Abstract
Purpose of Review
This review highlights the impact of Gnas inactivation on both bone remodeling and the development of heterotopic subcutaneous ossifications in Albright hereditary osteodystrophy (AHO). Here we discuss recent advancements in understanding the pathophysiologic mechanisms of the aberrant bone development in AHO as well as potential translational implications.
Recent Findings
Gnas inactivation can regulate the differentiation and function of not only osteoblasts but also osteoclasts and osteocytes. Investigations utilizing a mouse model of AHO generated by targeted disruption of Gnas have revealed that bone formation and resorption are differentially affected based upon the parental origin of the Gnas mutation. Data suggest that Gnas inactivation leads to heterotopic bone formation within subcutaneous tissue by changing the connective tissue microenvironment, thereby promoting osteogenic differentiation of tissue-resident mesenchymal progenitors.
Summary
Observed variations in bone formation and resorption based upon the parental origin of the Gnas mutation warrant future investigations and may have implications in the management and treatment of AHO and related conditions. Additionally, studies of heterotopic bone formation due to Gnas inactivation have identified an essential role of sonic hedgehog signaling, which could have therapeutic implications not only for AHO and related conditions but also for heterotopic bone formation in a wide variety of settings in which aberrant bone formation is a cause of significant morbidity.


Similar content being viewed by others

References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Albright F, Burnett C, Smith P. Pseudohypoparathyroidism: an example of “Seabright-Bantam syndrome”. Endocrinology. 1942;30:922–32.
Plagge A, Kelsey G, Germain-Lee EL. Physiological functions of the imprinted Gnas locus and its protein variants Galpha(s) and XLalpha(s) in human and mouse. J Endocrinol. 2008;196(2):193–214.
Levine MA. An update on the clinical and molecular characteristics of pseudohypoparathyroidism. Curr Opin Endocrinol Diabetes Obes. 2012;19(6):443–51.
Germain-Lee EL. Management of pseudohypoparathyroidism. Curr Opin Pediatr. 2019;31(4):537–49.
Linglart A, Levine MA, Juppner H. Pseudohypoparathyroidism. Endocrinol Metab Clin North Am. 2018;47(4):865–88.
Mantovani G, Bastepe M, Monk D, de Sanctis L, Thiele S, Usardi A, Ahmed SF, Bufo R, Choplin T, de Filippo G, Devernois G, Eggermann T, Elli FM, Freson K, García Ramirez A, Germain-Lee EL, Groussin L, Hamdy N, Hanna P, et al. Diagnosis and management of pseudohypoparathyroidism and related disorders: first international Consensus Statement. Nat Rev Endocrinol. 2018;14(8):476–500.
Albright FFA, Henneman P. Pseudo-pseudohypoparathyroidism. Trans Assoc Am Physicians. 1952;65:337–50.
Davies SJ, Hughes HE. Imprinting in Albright’s hereditary osteodystrophy. J Med Genet. 1993;30(2):101–3.
Levine MA, Downs RW Jr, Moses AM, Breslau NA, Marx SJ, Lasker RD, Rizzoli RE, Aurbach GD, Spiegel AM. Resistance to multiple hormones in patients with pseudohypoparathyroidism. Association with deficient activity of guanine nucleotide regulatory protein. Am J Med. 1983;74(4):545–56.
Germain-Lee EL, Ding CL, Deng Z, Crane JL, Saji M, Ringel MD, Levine MA. Paternal imprinting of Galpha(s) in the human thyroid as the basis of TSH resistance in pseudohypoparathyroidism type 1a. Biochem Biophys Res Commun. 2002;296(1):67–72.
Namnoum AB, Merriam GR, Moses AM, Levine MA. Reproductive dysfunction in women with Albright’s hereditary osteodystrophy. J Clin Endocrinol Metab. 1998;83(3):824–9.
Mantovani G, Maghnie M, Weber G, De Menis E, Brunelli V, Cappa M, et al. Growth hormone-releasing hormone resistance in pseudohypoparathyroidism type ia: new evidence for imprinting of the Gs alpha gene. J Clin Endocrinol Metab. 2003;88(9):4070–4.
Germain-Lee EL, Groman. J, Crane JL, Jan de Beur SM, Levine MA. Growth hormone deficiency in pseudohypoparathyroidism type 1a: another manifestation of multihormone resistance. J Clin Endocrinol Metab. 2003;88(9):4059–69.
Germain-Lee EL. Short stature, obesity, and growth hormone deficiency in pseudohypoparathyroidism type 1a. Pediatr Endocrinol Rev. 2006;3(Suppl 2):318–27.
Long DN, McGuire S, Levine MA, Weinstein LS, Germain-Lee EL. Body mass index differences in pseudohypoparathyroidism type 1a versus pseudopseudohypoparathyroidism may implicate paternal imprinting of Galpha(s) in the development of human obesity. J Clin Endocrinol Metab. 2007;92(3):1073–9.
Hayward BE, Kamiya M, Strain L, Moran V, Campbell R, Hayashizaki Y, Bonthron DT. The human GNAS1 gene is imprinted and encodes distinct paternally and biallelically expressed G proteins. Proc Natl Acad Sci U S A. 1998;95(17):10038–43.
Liu J, Erlichman B, Weinstein LS. The stimulatory G protein alpha-subunit Gs alpha is imprinted in human thyroid glands: implications for thyroid function in pseudohypoparathyroidism types 1A and 1B. J Clin Endocrinol Metab. 2003;88(9):4336–41.
Germain-Lee EL, Schwindinger W, Crane JL, Zewdu R, Zweifel LS, Wand G, Huso DL, Saji M, Ringel MD, Levine MA. A mouse model of Albright hereditary osteodystrophy generated by targeted disruption of exon 1 of the Gnas gene. Endocrinology. 2005;146(11):4697–709.
Mantovani G, Ballare E, Giammona E, Beck-Peccoz P, Spada A. The gsalpha gene: predominant maternal origin of transcription in human thyroid gland and gonads. J Clin Endocrinol Metab. 2002;87(10):4736–40.
Weinstein LS, Yu S, Ecelbarger CA. Variable imprinting of the heterotrimeric G protein G(s) alpha-subunit within different segments of the nephron. Am J Physiol Renal Physiol. 2000;278(4):F507–14.
Yu S, Yu D, Lee E, Eckhaus M, Lee R, Corria Z, Accili D, Westphal H, Weinstein LS. Variable and tissue-specific hormone resistance in heterotrimeric Gs protein alpha-subunit (Gsalpha) knockout mice is due to tissue-specific imprinting of the gsalpha gene. Proc Natl Acad Sci U S A. 1998;95(15):8715–20.
Shore EM, Ahn J. Jan de Beur S, Li M, Xu M, Gardner RJ, et al. Paternally inherited inactivating mutations of the GNAS1 gene in progressive osseous heteroplasia. N Engl J Med. 2002;346(2):99–106.
Sakamoto A, Chen M, Nakamura T, Xie T, Karsenty G, Weinstein LS. Deficiency of the G-protein alpha-subunit G(s)alpha in osteoblasts leads to differential effects on trabecular and cortical bone. J Biol Chem. 2005;280(22):21369–75.
Xu R, Khan SK, Zhou T, Gao B, Zhou Y, Zhou X, Yang Y. Galphas signaling controls intramembranous ossification during cranial bone development by regulating both Hedgehog and Wnt/beta-catenin signaling. Bone Res. 2018;6:33.
Cong Q, Xu R, Yang Y. Galphas signaling in skeletal development, homeostasis and diseases. Curr Top Dev Biol. 2019;133:281–307.
Wu JY, Aarnisalo P, Bastepe M, Sinha P, Fulzele K, Selig MK, Chen M, Poulton IJ, Purton LE, Sims NA, Weinstein LS, Kronenberg HM. Gsalpha enhances commitment of mesenchymal progenitors to the osteoblast lineage but restrains osteoblast differentiation in mice. J Clin Invest. 2011;121(9):3492–504.
Fulzele K, Krause DS, Panaroni C, Saini V, Barry KJ, Liu X, Lotinun S, Baron R, Bonewald L, Feng JQ, Chen M, Weinstein LS, Wu JY, Kronenberg HM, Scadden DT, Divieti Pajevic P. Myelopoiesis is regulated by osteocytes through Gsalpha-dependent signaling. Blood. 2013;121(6):930–9.
Fulzele K, Dedic C, Lai F, Bouxsein M, Lotinun S, Baron R, et al. Loss of Gsalpha in osteocytes leads to osteopenia due to sclerostin induced suppression of osteoblast activity. Bone. 2018;117:138–48 Fulzele et al. demonstrate a role of Gαs-signaling influencing osteocyte density and osteocyte-derived sclerostin production and reveal that pharmacological treatment with an anti-sclerostin antibody can partially rescue osteopenia within Gαs-deficient mice.
Huso DL, Edie S, Levine MA, Schwindinger W, Wang Y, Juppner H, Germain-Lee EL. Heterotopic ossifications in a mouse model of albright hereditary osteodystrophy. PLoS One. 2011;6(6):e21755.
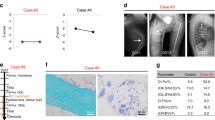
Salemi P, Skalamera Olson JM, Dickson LE, Germain-Lee EL. Ossifications in Albright hereditary osteodystrophy: role of genotype, inheritance, sex, age, hormonal status, and BMI. J Clin Endocrinol Metab. 2018;103(1):158–68 Salemi et al. provide essential clinical data regarding the prevalence of subcutaneous ossification formation in AHO. This study examined a large group of patients with AHO over a span of 16 years and found that approximately 70% of both PHP1A and PPHP patients developed SCOs, which were more extensive in those with frameshift and nonsense mutations and which were more pronounced in males compared to females. They also show that the prevalence of ossifications is independent of age, hormonal resistance, body mass index, and presence of other AHO physical features such as brachydactyly or brachymetacarpia.
Regard JB, Malhotra D, Gvozdenovic-Jeremic J, Josey M, Chen M, Weinstein LS, Lu J, Shore EM, Kaplan FS, Yang Y. Activation of Hedgehog signaling by loss of GNAS causes heterotopic ossification. Nat Med. 2013;19(11):1505–12.
Pignolo RJ, Xu M, Russell E, Richardson A, Kaplan J, Billings PC, Kaplan FS, Shore EM. Heterozygous inactivation of Gnas in adipose-derived mesenchymal progenitor cells enhances osteoblast differentiation and promotes heterotopic ossification. J Bone Miner Res. 2011;26(11):2647–55.
Adegbite NS, Xu M, Kaplan FS, Shore EM, Pignolo RJ. Diagnostic and mutational spectrum of progressive osseous heteroplasia (POH) and other forms of GNAS-based heterotopic ossification. Am J Med Genet A. 2008;146A(14):1788–96.
Ramaswamy G, Kim H, Zhang D, Lounev V, Wu JY, Choi Y, et al. Gsalpha controls cortical bone quality by regulating osteoclast differentiation via cAMP/PKA and beta-catenin pathways. Sci Rep. 2017;7:45140 Ramaswamy et al. identify distinctions in overall cortical bone quality as well as osteocyte and osteoclast number in vivo among Gnas+/- mice based on the inheritance pattern of their Gnas mutation. Specifically, mice with paternally-inherited (Gnas+/-p) mutations display a reduction in cortical bone quality with an increase in both the number of osteocytes and endosteal osteoclasts when compared to WT; however, mice with maternally-inherited (Gnas+/-m) mutations display no significant changes in cortical bone quality or endosteal osteoclast number compared to WT and display a reduction in the number of osteocytes compared to WT.
Weivoda MM, Ruan M, Hachfeld CM, Pederson L, Howe A, Davey RA, Zajac JD, Kobayashi Y, Williams BO, Westendorf JJ, Khosla S, Oursler MJ. Wnt signaling inhibits osteoclast differentiation by activating canonical and noncanonical cAMP/PKA pathways. J Bone Miner Res. 2016;31(1):65–75.
Yoon SH, Ryu J, Lee Y, Lee ZH, Kim HH. Adenylate cyclase and calmodulin-dependent kinase have opposite effects on osteoclastogenesis by regulating the PKA-NFATc1 pathway. J Bone Miner Res. 2011;26(6):1217–29.
Ramaswamy G, Fong J, Brewer N, Kim H, Zhang D, Choi Y, Kaplan FS, Shore EM. Ablation of Gsalpha signaling in osteoclast progenitor cells adversely affects skeletal bone maintenance. Bone. 2018;109:86–90.
Fulzele K, Lai F, Dedic C, Saini V, Uda Y, Shi C, Tuck P, Aronson JL, Liu X, Spatz JM, Wein MN, Divieti Pajevic P. Osteocyte-secreted Wnt signaling inhibitor sclerostin contributes to beige adipogenesis in peripheral fat depots. J Bone Miner Res. 2017;32(2):373–84.
Azab E, Chandler KB, Uda Y, Sun N, Hussein A, Shuwaikan R, Lu V, Costello CE, McComb ME, Divieti Pajevic P. Osteocytes control myeloid cell proliferation and differentiation through Gsalpha-dependent and -independent mechanisms. FASEB J. 2020;34(8):10191–211.
Divieti Pajevic P, Krause DS. Osteocyte regulation of bone and blood. Bone. 2019;119:13–8.
Bonewald LF. The amazing osteocyte. J Bone Miner Res. 2011;26(2):229–38.
Dallas SL, Prideaux M, Bonewald LF. The osteocyte: an endocrine cell ... and more. Endocr Rev. 2013;34(5):658-690, The Osteocyte: An Endocrine Cell … and More.
Spatz JM, Wein MN, Gooi JH, Qu Y, Garr JL, Liu S, Barry KJ, Uda Y, Lai F, Dedic C, Balcells-Camps M, Kronenberg HM, Babij P, Pajevic PD. The Wnt inhibitor sclerostin is up-regulated by mechanical unloading in osteocytes in vitro. J Biol Chem. 2015;290(27):16744–58.
Wein MN, Liang Y, Goransson O, Sundberg TB, Wang J, Williams EA, O’Meara MJ, Govea N, Beqo B, Nishimori S, Nagano K, Brooks DJ, Martins JS, Corbin B, Anselmo A, Sadreyev R, Wu JY, Sakamoto K, Foretz M, et al. SIKs control osteocyte responses to parathyroid hormone. Nat Commun. 2016;7:13176.
Trinchieri G. Interleukin-12 and the regulation of innate resistance and adaptive immunity. Nat Rev Immunol. 2003;3(2):133–46.
Sugiyama T, Kohara H, Noda M, Nagasawa T. Maintenance of the hematopoietic stem cell pool by CXCL12-CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity. 2006;25(6):977–88.
Long DN, Levine MA, Germain-Lee EL. Bone mineral density in pseudohypoparathyroidism type 1a. J Clin Endocrinol Metab. 2010;95(9):4465–75.
McMullan P, Maye P, Yang Q, Rowe DW, Germain-Lee EL. Parental origin of Gsα inactivation differentially affects bone remodeling in a mouse model of Albright hereditary osteodystrophy. J Bone Miner Res Plus. 2021:e10570. https://doi.org/10.1002/jbm4.10570McMullan et al. identify distinctions in overall cortical bone architecture, bone formation, and bone resorption in vivo among Gnas+/- mice based on the inheritance pattern of their Gnas mutation. In particular, mice with paternally-inherited (Gnas+/-p) mutations display a reduction in cortical bone parameters that correlate with a reduction in osteoblast number and mineral apposition as well as an increase in osteoclast number and bone resorption when compared to WT. Alternatively, mice with maternally-inherited (Gnas+/-m) mutations display normal to increased cortical bone parameters when compared to WT that can be attributed to a significant increase in osteoblast activity without significant concomitant variations in osteoclast number or in the amount of bone resorption.
Pignolo RJ, Ramaswamy G, Fong JT, Shore EM, Kaplan FS. Progressive osseous heteroplasia: diagnosis, treatment, and prognosis. Appl Clin Genet. 2015;8:37–48.
Izraeli S, Metzker A, Horev G, Karmi D, Merlob P, Farfel Z. Albright hereditary osteodystrophy with hypothyroidism, normocalcemia, and normal Gs protein activity: a family presenting with congenital osteoma cutis. Am J Med Genet. 1992;43(4):764–7.
Prendiville JS, Lucky AW, Mallory SB, Mughal Z, Mimouni F, Langman CB. Osteoma cutis as a presenting sign of pseudohypoparathyroidism. Pediatr Dermatol. 1992;9(1):11–8.
Kaplan FS, Craver R, MacEwen GD, Gannon FH, Finkel G, Hahn G, et al. Progressive osseous heteroplasia: a distinct developmental disorder of heterotopic ossification. Two new case reports and follow-up of three previously reported cases. J Bone Joint Surg Am. 1994;76(3):425–36.
Kaplan FS, Shore EM. Progressive osseous heteroplasia. J Bone Miner Res. 2000;15(11):2084–94.
Eddy MC, Jan De Beur SM, Yandow SM, McAlister WH, Shore EM, Kaplan FS, et al. Deficiency of the alpha-subunit of the stimulatory G protein and severe extraskeletal ossification. J Bone Miner Res. 2000;15(11):2074–83.
Lin MH, Numbenjapon N, Germain-Lee EL, Pitukcheewanont P. Progressive osseous heteroplasia, as an isolated entity or overlapping with Albright hereditary osteodystrophy. J Pediatr Endocrinol Metab. 2015;28(7-8):911–8.
Levine MA, Eil C, Downs RW Jr, Spiegel AM. Deficient guanine nucleotide regulatory unit activity in cultured fibroblast membranes from patients with pseudohypoparathyroidism type I. a cause of impaired synthesis of 3',5'-cyclic AMP by intact and broken cells. J Clin Invest. 1983;72(1):316–24.
Meyers C, Lisiecki J, Miller S, Levin A, Fayad L, Ding C, Sono T, McCarthy E, Levi B, James AW. Heterotopic ossification: a comprehensive review. JBMR Plus. 2019;3(4):e10172.
Kaplan FS, Glaser DL, Hebela N, Shore EM. Heterotopic ossification. J Am Acad Orthop Surg. 2004;12(2):116–25.
Jahoda CA, Whitehouse J, Reynolds AJ, Hole N. Hair follicle dermal cells differentiate into adipogenic and osteogenic lineages. Exp Dermatol. 2003;12(6):849–59.
Mistriotis P, Andreadis ST. Hair follicle: a novel source of multipotent stem cells for tissue engineering and regenerative medicine. Tissue Eng Part B Rev. 2013;19(4):265–78.
Hsu YC, Li L, Fuchs E. Emerging interactions between skin stem cells and their niches. Nat Med. 2014;20(8):847–56.
Cong Q, Liu Y, Zhou T, Zhou Y, Xu R, Cheng C, et al. A self-amplifying loop of YAP and SHH drives formation and expansion of heterotopic ossification. Sci Transl Med. 2021;13(599) Cong et al. demonstrate a conserved role of a positive hedgehog and hippo signaling loop across mouse models that form heterotopic ossifications as a result of genetic etiologies (POH and FOP mouse models) and trauma-induced etiologies (such as Achilles tendon puncture injury) and that pharmacological inhibition of either hedgehog or hippo signaling in these models is sufficient in abrogating heterotopic bone formation.
Brewer N, Fong JT, Zhang D, Ramaswamy G, Shore EM. Gnas inactivation alters subcutaneous tissues in progression to heterotopic ossification. Front Genet. 2021;12:633206 Brewer et al. suggest that heterotopic ossification formation as a result of Gnas inactivation is not necessarily a cell-autonomous process but rather involves a delicate balance of cellular expansion with changes in the tissue microenvironment.
Kan C, Chen L, Hu Y, Ding N, Lu H, Li Y, Kessler JA, Kan L. Conserved signaling pathways underlying heterotopic ossification. Bone. 2018;109:43–8.
Haupt J, Stanley A, McLeod CM, Cosgrove BD, Culbert AL, Wang L, et al. ACVR1(R206H) FOP mutation alters mechanosensing and tissue stiffness during heterotopic ossification. Mol Biol Cell. 2019;30(1):17–29.
Stanley A, Heo SJ, Mauck RL, Mourkioti F, Shore EM. Elevated BMP and mechanical signaling through YAP1/RhoA poises FOP mesenchymal progenitors for osteogenesis. J Bone Miner Res. 2019;34(10):1894–909.
Huber AK, Patel N, Pagani CA, Marini S, Padmanabhan KR, Matera DL, Said M, Hwang C, Hsu GCY, Poli AA, Strong AL, Visser ND, Greenstein JA, Nelson R, Li S, Longaker MT, Tang Y, Weiss SJ, Baker BM, et al. Immobilization after injury alters extracellular matrix and stem cell fate. J Clin Invest. 2020;130(10):5444–60.
Iglesias-Bartolome R, Torres D, Marone R, Feng X, Martin D, Simaan M, Chen M, Weinstein LS, Taylor SS, Molinolo AA, Gutkind JS. Inactivation of a Galpha(s)-PKA tumour suppressor pathway in skin stem cells initiates basal-cell carcinogenesis. Nat Cell Biol. 2015;17(6):793–803.
BioRender [cited 2021. Available from: https://biorender.com/.
Adapted from “Tissue-Specific Effects of Connective Tissue and Mucosal Mast Cells: Subcutaneous Entry”, by BioRender.com 2021 [Available from: https://app.biorender.com/biorender-templates
Joseph AW, Shoemaker AH, Germain-Lee EL. Increased prevalence of carpal tunnel syndrome in Albright hereditary osteodystrophy. J Clin Endocrinol Metab. 2011 Jul;96(7):2065–73.
Funding
This work was supported by National Institutes of Health Grant NICHD R21 HD078864 to E.L.G-L and Connecticut Children’s Albright Fund to E.L.G.-L. P.M. was supported by training grant NIDCR T90DE021989-09 and the Connecticut Children’s Albright Fund.
Author information
Authors and Affiliations
Contributions
Both authors (P.M. and E.L.G.-L.) contributed equally to the preparation of this manuscript with respect to literature search and data analysis, drafting of the original manuscript, and critical revision of the manuscript. The authors have no disclosures.
Corresponding author
Ethics declarations
Conflicts of Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Rare Bone Disease
Rights and permissions
About this article
Cite this article
McMullan, P., Germain-Lee, E.L. Aberrant Bone Regulation in Albright Hereditary Osteodystrophy dueto Gnas Inactivation: Mechanisms and Translational Implications. Curr Osteoporos Rep 20, 78–89 (2022). https://doi.org/10.1007/s11914-022-00719-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-022-00719-w