Abstract
Purpose of Review
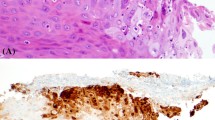
Esophageal diseases are a common manifestation of HIV infection, and in some cases may be the first presentation of an underlying, severely immunocompromised state. The esophagus may be the site of the first acquired immunodeficiency syndrome (AIDS)–defining opportunistic illness in a large number of patients, and this review highlights varying clinical presentations and symptoms of esophageal diseases in HIV.
Recent Findings
Infective esophagitis often signals the onset of symptomatic HIV infection and endoscopic evaluation with biopsies is instrumental in their diagnosis and management. As esophageal diseases in HIV are present, there is notable advancement in the diagnostic approach and pharmacotherapeutics.
Summary
This review briefly highlights various esophageal diseases related to underlying HIV infection and outlines recent updates in diagnosis, management, and available treatment options.








Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
López-Dupla M, Mora Sanz P, PintadoGarcía V, et al. Clinical, endoscopic, immunologic, and therapeutic aspects of oropharyngeal and esophageal candidiasis in HIV-infected patients: a survey of 114 cases. Am J Gastroenterol. 1992;87(12):1771–6.
Takahashi Y, Nagata N, Shimbo T, et al. Long-term trends in esophageal candidiasis prevalence and associated risk factors with or without HIV infection: lessons from an endoscopic study of 80,219 patients. PLoS One. 2015;10(7):e0133589. https://doi.org/10.1371/journal.pone.0133589. (Published 2015 Jul 24).
Pons V, Greenspan D, Lozada-Nur F, et al. Oropharyngeal candidiasis in patients with AIDS: randomized comparison of fluconazole versus nystatin oral suspensions. Clin Infect Dis. 1997;24(6):1204–7. https://doi.org/10.1086/513664.
Vazquez JA. Optimal management of oropharyngeal and esophageal candidiasis in patients living with HIV infection. HIV AIDS (Auckl). 2010;2:89–101. https://doi.org/10.2147/hiv.s6660.
Benson CA, Kaplan JE, Masur H, et al. Treating opportunistic infections among HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America [published correction appears in MMWR Morb Mortal Wkly Rep. 2005 Apr 1;54(12):311]. MMWR Recomm Rep. 2004;53(RR-15):1–112
Laine L, Dretler RH, Conteas CN, et al. Fluconazole compared with ketoconazole for the treatment of Candida esophagitis in AIDS. A Randomized trial Ann Intern Med. 1992;117(8):655–60. https://doi.org/10.7326/0003-4819-117-8-655.
Barbaro G, Barbarini G, Di Lorenzo G. Fluconazole vs. flucytosine in the treatment of esophageal candidiasis in AIDS patients: a double-blind, placebo-controlled study. Endoscopy. 1995;27(5):377–83. https://doi.org/10.1055/s-2007-1005717.
Barbaro G, Barbarini G, Calderon W, Grisorio B, Alcini P, Di Lorenzo G. Fluconazole versus itraconazole for candida esophagitis in acquired immunodeficiency syndrome. Candida Esophagitis. Gastroenterology. 1996;111(5):1169–77. https://doi.org/10.1053/gast.1996.v111.pm8898629.
Wilcox CM, Darouiche RO, Laine L, Moskovitz BL, Mallegol I, Wu J. A randomized, double-blind comparison of itraconazole oral solution and fluconazole tablets in the treatment of esophageal candidiasis. J Infect Dis. 1997;176(1):227–32. https://doi.org/10.1086/514028.
Villanueva A, Gotuzzo E, Arathoon EG, et al. A randomized double-blind study of caspofungin versus fluconazole for the treatment of esophageal candidiasis. Am J Med. 2002;113(4):294–9. https://doi.org/10.1016/s0002-9343(02)01191-9.
Pappas PG, Kauffman CA, Andes D, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(5):503–35. https://doi.org/10.1086/596757.
Drew WL. Cytomegalovirus infection in patients with AIDS. Clin Infect Dis. 1992;14(2):608–15.
Weber JN, Thom S, Barrison I, Unwin R, Forster S, Jeffries DJ, et al. Cytomegalovirus colitis and esophageal ulceration in the context of AIDS: clinical manifestations and preliminary report of treatment with Foscarnet (phosphonoformate). Gut. 1987;28:482–7.
• Yeh PJ, Wu RC, Chen CM, Chiu CT, Lai MW, Chen CC, Kuo CJ, Hsu JT, Su MY, Le PH. Risk factors, clinical and endoscopic features, and clinical outcomes in patients with cytomegalovirus esophagitis. J Clin Med. 2022;11(6):1583. https://doi.org/10.3390/jcm11061583.PMID:35329909;PMCID:PMC8955160. This is a recent study which highlights the risk factors of CMV esophagitis and the high mortality rate of patients with CMV esophagitis.
Freedman PG, Weiner BC, Balthazar EJ. Cytomegalovirus esophagogastritis in a patient with acquired immunodeficiency syndrome. Am J Gastroenterol. 1985;80(6):434–7.
Parente F, Cernuschi M, Valsecchi L, et al. Acute upper gastrointestinal bleeding in patients with AIDS: a relatively uncommon condition associated with reduced survival. Gut. 1991;32(9):987–90.
Wilcox CM, Diehl DL, Cello JP, Margaretten W, Jacobson MA. Cytomegalovirus esophagitis in patients with AIDS. A clinical, endoscopic, and pathologic correlation. Ann Intern Med. 1990;113(8):589–93.
Dieterich DT, Wilcox CM. Diagnosis and treatment of esophageal diseases associated with HIV infection. Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1996;91(11):2265–9.
Wang HW, Kuo CJ, Lin WR, et al. Clinical characteristics and manifestation of herpes esophagitis: one single-center experience in Taiwan. Medicine (Baltimore). 2016;95(14): e3187. https://doi.org/10.1097/MD.0000000000003187.
Bonacini M, Young T, Laine L. The causes of esophageal symptoms in human immunodeficiency virus infection. A prospective study of 110 patients. Arch Intern Med. 1991;151(8):1567–72.
Zaidi SA, Cervia JS. Diagnosis and management of infectious esophagitis associated with human immunodeficiency virus infection. J Int Assoc Physicians AIDS Care (Chic). 2002;1(2):53–62. https://doi.org/10.1177/154510970200100204.
Wilcox CM, Straub RF, Schwartz DA. Prospective evaluation of biopsy number for the diagnosis of viral esophagitis in patients with HIV infection and esophageal ulcer. Gastrointest Endosc. 1996;44(5):587–93. https://doi.org/10.1016/s0016-5107(96)70014-7.
Jazeron JF, Barbe C, Frobert E, et al. Virological diagnosis of herpes simplex virus 1 esophagitis by quantitative real-time PCR assay. J Clin Microbiol. 2012;50(3):948–52. https://doi.org/10.1128/JCM.05748-11.
Dekeyser S, El Nady M, Diaz E, Cassagnou M, Descamps D. Diagnostic d’oesophagite herpétique à HSV1 chez le sujet immunocompétent par PCR (Herpès Consensus Générique-Argène). A propos de six cas [Diagnosis of herpetic esophagitis in the immunocompetent subject by PCR (Herpès Consensus Générique-Argène). Report of six cases]. Pathol Biol (Paris). 2009;57(1):101–6. https://doi.org/10.1016/j.patbio.2008.07.005.
Rabeneck L, Popovic M, Gartner S, et al. Acute HIV infection presenting with painful swallowing and esophageal ulcers. JAMA. 1990;263(17):2318–22.
Wilcox CM, Schwartz DA. Comparison of two corticosteroid regimens for the treatment of HIV-associated idiopathic esophageal ulcer. Am J Gastroenterol. 1994;89(12):2163–7.
Kayamba V, Bateman AC, Asombang AW, et al. HIV infection and domestic smoke exposure, but not human papillomavirus, are risk factors for esophageal squamous cell carcinoma in Zambia: a case-control study. Cancer Med. 2015;4(4):588–95. https://doi.org/10.1002/cam4.434.
• Asombang AW, Chishinga N, Nkhoma A, et al. Systematic review and meta-analysis of esophageal cancer in Africa: epidemiology, risk factors, management and outcomes. World J Gastroenterol. 2019;25(31):4512–33. https://doi.org/10.3748/wjg.v25.i31.4512. This review discusses risk factors for esophageal cancer and highlights the role of HIV.
Loots E, Sartorius B, Madiba TE, Mulder CJJ, Clarke DL. Oesophageal squamous cell cancer in a South African tertiary hospital: a risk factor and presentation analysis. S Afr J Surg. 2017;55(3):42–6.
Horner MJ, Salima A, Chilima C, et al. Frequent HIV and young age among individuals with diverse cancers at a national teaching hospital in Malawi. J Glob Oncol. 2018;4:1–11. https://doi.org/10.1200/JGO.17.00174.
Thrift AP, Kramer JR, Hartman CM, et al. Risk and predictors of esophageal and stomach cancers in HIV-infected veterans: a matched cohort study. J Acquir Immune Defic Syndr. 2019;81(3):e65–72. https://doi.org/10.1097/QAI.0000000000002038.
Kahl P, Buettner R, Friedrichs N, Merkelbach-Bruse S, Wenzel J, Heukamp LC, Kaposi’s sarcoma of the gastrointestinal tract: report of two cases and review of the literature. Pathol - Res Pract. 2007;203 4;227–231, vISSN 0344–0338, https://doi.org/10.1016/j.prp.2007.01.007
Lee AJ et al. Gastrointestinal Kaposi’s sarcoma: case report and review of the literature. World J Gastrointest Pharmacol Ther. 2015;6,3:89–95. https://doi.org/10.4292/wjgpt.v6.i3.89.
Carmo J, Marques SC, Bispo M, Pinto D, Chagas C. Clinical and endoscopic features of gastrointestinal kaposi sarcoma: a single-center Portuguese experience over the last decade. GE Port J Gastroenterol. 2017;24(5):219–26. https://doi.org/10.1159/000461592.
Kalogeropoulos IV, Chalazonitis AN, Tsolaki S, Laspas F, Ptohis N, Neofytou I, Rontogianni D. A case of primary isolated non-Hodgkin’s lymphoma of the esophagus in an immunocompetent patient. World J Gastroenterol. 2009;15(15):1901–3. https://doi.org/10.3748/wjg.15.1901.
Ghai S, Pattison J, Ghai S, O’Malley ME, Khalili K, Stephens M. Primary gastrointestinal lymphoma: spectrum of imaging findings with pathologic correlation. Radiographics. 2007;27(5):1371–88. https://doi.org/10.1148/rg.275065151.
Zalar AE, Olmos MA, Piskorz EL, Magnanini FL. Esophageal motility disorders in HIV patients. Dig Dis Sci. 2003;48(5):962–7. https://doi.org/10.1023/a:1023063916026.
Barrow PH, Mahomed A, Karlsson KA. HIV and achalasia. AIDS. 2005;19(15):1709–11. https://doi.org/10.1097/01.aids.0000186820.22865.ce.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Aleem Azal Ali declares no conflict of interest.
Kimberly Sanders declares no conflict of interest.
Anna Marie McCarthy declares no conflict of interest.
Kintin Ng declares no conflict of interest.
Ahmad Alkhasawneh declares no conflict of interest.
Carmen Isache declares no conflict of interest.
Ron Schey declares no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurogastroenterology and Motility
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ali, A.A., Sanders, K., McCarthy, A.M. et al. Infective Esophagitis: a Review of Esophageal Diseases in HIV. Curr Treat Options Gastro 22, 1–14 (2024). https://doi.org/10.1007/s11938-023-00435-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-023-00435-z