Abstract
Purpose of Review
Cigarette smoking is the primary cause of cancer and is the leading preventable cause of morbidity and mortality. Cognitive behavioral therapy (CBT) is one of the most well-established and efficacious interventions for smoking cessation. The study of mindfulness-based interventions (MBIs) has increased exponentially in recent years, showing efficacy for smoking cessation as well. This review highlights research from the past 5 years examining CBT and MBIs for smoking cessation.
Recent Findings
Both CBT and MBIs are efficacious for special populations (e.g., low SES; pregnant smokers) and have shown initial efficacy when delivered via mhealth/ehealth. CBT has shown efficacy when combined with another behavioral treatment (e.g., ACT).
Summary
Continued research is needed on CBT and MBIs that have high potential for scalability. Understanding whether they are beneficial for certain populations (e.g., cancer survivors), along with determining for whom CBT vs MBIs are most effective, is also needed.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Cancer Society. Cancer facts and figures 2014. Atlanta: American Cancer Society; 2014.
U.S. Department of Health and Human Services. The health consequences of smoking—50 years of progress: a report of the surgeon general. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
Centers for Disease Control and Prevention. Current cigarette smoking among adults—United States, 2017. Morb Mortal Wkly Rep. 2018; 67(44):1225–1232.
Nathan PE, Gorman JM. A guide to treatments that work: Oxford University Press; 2015.
Marlatt GA, Donovan DM. Relapse prevention: maintenance strategies in the treatment of addictive behaviors: Guilford Press; 2005.
Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz N, Curry S, et al. Clinical practice guideline. Rockville: US Department of Health and Human Services. Public Health Service; 2008. p. 1196–9.
Šagud M, Mihaljević-Peleš A, Mück-Šeler D, Pivac N, Vuksan-Ćusa B, Brataljenović T, et al. Smoking and schizophrenia. Psychiatr Danub. 2009;21(3):371–5.
Evins AE, Cather C, Pratt SA, Pachas GN, Hoeppner SS, Goff DC, et al. Maintenance treatment with varenicline for smoking cessation in patients with schizophrenia and bipolar disorder: a randomized clinical trial. JAMA. 2014;311(2):145–54.
Cather C, Pachas GN, Cieslak KM, Evins AE. Achieving smoking cessation in individuals with schizophrenia: special considerations. CNS drugs. 2017;31(6):471–81.
Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: what you need to know. J Subst Abus Treat. 2009;36(2):205–19.
Cookson C, Strang J, Ratschen E, Sutherland G, Finch E, McNeill A. Smoking and its treatment in addiction services: clients’ and staff behaviour and attitudes. BMC Health Serv Res. 2014;14(1):304.
McCarthy WJ, Collins C, Hser Y-I. Does cigarette smoking affect drug abuse treatment? J Drug Issues. 2002;32(1):61–79.
Thurgood SL, McNeill A, Clark-Carter D, Brose LS. A systematic review of smoking cessation interventions for adults in substance abuse treatment or recovery. Nicotine Tob Res. 2016;18(5):993–1001.
Mdodo R, Frazier EL, Dube SR, Mattson CL, Sutton MY, Brooks JT, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys. Ann Intern Med. 2015;162(5):335–44.
Crothers K, Goulet JL, Rodriguez-Barradas MC, Gibert CL, Oursler KAK, Goetz MB, et al. Impact of cigarette smoking on mortality in HIV-positive and HIV-negative veterans. AIDS Educ Prev. 2009;21(3_supplement):40–53.
Feldman DN, Feldman JG, Greenblatt R, Anastos K, Pearce L, Cohen M, et al. CYP1A1 genotype modifies the impact of smoking on effectiveness of HAART among women. AIDS Educ Prev. 2009;21(3_supplement):81–93.
Lifson AR, Neuhaus J, Arribas JR, van den Berg-Wolf M, Labriola AM, Read TR, et al. Smoking-related health risks among persons with HIV in the strategies for management of antiretroviral therapy clinical trial. Am J Public Health. 2010;100(10):1896–903.
•• O'Cleirigh C, Zvolensky MJ, Smits JA, Labbe AK, Coleman JN, Wilner JG, et al. Integrated treatment for smoking cessation, anxiety, and depressed mood in people living with HIV: a randomized controlled trial. JAIDS J Acquir Immune Def Synd. 2018;79(2):261–8 Participants living with HIV (N=72) were randomized to either QUIT (1 psychoeducational session + 8 CBT sessions that targeted smoking cessation, anxiety, and depression) or ETAU (1 psychoeducation session + 4 brief, weekly check-in sessions). Those in the QUIT intervention had significantly higher abstinence rates at end of treatment and 6 months post-quit than the ETAU group.
Centers for Disease Control and Prevention. Quitting smoking among adults - United States, 2001–2010. Morbidity Mortal Weekly Rep. 2011;60(44):1513–9.
Hooper MW, Lee DJ, Simmons VN, Brandon KO, Antoni MH, Unrod M, et al. Reducing racial/ethnic tobacco cessation disparities via cognitive behavioral therapy: design of a dualsite randomized controlled trial. Contemp Clin Trials. 2018;68:127–32.
Webb Hooper M, Kolar SK. Distress, race/ethnicity and smoking cessation in treatment-seekers: implications for disparity elimination. Addiction. 2015;110(9):1495–504.
Carroll KM. Lost in translation? Moving contingency management and cognitive behavioral therapy into clinical practice. Ann N Y Acad Sci. 2014;1327(1):94.
Japuntich SJ, Lee LO, Pineles SL, Gregor K, Joos CM, Patton SC, et al. Contingency management and cognitive behavioral therapy for trauma-exposed smokers with and without posttraumatic stress disorder. Addict Behav. 2019;90:136–42.
Secades-Villa R, García-Rodríguez O, López-Núñez C, Alonso-Pérez F, Fernández-Hermida JR. Contingency management for smoking cessation among treatment-seeking patients in a community setting. Drug Alcohol Depend. 2014;140:63–8.
Centers for Disease Control and Prevention. Current cigarette smoking among adults - United States, 2005–2015. Morbid Mortal Weekly Rep. 2016; 65(44):1205–1211.
Fang WL, Goldstein AO, Butzen AY, Hartsock SA, Hartmann KE, Helton M, et al. Smoking cessation in pregnancy: a review of postpartum relapse prevention strategies. J Am Board Fam Pract. 2004;17(4):264–75.
Rockhill KM, Tong VT, Farr SL, Robbins CL, D'Angelo DV, England LJ. Postpartum smoking relapse after quitting during pregnancy: pregnancy risk assessment monitoring system, 2000–2011. J Women's Health. 2016;25(5):480–8.
• Bradizza CM, Stasiewicz PR, Zhuo Y, Ruszczyk M, Maisto SA, Lucke JF, et al. Smoking cessation for pregnant smokers: development and pilot test of an emotion regulation treatment supplement to standard smoking cessation for negative affect smokers. Nicotine & Tobacco Research. 2017;19(5):578–84 Pregnant smokers (N=70) were randomized to one of two groups: 1) emotion regulation treatment (ERT) + CBT, or 2) a control group of health and lifestyle + CBT. The ERT + CBT condition had higher abstinence rates and smoked fewer cigarettes per day compared to the control group at follow-ups.
Ghorai K, Akter S, Khatun F, Ray P. mHealth for smoking cessation programs: a systematic review. J Personal Med. 2014;4(3):412–23.
Haskins BL, Lesperance D, Gibbons P, Boudreaux ED. A systematic review of smartphone applications for smoking cessation. Transl Behav Med. 2017;7(2):292–9.
Scott-Sheldon LA, Lantini RC, Jennings EG, Thind H, Rosen RK, Salmoirago-Blotcher E, et al. Text messaging-based interventions for smoking cessation: a systematic review and meta-analysis. JMIR mHealth uHealth. 2016;4(2):e49.
Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2016;4.
Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One. 2010;5(10):e13196.
Grist R, Cavanagh K. Computerised cognitive behavioural therapy for common mental health disorders, what works, for whom under what circumstances? A systematic review and meta-analysis. J Contemp Psychother. 2013;43(4):243–51.
Watts S, Mackenzie A, Thomas C, Griskaitis A, Mewton L, Williams A, et al. CBT for depression: a pilot RCT comparing mobile phone vs. computer. BMC Psychiatry. 2013;13(1):49.
Tudor-Sfetea C, Rabee R, Najim M, Amin N, Chadha M, Jain M, et al. Evaluation of two mobile health apps in the context of smoking cessation: qualitative study of cognitive behavioral therapy (CBT) versus non-CBT-based digital solutions. JMIR mHealth uHealth. 2018;6(4):e98.
Bricker JB, Mull KE, Kientz JA, Vilardaga R, Mercer LD, Akioka KJ, et al. Randomized, controlled pilot trial of a smartphone app for smoking cessation using acceptance and commitment therapy. Drug Alcohol Depend. 2014;143:87–94.
Heffner JL, Vilardaga R, Mercer LD, Kientz JA, Bricker JB. Feature-level analysis of a novel smartphone application for smoking cessation. Am J Drug Alcohol Abuse. 2015;41(1):68–73.
Zeng EY, Vilardaga R, Heffner JL, Mull KE, Bricker JB. Predictors of utilization of a novel smoking cessation smartphone app. Telemed e-Health. 2015;21(12):998–1004.
de Souza ICW, de Barros VV, Gomide HP, Miranda TCM, de Paula MV, Kozasa EH, et al. Mindfulness-based interventions for the treatment of smoking: a systematic literature review. J Altern Complement Med. 2015;21(3):129–40.
Maglione MA, Maher AR, Ewing B, Colaiaco B, Newberry S, Kandrack R, et al. Efficacy of mindfulness meditation for smoking cessation: a systematic review and meta-analysis. Addict Behav. 2017;69:27–34.
Oikonomou MT, Arvanitis M, Sokolove RL. Mindfulness training for smoking cessation: a meta-analysis of randomized-controlled trials. J Health Psychol. 2017;22(14):1841–1850.
Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don't. Ann N Y Acad Sci. 1999;896(1):3–15.
Businelle MS, Kendzor DE, Reitzel LR, Costello TJ, Cofta-Woerpel L, Li Y, et al. Mechanisms linking socioeconomic status to smoking cessation: a structural equation modeling approach. Health Psychol. 2010;29(3):262–73.
Gallo LC, de los Monteros KE, Shivpuri S. Socioeconomic status and health: what is the role of reserve capacity? Curr Dir Psychol Sci. 2009;18(5):269–74.
Barbeau EM, Krieger N, Soobader MJ. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health. 2004;94(2):269–78.
Centers for Disease Control and Prevention. Current cigarette smoking among adults - United States, 2005–2012. Morb Mortal Wkly Rep. 2015;63(02):29–34.
Chiang K, Borrelli B. Income predictors of smoking cessation among Hispanics. J Health Psychol. 2014;19(7):869–76.
Kendzor DE, Businelle MS, Costello TJ, Castro Y, Reitzel LR, Cofta-Woerpel LM, et al. Financial strain and smoking cessation among racially/ethnically diverse smokers. Am J Public Health. 2010;100(4):702–6.
Vinci C, Guo L, Spears CA, Li L, Etcheverry PE, Lam CY, et al. Socioeconomic indicators as predictors of smoking cessation among Spanish-speaking Mexican Americans. Ethn Health. 2019; 24(7):841–853.
Davis JM, Goldberg SB, Anderson MC, Manley AR, Smith SS, Baker TB. Randomized trial on mindfulness training for smokers targeted to a disadvantaged population. Subst Use Misuse. 2014;49(5):571–85.
Davis JM, Manley AR, Goldberg SB, Stankevitz KA, Smith SS. Mindfulness training for smokers via web-based video instruction with phone support: a prospective observational study. BMC Complement Altern Med. 2015;15(1):1.
Spears CA, Abroms LC, Glass CR, Hedeker D, Eriksen MP, Cottrell-Daniels C, et al. Mindfulness-based smoking cessation enhanced with mobile technology (iQuit mindfully): pilot randomized controlled trial. JMIR mHealth uHealth. 2019;7(6):e13059.
•• Vidrine JI, Spears CA, Heppner WL, Reitzel LR, Marcus MT, Cinciripini PM, et al. Efficacy of mindfulness-based addiction treatment (MBAT) for smoking cessation and lapse recovery: a randomized clinical trial. J Consult Clin Psychol. 2016;84:824–38 The largest RCT to date (N=412) examining MBI vs CBT vs TAU for smoking cessation among low SES individuals. Results indicated no significant group differences, but that those in the MBI group were more successful at recovering from a lapse.
Brown KW, Weinstein N, Creswell JD. Trait mindfulness modulates neuroendocrine and affective responses to social evaluative threat. Psychoneuroendocrinology. 2012;37(12):2037–41.
Creswell JD, Lindsay EK. How does mindfulness training affect health? A mindfulness stress buffering account. Curr Dir Psychol Sci. 2014;23(6):401–7.
Singh NN, Lancioni GE, Myers RE, Karazsia BT, Winton AS, Singh J. A randomized controlled trial of a mindfulness-based smoking cessation program for individuals with mild intellectual disability. Int J Ment Heal Addict. 2014;12(2):153–68.
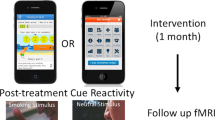
•• Garrison KA, Pal P, O’Malley SS, Pittman BP, Gueorguieva R, Rojiani R, et al. Craving to quit: a randomized controlled trial of smartphone app–based mindfulness training for smoking cessation. Nicotine Tob Res. 2020; 22(3):324–331; RCT that found both the experience sampling and mindfulness + experience sampling groups had reductions in cigarettes per day and craving at 6 months follow-up. For those in the mindfulness group, the relationship between craving and cigarettes per day lessened over time, which could aid in long-term cessation.
Garrison KA, Pal P, Rojiani R, Dallery J, O’Malley SS, Brewer JA. A randomized controlled trial of smartphone-based mindfulness training for smoking cessation: a study protocol. BMC Psychiatry. 2015;15(1):83.
Minami H, Brinkman HR, Nahvi S, Arnsten JH, Rivera-Mindt M, Wetter DW, et al. Rationale, design and pilot feasibility results of a smartphone-assisted, mindfulness-based intervention for smokers with mood disorders: project mSMART MIND. Contemp Clin Trials. 2018;66:36–44.
Vidrine DJ, Frank-Pearce SG, Vidrine JI, Tahay PD, Marani SK, Chen S, et al. Efficacy of mobile phone–delivered smoking cessation interventions for socioeconomically disadvantaged individuals: a randomized clinical trial. JAMA Intern Med. 2019;179(2):167–74.
Abroms LC, Johnson PR, Heminger CL, Van Alstyne JM, Leavitt LE, Schindler-Ruwisch JM, et al. Quit4baby: results from a pilot test of a mobile smoking cessation program for pregnant women. JMIR mHealth uHealth. 2015;3(1):e10.
Abroms LC, Johnson PR, Leavitt LE, Cleary SD, Bushar J, Brandon TH, et al. A randomized trial of text messaging for smoking cessation in pregnant women. Am J Prev Med. 2017;53(6):781–90.
Nahum-Shani, I, Smith, SN, Sping, BJ, Collin LM, Witkiewitz, K, Tewari, A, & Murpy, SA. Just-in-Time adpative interventions (JITAIs) in mobile health: Key components and design principles for ongoing health behavior support. Ann Behav Med. 2018; 52(6):446–462.
Spruijt-Metz D, Nilsen W. Dynamic models of behavior for just-in-time adaptive interventions. IEEE Perv Comput. 2014;3:13–7.
Vinci C, Haslam A, Lam CY, Kumar S, Wetter DW. The use of ambulatory assessment in smoking cessation. Addict Behav. 2018;83:18–24.
Businelle MS, Ma P, Kendzor DE, Frank SG, Vidrine DJ, Wetter DW. An ecological momentary intervention for smoking cessation: evaluation of feasibility and effectiveness. J Med Internet Res. 2016;18(12): e321.
Cerrada CJ, Dzubur E, Blackman KC, Mays V, Shoptaw S, Huh J. Development of a just-in-time adaptive intervention for smoking cessation among Korean American emerging adults. Int J Behav Med. 2017;24(5):665–72.
Hébert ET, Stevens EM, Frank SG, Kendzor DE, Wetter DW, Zvolensky MJ, et al. An ecological momentary intervention for smoking cessation: the associations of just-in-time, tailored messages with lapse risk factors. Addict Behav. 2018;78:30–5.
Naughton F. Delivering “Just-In-Time” smoking cessation support via mobile phones: current knowledge and future directions. Nicotine Tob Res. 2017;19(3):379–83.
Naughton F, Hopewell S, Lathia N, Schalbroeck R, Brown C, Mascolo C, et al. A context-sensing mobile phone app (Q sense) for smoking cessation: a mixed-methods study. JMIR mHealth and uHealth. 2016;4(3):e106.
Brandon TH, Simmons VN, Sutton SK, Unrod M, Harrell PT, Meade CD, et al. Extended self-help for smoking cessation: a randomized controlled trial. Am J Prev Med. 2016;51(1):54–62.
Sheeran P, Jones K, Avishai A, Symes YR, Abraham C, Miles E, et al. What works in smoking cessation interventions for cancer survivors? A meta-analysis. Health Psychol. 2019;38(10):855–65.
Funding
This manuscript was supported by funding from the National Center for Complementary and Integrative Health (R34AT009689).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Christine Vinci declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Integrative Care
Rights and permissions
About this article
Cite this article
Vinci, C. Cognitive Behavioral and Mindfulness-Based Interventions for Smoking Cessation: a Review of the Recent Literature. Curr Oncol Rep 22, 58 (2020). https://doi.org/10.1007/s11912-020-00915-w
Published:
DOI: https://doi.org/10.1007/s11912-020-00915-w