–149. https://doi.org/10.1111/j.1600-0412.2010.01030.x
Tozour, J., Hughes, F., Carrier, A., Vieau, D., & Delahaye, F. (2020). Prenatal Hyperglycemia Exposure and Cellular Stress, a Sugar-Coated View of Early Programming of Metabolic Diseases. Biomolecules, 10(10), 1359. https://doi.org/10.3390/biom10101359
Castori, M. (2013). Diabetic Embryopathy: A Developmental Perspective from Fertilization to Adulthood. Molecular Syndromology, 4(1–2), 74–86. https://doi.org/10.1159/000345205
Petersen, M. C., & Shulman, G. I. (2018). Mechanisms of Insulin Action and Insulin Resistance. Physiological Reviews, 98(4), 2133–2223. https://doi.org/10.1152/physrev.00063.2017
Tunduguru, R., & Thurmond, D. C. (2017). Promoting Glucose Transporter-4 Vesicle Trafficking along Cytoskeletal Tracks: PAK-Ing Them Out. Frontiers in Endocrinology, 8, 329. https://doi.org/10.3389/fendo.2017.00329
Giacco, F., & Brownlee, M. (2010). Oxidative Stress and Diabetic Complications. Circulation Research, 107(9), 1058–1070. https://doi.org/10.1161/CIRCRESAHA.110.223545
Zhao, Q., Chen, X.-Y., & Martin, C. (2016). Scutellaria baicalensis, the golden herb from the garden of Chinese medicinal plants. Science Bulletin, 61(18), 1391–1398. https://doi.org/10.1007/s11434-016-1136-5
Fang, D. N., Zheng, C. W., & Ma, Y. L. (2023). Effectiveness of Scutellaria baicalensis Georgi root in pregnancy-related diseases: A review. Journal of Integrative Medicine, 21(1), 17–25. https://doi.org/10.1016/j.joim.2022.09.005
Wang, G., Lu, J. Q., Ding, Y., Zhang, T., Song, J. H., Long, D., Liang, J., Cheng, X., Si, Z., Qi, G., Jiang, X., & Yang, X. (2020). Baicalin rescues hyperglycemia-induced neural tube defects via targeting on retinoic acid signaling. American Journal of Translational Research, 12(7), 3311–3328.
Wang, G., Liang, J., Gao, L. R., Si, Z. P., Zhang, X. T., Liang, G., Yan, Y., Li, K., Cheng, X., Bao, Y., Chuai, M., Chen, L. G., Lu, D. X., & Yang, X. (2018). Baicalin administration attenuates hyperglycemia-induced malformation of cardiovascular system. Cell Death & Disease, 9(2), 234. https://doi.org/10.1038/s41419-018-0318-2
Li, J., Wang, Y., Wu, T., Li, S., Sun, Y. N., & Liu, Z. H. (2022). Baicalein suppresses high glucose-induced inflammation and apoptosis in trophoblasts by targeting the miRNA-17-5p-Mfn1/2-NF-κB pathway. Placenta, 121, 126–136. https://doi.org/10.1016/j.placenta.2022.02.013
Ma, P., Mao, X.-Y., Li, X.-L., Ma, Y., Qiao, Y.-D., Liu, Z.-Q., … Cao, Y.-G. (2015). Baicalin alleviates diabetes-associated cognitive deficits via modulation of mitogen-activated protein kinase signaling, brain-derived neurotrophic factor and apoptosis. Molecular Medicine Reports, 12(4), 6377–6383. https://doi.org/10.3892/mmr.2015.4219
Ma, L., Wu, F., Shao, Q., Chen, G., Xu, L., & Lu, F. (2021). Baicalin Alleviates Oxidative Stress and Inflammation in Diabetic Nephropathy via Nrf2 and MAPK Signaling Pathway. Drug Design, Development and Therapy, 15, 3207–3221. https://doi.org/10.2147/DDDT.S319260
Yang, M., Kan, L., Wu, L., Zhu, Y., & Wang, Q. (2019). Effect of baicalin on renal function in patients with diabetic nephropathy and its therapeutic mechanism. Experimental and Therapeutic Medicine. https://doi.org/10.3892/etm.2019.7181
Xu, W., Tang, M., Wang, J., & Wang, L. (2020). Anti-inflammatory activities of puerarin in high-fat diet-fed rats with streptozotocin-induced gestational diabetes mellitus. Molecular Biology Reports, 47(10), 7537–7546. https://doi.org/10.1007/s11033-020-05816-6
Tian, Z.-H., Miao, F.-T., Zhang, X., Wang, Q.-H., Lei, N., & Guo, L.-C. (2015). Therapeutic effect of okra extract on gestational diabetes mellitus rats induced by streptozotocin. Asian Pacific Journal of Tropical Medicine, 8(12), 1038–1042. https://doi.org/10.1016/j.apjtm.2015.11.002
Wang, Y., Wang, L., Xu, G., & Wei, D. (2019). Hesperidin Exerts the Gestational Diabetes Mellitus via AGEs-RAGE Signalling Pathway. International Journal of Pharmacology, 15(5), 604–615. https://doi.org/10.3923/ijp.2019.604.615
Tang, X., Qin, Q., Xie, X., & He, P. (2015). Protective Effect of sRAGE on Fetal Development in Pregnant Rats with Gestational Diabetes Mellitus. Cell Biochemistry and Biophysics, 71(2), 549–556. https://doi.org/10.1007/s12013-014-0233-9
Dai, S., Meng, X., Cai, X., Yuan, C., Zhao, Z., Zhong, L., … Yin, F. (2021). Therapeutic effect of ursolic acid on fetal development in pregnant rats with gestational diabetes mellitus via AGEs‐RAGE signaling pathway. Journal of Food Biochemistry, 45(4). https://doi.org/10.1111/jfbc.13651
Plows, J., Stanley, J., Baker, P., Reynolds, C., & Vickers, M. (2018). The Pathophysiology of Gestational Diabetes Mellitus. International Journal of Molecular Sciences, 19(11), 3342. https://doi.org/10.3390/ijms19113342
Alejandro, E. U., Mamerto, T. P., Chung, G., Villavieja, A., Gaus, N. L., Morgan, E., & Pineda-Cortel, M. R. B. (2020). Gestational Diabetes Mellitus: A Harbinger of the Vicious Cycle of Diabetes. International Journal of Molecular Sciences, 21(14), 5003. https://doi.org/10.3390/ijms21145003
Tanase-Nakao, K., Arata, N., Kawasaki, M., Yasuhi, I., Sone, H., Mori, R., & Ota, E. (2017). Potential protective effect of lactation against incidence of type 2 diabetes mellitus in women with previous gestational diabetes mellitus: A systematic review and meta-analysis. Diabetes/Metabolism Research and Reviews, 33(4), e2875. https://doi.org/10.1002/dmrr.2875
Kumar, V., Ahmed, D., Verma, A., Anwar, F., Ali, M., & Mujeeb, M. (2013). Umbelliferone β-D-galactopyranoside from Aegle marmelos (L.) corr. an ethnomedicinal plant with antidiabetic, antihyperlipidemic and antioxidative activity. BMC Complementary and Alternative Medicine, 13(1), 273. https://doi.org/10.1186/1472-6882-13-273
Menon, V. B., Kurian, J., Undela, K., Ramesh, M., & Gowdappa, H. B. (2015). Phenytoin Toxicity: A Case Report. Journal of Young Pharmacists, 7(3), 272–275. https://doi.org/10.5530/jyp.2015.3.20
Vargesson, N. (2015). Thalidomide-induced teratogenesis: History and mechanisms. Birth Defects Research Part C: Embryo Today: Reviews, 105(2), 140–156. https://doi.org/10.1002/bdrc.21096
Volpe, C. M. O., Villar-Delfino, P. H., dos Anjos, P. M. F., & Nogueira-Machado, J. A. (2018). Cellular death, reactive oxygen species (ROS) and diabetic complications. Cell Death & Disease, 9(2), 119. https://doi.org/10.1038/s41419-017-0135-z
Vambergue, A., & Fajardy, I. (2011). Consequences of gestational and pregestational diabetes on placental function and birth weight. World Journal of Diabetes, 2(11), 196. https://doi.org/10.4239/wjd.v2.i11.196
Mythili, M. D., Vyas, R., Akila, G., & Gunasekaran, S. (2004). Effect of streptozotocin on the ultrastructure of rat pancreatic islets. Microscopy Research and Technique, 63(5), 274–281. https://doi.org/10.1002/jemt.20039
Farid, M. M., Aboul Naser, A. F., Salem, M. M., Ahmed, Y. R., Emam, M., & Hamed, M. A. (2022). Chemical compositions of Commiphora opobalsamum stem bark to alleviate liver complications in streptozotocin-induced diabetes in rats: Role of oxidative stress and DNA damage. Biomarkers, 1–13. https://doi.org/10.1080/1354750X.2022.2099015
Nurdiana, S., Goh, Y. M., Ahmad, H., Dom, S. M., Syimal’ain Azmi, N., Noor Mohamad Zin, N. S., & Ebrahimi, M. (2017). Changes in pancreatic histology, insulin secretion and oxidative status in diabetic rats following treatment with Ficus deltoidea and vitexin. BMC Complementary and Alternative Medicine, 17(1), 290.https://doi.org/10.1186/s12906-017-1762-8
Smirnov, A. V., Snigur, G. L., & Voronkov, M. P. (2012). Pancreatic Islet Beta-Cell Apoptosis in Experimental Diabetes Mellitus. In T. Ntuli (Ed.), Apoptosis and Medicine. InTech. https://doi.org/10.5772/51411
Chen, G., Chen, X., Niu, C., Huang, X., An, N., Sun, J., … Jin, L. (2019). Baicalin alleviates hyperglycemia-induced endothelial impairment via Nrf2. Journal of Endocrinology, 240(1), 81–98. https://doi.org/10.1530/JOE-18-0457
Ku, S.-K., & Bae, J.-S. (2015). Baicalin, baicalein and wogonin inhibits high glucose-induced vascular inflammation in vitro and in vivo. BMB Reports, 48(9), 519–524. https://doi.org/10.5483/BMBRep.2015.48.9.017
Tsalamandris, S., Antonopoulos, A. S., Oikonomou, E., Papamikroulis, G.-A., Vogiatzi, G., Papaioannou, S., … Tousoulis, D. (2019). The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. European Cardiology Review, 14(1), 50–59. https://doi.org/10.15420/ecr.2018.33.1
Zhang, R., Zhang, X., Xing, B., Zhao, J., Zhang, P., Shi, D., & Yang, F. (2019). Astragaloside IV attenuates gestational diabetes mellitus via targeting NLRP3 inflammasome in genetic mice. Reproductive Biology and Endocrinology, 17(1), 77. https://doi.org/10.1186/s12958-019-0522-7
Fang, P., Yu, M., Zhang, L., Wan, D., Shi, M., Zhu, Y., … Zhang, Z. (2017). Baicalin against obesity and insulin resistance through activation of AKT/AS160/GLUT4 pathway. Molecular and Cellular Endocrinology, 448, 77–86. https://doi.org/10.1016/j.mce.2017.03.027
Rask-Madsen, C., & King, G. L. (2013). Vascular Complications of Diabetes: Mechanisms of Injury and Protective Factors. Cell Metabolism, 17(1), 20–33. https://doi.org/10.1016/j.cmet.2012.11.012
Safi, S. Z., Qvist, R., Kumar, S., Batumalaie, K., & Ismail, I. S. B. (2014). Molecular Mechanisms of Diabetic Retinopathy, General Preventive Strategies, and Novel Therapeutic Targets. BioMed Research International, 2014, 1–18. https://doi.org/10.1155/2014/801269
Twarda-Clapa, A., Olczak, A., Białkowska, A. M., & Koziołkiewicz, M. (2022). Advanced Glycation End-Products (AGEs): Formation, Chemistry, Classification, Receptors, and Diseases Related to AGEs. Cells, 11(8), 1312. https://doi.org/10.3390/cells11081312
Yan, S. F., Ramasamy, R., & Schmidt, A. M. (2009). The receptor for advanced glycation endproducts (RAGE) and cardiovascular disease. Expert Reviews in Molecular Medicine, 11, e9. https://doi.org/10.1017/S146239940900101X
Singh, V. P., Bali, A., Singh, N., & Jaggi, A. S. (2014). Advanced Glycation End Products and Diabetic Complications. The Korean Journal of Physiology & Pharmacology, 18(1), 1. https://doi.org/10.4196/kjpp.2014.18.1.1
Ramasamy, R., Yan, S. F., & Schmidt, A. M. (2012). Advanced glycation endproducts: From precursors to RAGE: Round and round we go. Amino Acids, 42(4), 1151–1161. https://doi.org/10.1007/s00726-010-0773-2
AL-Ishaq, Abotaleb, Kubatka, Kajo, & Büsselberg. (2019). Flavonoids and Their Anti-Diabetic Effects: Cellular Mechanisms and Effects to Improve Blood Sugar Levels. Biomolecules, 9(9), 430.https://doi.org/10.3390/biom9090430
Shi, J., Wu, G., Zou, X., & Jiang, K. (2019). Enteral Baicalin, a Flavone Glycoside, Reduces Indicators of Cardiac Surgery-Associated Acute Kidney Injury in Rats. Cardiorenal Medicine, 9(1), 31–40. https://doi.org/10.1159/000492159
Vafaei-Pour, Z., Shokrzadeh, M., Jahani, M., & Shaki, F. (2018). Embryo-Protective Effects of Cerium Oxide Nanoparticles against Gestational Diabetes in Mice. Iranian journal of pharmaceutical research: IJPR, 17(3), 964–975.
Holemans, K., Caluwaerts, S., Poston, L., & Van Assche, F. A. (2004). Diet-induced obesity in the rat: A model for gestational diabetes mellitus. American Journal of Obstetrics and Gynecology, 190(3), 858–865. https://doi.org/10.1016/j.ajog.2003.09.025
Liu, B., Xu, Y., Voss, C., Qiu, F., Zhao, M., Liu, Y., … Wang, Z. (2012). Altered Protein Expression in Gestational Diabetes Mellitus Placentas Provides Insight into Insulin Resistance and Coagulation/Fibrinolysis Pathways. PLoS One, 7(9), e44701. https://doi.org/10.1371/journal.pone.0044701
Nowotny, K., Jung, T., Höhn, A., Weber, D., & Grune, T. (2015). Advanced Glycation End Products and Oxidative Stress in Type 2 Diabetes Mellitus. Biomolecules, 5(1), 194–222. https://doi.org/10.3390/biom5010194
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SQ, XW, and QW: data curation, formal analysis, writing original data, review, and editing; XJ, RR, and XL: formal analysis, conceptualization, project administration, investigation, and methodology. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Consent to Participate
The authors have the consent to participate.
Consent to Publish
The authors have the consent to publish.
Competing interests
The authors declare no competing of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Practical Application
It is well known that the prevalence of gestational diabetes is rising globally. Baicalin is traditional Chinese medicine and is used in diabetes management. The present study describes the potential effect of baicalin on gestational diabetes mellitus in pregnant animals via an underlying probable mechanism. The result also supported the efficacy of BC in GDM rats in a dose-dependent manner via improving biochemical analysis, inflammation and oxidative stress, and the AGE-RAGE signaling pathway. We can conclude from the findings that baicalin may be a protective medication for the management of gestational diabetes mellitus.
Statement of Novelty
Our results suggest the efficacy of baicalin in gestational diabetes mellitus rats. It increases the weight of the fetus’s body and placenta. It also elevates the level of lipid profile, serum, and glycogen in a dose-dependent manner. It was also found effective in increasing the antioxidant parameter and inflammatory profile and attenuating the gene expression via AGE and RAGE signaling pathways. It can be used in clinical trials and lead to technology transfer for the welfare of the society in the management of diabetes mellitus.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qiu, S., Wu, X., Wu, Q. et al. Pharmacological Action of Baicalin on Gestational Diabetes Mellitus in Pregnant Animals Induced by Streptozotocin via AGE-RAGE Signaling Pathway. Appl Biochem Biotechnol 196, 1636–1651 (2024). https://doi.org/10.1007/s12010-023-04586-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12010-023-04586-8