Abstract
Purpose of Review
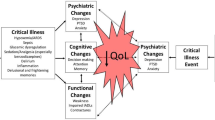
Purposes were to identify evidence for post-intensive care syndrome (PICS) and post-intensive care syndrome-family (PICS-F), defined as the psychological impact on families from exposure to critical care, in the neurologically injured population and to characterize existing models for neurorecovery clinics and the evidence to support their use.
Recent Findings
There has been an explosion of post-ICU clinics among the general critical care population, with their use largely justified based on the management of PICS and PICS-F, terminology which excludes brain injured patients. In contrast, neurocritical care recovery clinics are not common and not well-described. There is however evidence in the neuro-ICU population supporting the provision of “dyadic” care, whereby the patient and caregiver are treated as one unit.
Summary
Brain injured populations likely experience many of the same PICS phenomena as medically ill patients but are not represented in this body of literature. These patients deserve the same level of follow-up as other patients who have experienced critical illness. We propose a neuro-ICU transitional care clinic that addresses PICS-like symptoms and is modeled after transitional care provided to other brain injured populations. Future investigations should be targeted toward understanding the sequalae of a neuro-ICU admission, mechanisms for providing dyadic care, and the impact of neurorecovery clinics on long-term outcomes.


Similar content being viewed by others
Data Availability
This is not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2). https://doi.org/10.1097/CCM.0b013e318232da75.
Cameron J, Chu L, Matte A, Tomlinson G, Chan L, Thomas C, Friedrich JO, Mehta S, Lamontagne F, Levasseur M, Ferguson ND, Adhikari NKJ, Rudkowski JC, Meggison H, Skrobik Y, Flannery J, Bayley M, Batt J, dos Santos C, Abbey SE, Tan A, Lo V, Mathur S, Parotto M, Morris D, Flockhart L, Fan E, Lee CM, Wilcox ME, Ayas N, Choong K, Fowler R, Scales DC, Sinuff T, Cuthbertson BH, Rose L, Robles P, Burns S, Cypel M, Singer L, Chaparro C, Chow C-W, Keshavjee S, Brochard L, Hébert P, Slutsky AS, Marshall JC, Cook D, Herridge MS. One-year outcomes in caregivers of critically ill patients. N Engl J Med. 2016;374(19):1831–41. https://doi.org/10.1056/NEJMoa1511160.
Herridge MS, Moss M, Hough CL, et al. Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers. Intensive Care Med. 2016;42(5). https://doi.org/10.1007/s00134-016-4321-8.
Brück E, Schandl A, Bottai M, Sackey P. The impact of sepsis, delirium, and psychological distress on self-rated cognitive function in ICU survivors-a prospective cohort study. J Intensive Care. 2018;6(1). https://doi.org/10.1186/s40560-017-0272-6.
Teixeira C, Rosa RG. Post-intensive care outpatient clinic: is it feasible and effective? A literature review. Rev Bras Ter Intensiva. 2018;30(1). https://doi.org/10.5935/0103-507X.20180016.
Kuehn BM. Clinics aim to improve post-ICU recovery. JAMA-J Am Med Assoc. 2019;321(11). https://doi.org/10.1001/jama.2019.0420.
Sevin CM, Jackson JC. Post-ICU clinics should be staffed by ICU clinicians. Crit Care Med. 2019;47(2). https://doi.org/10.1097/CCM.0000000000003535.
Herridge MS, Chu LM, Matte A, et al. The RECOVER program: disability risk groups and 1-year outcome after 7 or more days of mechanical ventilation. Am J Respir Crit Care Med. 2016;194(7). https://doi.org/10.1164/rccm.201512-2343OC.
Prescott HC, Angus DC. Enhancing recovery from sepsis: a review. JAMA – J Am Med Assoc. 2018;319(1). https://doi.org/10.1001/jama.2017.17687.
Brown SM, Dinglas VD, Akhlaghi N, et al. Association between unmet medication needs after hospital discharge and readmission or death among acute respiratory failure survivors: the addressing post-intensive care syndrome (APICS-01) multicenter prospective cohort study. Crit Care. 2022;26(1). https://doi.org/10.1186/s13054-021-03848-3.
Taylor SP, Chou SH, Sierra MF, et al. Association between adherence to recommended care and outcomes for adult survivors of sepsis. Ann Am Thorac Soc. 2020;17(1). https://doi.org/10.1513/AnnalsATS.201907-514OC.
• LaBuzetta JN, Rosand J, Vranceanu AM. Review: post-intensive care syndrome: unique challenges in the neurointensive care unit. Neurocrit Care. 2019;31(3). https://doi.org/10.1007/s12028-019-00826-0. This paper provides of review of the neuoropsychological sequelae of ICU admission in the neurocritical care population.
Hwang DY, Yagoda D, Perrey HM, et al. Anxiety and depression symptoms among families of adult intensive care unit survivors immediately following brief length of stay. J Crit Care. 2014;29(2). https://doi.org/10.1016/j.jcrc.2013.11.022.
Trevick SA, Lord AS. Post-traumatic Stress Disorder and Complicated Grief are Common in Caregivers of Neuro-ICU Patients. Neurocrit Care. 2017;26(3). https://doi.org/10.1007/s12028-016-0372-5.
Meyers EE, Presciutti A, Shaffer KM, et al. The impact of resilience factors and anxiety during hospital admission on longitudinal anxiety among dyads of neurocritical care patients without major cognitive impairment and their family caregivers. Neurocrit Care. 2020;33(2):468–78. https://doi.org/10.1007/s12028-020-00913-7.
• Hwang DY. Is post-neurointensive care syndrome actually a thing? Neurocrit Care. 2019;31(3). https://doi.org/10.1007/s12028-019-00827-z. The author questions whether PICS terminology can be applied in the neurointensive care population and highlights the clear evidence for PICS-F in this population.
Bakas T, McCarthy MJ, Miller EL. Systematic review of the evidence for stroke family caregiver and dyad interventions. Stroke. 2022;53(6). https://doi.org/10.1161/STROKEAHA.121.034090.
Badr H, Krebs P. A systematic review and meta-analysis of psychosocial interventions for couples coping with cancer. Psychooncology. 2013;22(8). https://doi.org/10.1002/pon.3200.
von Heymann-Horan A, Bidstrup P, Guldin MB, et al. Effect of home-based specialised palliative care and dyadic psychological intervention on caregiver anxiety and depression: a randomised controlled trial. Br J Cancer. 2018;119(11). https://doi.org/10.1038/s41416-018-0193-8.
•• Vranceanu AM, Bannon S, Mace R, et al. Feasibility and efficacy of a resiliency intervention for the prevention of chronic emotional distress among survivor-caregiver dyads admitted to the neuroscience intensive care unit: a randomized clinical trial. JAMA Netw Open. 2020;3(10). https://doi.org/10.1001/jamanetworkopen.2020.20807. This is a pilot randomized control trial in one neuroscience unit showing that dyadic resiliency training is feasible and reduced symptoms of anxiety, depression, and post-traumatic stress.
McCurley JL, Funes CJ, Zale EL, et al. Preventing chronic emotional distress in stroke survivors and their informal caregivers. Neurocrit Care. 2019;30(3). https://doi.org/10.1007/s12028-018-0641-6.
Zarino B, Bertani G, Conte V, Magnoni S, Cristofori A di, Stocchetti N. Time course of neuropsychological functioning after aneurysmal subarachnoid hemorrhage. Crit Care. 2013;17(S2). https://doi.org/10.1186/cc12282.
Lindner A, Brunelli L, Rass V, et al. Long-term clinical trajectory of patients with subarachnoid hemorrhage: linking acute care and neurorehabilitation. Neurocrit Care. 2023;38:138–148. https://doi.org/10.1007/s12028-022-01572-6.
J. VM, P. A, V. S, M. P, G. R, P. P. Depressive symptoms and anxiety up to three years after subarachnoid haemorrhage: prevalence and prediction. Cerebrovascular Diseases. 2012;33:341–342. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed12&NEWS=N&AN=71637192
Ackermark YIP, Schepers VPM, Post MWM, Rinkel GJE, Passier PECA, Visser-Meily JMA. Longitudinal course of depressive symptoms and anxiety after aneurysmal subarachnoid hemorrhage. Eur J Phys Rehabil Med. 2017;53(1). https://doi.org/10.23736/S1973-9087.16.04202-7.
Cheng EM, Cunningham WE, Towfighi A, et al. Efficacy of a chronic care-based intervention on secondary stroke prevention among vulnerable stroke survivors: a randomized controlled trial. Circ Cardiovasc Qual Outcomes. 2018;11(1). https://doi.org/10.1161/CIRCOUTCOMES.116.003228.
Nelson LD, Temkin NR, Dikmen S, et al. Recovery after mild traumatic brain injury in patients presenting to US level I trauma centers: a transforming research and clinical knowledge in traumatic brain injury (TRACK-TBI) study. JAMA Neurol. 2019;76(9). https://doi.org/10.1001/jamaneurol.2019.1313.
•• Fann JR, Hart T, Ciol MA, et al. Improving transition from inpatient rehabilitation following traumatic brain injury: protocol for the BRITE pragmatic comparative effectiveness trial. Contemp Clin Trials. 2021;104. https://doi.org/10.1016/j.cct.2021.106332. This ongoing trial is examining the impact of a rehabilitation transition plan on patient and caregiver reported outcomes and healthcare utilization.
•• National Institute for Health and Care Excellence. Rehabilitation after critical illness in adults | Guidance and guidelines | NICE. NICE Guideline 83. n.d. Published online 2009. The UK has set rehabilitation guidelines as a quality standard after critical illness.
Sevin CM, Bloom SL, Jackson JC, Wang L, Wesley Ely E, Stollings JL. Comprehensive care of ICU survivors: development and implementation of an ICU recovery center. J Crit Care. 2018;46. https://doi.org/10.1016/j.jcrc.2018.02.011.
van Schaaf M der, Bakhshi-Raiez F, van der Steen M, Dongelmans DA, de Keizer NF. Recommendations for intensive care follow-up clinics; Report from a survey and conference of Dutch intensive cares. Minerva Anestesiol. 2015;81(2). https://www.minervamedica.it/en/journals/minerva-anestesiologica/article.php?cod=R02Y2015N02A0135.
Rosa RG, Kochhann R, Berto P, et al. More than the tip of the iceberg: association between disabilities and inability to attend a clinic-based post-ICU follow-up and how it may impact on health inequalities. Intensive Care Med. 2018;44(8). https://doi.org/10.1007/s00134-018-5146-4.
Kubota R, Meurer K, Baskaran N, et al. Coping strategies and psychosocial resource needs reported by families of patients recovering from coma in neurointensive care units: preliminary findings from a multicenter qualitative study (RP423). J Pain Symptom Manage. 2022;63(6):1095–6. https://doi.org/10.1016/j.jpainsymman.2022.04.064.
Donaghy E, Salisbury L, Lone NI, et al. Unplanned early hospital readmission among critical care survivors: a mixed methods study of patients and carers. BMJ Qual Saf. 2018;27(11). https://doi.org/10.1136/bmjqs-2017-007513.
Bloom SL, Stollings JL, Kirkpatrick O, et al. Randomized clinical trial of an ICU recovery pilot program for survivors of critical illness. Crit Care Med. 2019;47(10). https://doi.org/10.1097/CCM.0000000000003909.
Rousseau AF, Prescott HC, Brett SJ, et al. Long-term outcomes after critical illness: recent insights. Crit Care. 2021;25(1). https://doi.org/10.1186/s13054-021-03535-3.
• Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11). https://doi.org/10.1016/j.jclinepi.2010.04.011. This study describes the development of the PROMIS.
Naidech AM, Beaumont JL, Berman M, et al. Web-based assessment of outcomes after subarachnoid and intracerebral hemorrhage: a new patient centered option for outcomes assessment. Neurocrit Care. 2015;23(1). https://doi.org/10.1007/s12028-014-0098-1.
Giacino JT, Fins JJ, Laureys S, Schiff ND. Disorders of consciousness after acquired brain injury: the state of the science. Nat Rev Neurol. 2014;10(2). https://doi.org/10.1038/nrneurol.2013.279.
Haines KJ, Sevin CM, Hibbert E, et al. Key mechanisms by which post-ICU activities can improve in-ICU care: results of the international THRIVE collaboratives. Intensive Care Med. 2019;45(7). https://doi.org/10.1007/s00134-019-05647-5.
Jaffa MN, Podell JE, Motta M. A change of course: the case for a neurorecovery clinic. Neurocrit Care. 2020;33(2). https://doi.org/10.1007/s12028-020-00976-6.
Author information
Authors and Affiliations
Contributions
Vanessa Salasky, MD performed the literature search and drafted and revised the work. Matthew N. Jaffa, DO critically revised the work and approved the version to be published. Melissa Motta, MD critically revised the work and approved the version to be published. Gunjan Y. Parikh, MD made substantial contributions to the conception of and ideas for the article and critically revised the work for important intellectual content and approved the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salasky, V., Jaffa, M.N., Motta, M. et al. Neurocritical Care Recovery Clinics: An Idea Whose Time Has Come. Curr Neurol Neurosci Rep 23, 159–166 (2023). https://doi.org/10.1007/s11910-023-01256-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-023-01256-4