Abstract
Purpose of Review
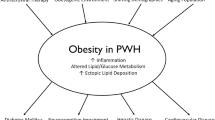
This review reports on published studies describing metabolic changes associated with antiretroviral therapy (ART) to treat HIV disease including a historical perspective of earlier ART agents, but with the main focus on newer ART agents currently in use.
Recent Findings
Studies from different countries around the world have shown that integrase inhibitor (INSTI)-based regimens as well as tenofovir alafenamide (TAF) are associated with weight gain, with women and people of black race at especially high risk. Some studies preliminarily suggest worsened metabolic outcomes associated with this weight gain including adverse effects on glucose homeostasis.
Summary
Antiretroviral therapy can affect weight, adipose tissue, glucose, and lipids. As obesity is prevalent and increasing among people with HIV, awareness of risk factors for weight gain, including the ART medications associated with greater weight gain, are needed in order to inform prevention efforts. Further research is needed to better understand the long-term health consequences of INSTI- and TAF-associated weight increases.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Walensky RP, Paltiel AD, Losina E, Mercincavage LM, Schackman BR, Sax PE, et al. The survival benefits of AIDS treatment in the United States. J Infect Dis. 2006;194(1):11–9. https://doi.org/10.1086/505147.
Joly V, Flandre P, Meiffredy V, Leturque N, Harel M, Aboulker JP, et al. Increased risk of lipoatrophy under stavudine in HIV-1-infected patients: results of a substudy from a comparative trial. AIDS. 2002;16(18):2447–54. https://doi.org/10.1097/00002030-200212060-00010.
Carr A, Workman C, Smith DE, Hoy J, Hudson J, Doong N, et al. Abacavir substitution for nucleoside analogs in patients with HIV lipoatrophy: a randomized trial. JAMA. 2002;288(2):207–15. https://doi.org/10.1001/jama.288.2.207.
van Vonderen MG, van Agtmael MA, Hassink EA, Milinkovic A, Brinkman K, Geerlings SE, et al. Zidovudine/lamivudine for HIV-1 infection contributes to limb fat loss. PLoS ONE. 2009;4(5): e5647. https://doi.org/10.1371/journal.pone.0005647.
Bogner JR, Vielhauer V, Beckmann RA, Michl G, Wille L, Salzberger B, et al. Stavudine versus zidovudine and the development of lipodystrophy. J Acquir Immune Defic Syndr. 2001;27(3):237–44. https://doi.org/10.1097/00126334-200107010-00004.
Carr A, Samaras K, Burton S, Law M, Freund J, Chisholm DJ, et al. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS. 1998;12(7):F51–8. https://doi.org/10.1097/00002030-199807000-00003.
Crane HM, Grunfeld C, Willig JH, Mugavero MJ, Van Rompaey S, Moore R, et al. Impact of NRTIs on lipid levels among a large HIV-infected cohort initiating antiretroviral therapy in clinical care. AIDS. 2011;25(2):185–95. https://doi.org/10.1097/QAD.0b013e328341f925.
Valantin MA, Bittar R, de Truchis P, Bollens D, Slama L, Giral P, et al. Switching the nucleoside reverse transcriptase inhibitor backbone to tenofovir disoproxil fumarate + emtricitabine promptly improves triglycerides and low-density lipoprotein cholesterol in dyslipidaemic patients. J Antimicrob Chemother. 2010;65(3):556–61. https://doi.org/10.1093/jac/dkp462.
Riddler SA, Li X, Chu H, Kingsley LA, Dobs A, Evans R, et al. Longitudinal changes in serum lipids among HIV-infected men on highly active antiretroviral therapy. HIV Med. 2007;8(5):280–7. https://doi.org/10.1111/j.1468-1293.2007.00470.x.
Periard D, Telenti A, Sudre P, Cheseaux JJ, Halfon P, Reymond MJ, et al. Atherogenic dyslipidemia in HIV-infected individuals treated with protease inhibitors. The Swiss HIV Cohort Study. Circulation. 1999;100(7):700–5. https://doi.org/10.1161/01.cir.100.7.700.
De Wit S, Sabin CA, Weber R, Worm SW, Reiss P, Cazanave C, et al. Incidence and risk factors for new-onset diabetes in HIV-infected patients: the Data collection on adverse events of anti-HIV drugs (D:A:D) study. Diabetes Care. 2008;31(6):1224–9. https://doi.org/10.2337/dc07-2013.
Koethe JR, Lagathu C, Lake JE, Domingo P, Calmy A, Falutz J, et al. HIV and antiretroviral therapy-related fat alterations. Nat Rev Dis Primers. 2020;6(1):48. https://doi.org/10.1038/s41572-020-0181-1.
Grinspoon S, Carr A. Cardiovascular risk and body-fat abnormalities in HIV-infected adults. N Engl J Med. 2005;352(1):48–62. https://doi.org/10.1056/NEJMra041811.
Ledergerber B, Furrer H, Rickenbach M, Lehmann R, Elzi L, Hirschel B, et al. Factors associated with the incidence of type 2 diabetes mellitus in HIV-infected participants in the Swiss HIV Cohort Study. Clin Infect Dis. 2007;45(1):111–9. https://doi.org/10.1086/518619.
• Bourgi K, Rebeiro PF, Turner M, Castilho JL, Hulgan T, Raffanti SP, et al. Greater weight gain in treatment-naive persons starting dolutegravir-based antiretroviral therapy. Clin Infect Dis. 2020;70(7):1267–74. https://doi.org/10.1093/cid/ciz407. In a cohort of 1152 PLWH initiating PIs (39%), NNRTIs (30%), or INSTIs (30%), DTG was shown to be associated with significantly greater increases in body mass compared with NNRTIs. Comparisons among INSTI-based regimens showed greater weight gain on either DTG or RAL than EVG after 6 and 18 months. Importantly, DTG and EVG were associated with the most and least weight gain, respectively, among all ART regimens, underscoring the importance of investing metabolic consequences not only between ART classes, but within them.
Koethe JR, Jenkins CA, Lau B, Shepherd BE, Justice AC, Tate JP, et al. Rising obesity prevalence and weight gain among adults starting antiretroviral therapy in the United States and Canada. AIDS Res Hum Retroviruses. 2016;32(1):50–8. https://doi.org/10.1089/aid.2015.0147.
World Health Organization. Update of Recommendations on First- and Second-Line Antiretroviral Regimens. World Health Organization, Geneva, Switzerland. 2019 (WHO/CDS/HIV/19.15). https://apps.who.int/iris/bitstream/handle/10665/325892/WHO-CDS-HIV-19.15-eng.pdf. Accessed 1 Mar 2022.
U.S. Department of Health and Human Services Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV: What to Start: Initial Combination Regimens for the Antiretroviral-Naive Patient. 2021. https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-arv/what-start-initial-combination-regimens-antiretroviral-naive?view=full. Accessed 1 Mar 2022.
•• Venter WDF, Sokhela S, Simmons B, Moorhouse M, Fairlie L, Mashabane N, et al. Dolutegravir with emtricitabine and tenofovir alafenamide or tenofovir disoproxil fumarate versus efavirenz, emtricitabine, and tenofovir disoproxil fumarate for initial treatment of HIV-1 infection (ADVANCE): week 96 results from a randomised, phase 3, non-inferiority trial. Lancet HIV. 2020;7(10):e666–76. https://doi.org/10.1016/S2352-3018(20)30241-1. This 96-week, phase 3 randmoized trial found that people who started ART on DTG/FTC/TAF or DTG/FTC/TDF experienced greater increases in body mass compared with people who started ART on EFV/FTC/TDF. Differences were only significant between DTG/FTC/TAF and EFV/FTC/TDF, suggesting that DTG and TAF taken together may have additive effects on body mass.
•• Sax PE, Erlandson KM, Lake JE, McComsey GA, Orkin C, Esser S, et al. weight gain following initiation of antiretroviral therapy: risk factors in randomized comparative clinical trials. Clin Infect Dis. 2020;71(6):1379–89. https://doi.org/10.1093/cid/ciz999. In this pooled analysis of eight phase 3 clinical trials, PLWH starting ART on INSTIs were found to experience greater weight gain compared with those starting ART on PIs or NNRTIs. Similarly, PLWH initiating a TAF-containing regimen were found to gain more weight than PLWH initiating other NRTIs, particularly ZDV. These findings are in line with recent studies showing elevated weight gain in association with TAF and/or INSTI use. In full cohort analyses, ART-associated weight gain was found to be particularly pronounced (increasing by 10% or more) among females, Black individuals, and people with lower body mass, fewer CD4+ T cells, and/or greater HIV-1 RNA levels at ART initiation.
•• Surial B, Mugglin C, Calmy A, Cavassini M, Gunthard HF, Stockle M, et al. Weight and metabolic changes after switching from tenofovir disoproxil fumarate to tenofovir alafenamide in people living with HIV : a cohort study. Ann Intern Med. 2021;174(6):758–67. https://doi.org/10.7326/M20-4853. In this switch study, PLWH who transitioned from TDF to TAF—particularly women and people of African origin—experienced significantly greater weight gain, on average, compared to those who remained on TDF, regardless of whether they took an INSTI, NNRTI, or PI in combination. Total, HDL, and LDL cholesterol levels were also found to rise only among people who transitioned to TAF, suggesting that TAF initiation and/or TDF termination is associated with dyslipidemia. Total cholesterol-to-HDL ratio and rates of diabetes development, however, did not differ between those who switched to TAF vs. remained on TDF, making the long-term cardiometabolic consequences of TAF unclear.
Carr A, Cooper DA. Images in clinical medicine. Lipodystrophy associated with an HIV-protease inhibitor. N Engl J Med. 1998;339(18):1296. https://doi.org/10.1056/NEJM199810293391806.
Chen D, Misra A, Garg A. Clinical review 153: Lipodystrophy in human immunodeficiency virus-infected patients. J Clin Endocrinol Metab. 2002;87(11):4845–56. https://doi.org/10.1210/jc.2002-020794.
Mallon PW, Miller J, Cooper DA, Carr A. Prospective evaluation of the effects of antiretroviral therapy on body composition in HIV-1-infected men starting therapy. AIDS. 2003;17(7):971–9. https://doi.org/10.1097/00002030-200305020-00005.
Dube MP, Komarow L, Mulligan K, Grinspoon SK, Parker RA, Robbins GK, et al. Long-term body fat outcomes in antiretroviral-naive participants randomized to nelfinavir or efavirenz or both plus dual nucleosides. Dual X-ray absorptiometry results from A5005s, a substudy of Adult Clinical Trials Group 384. J Acquir Immune Defic Syndr. 2007;45(5):508–14. https://doi.org/10.1097/QAI.0b013e3181142d26.
Han SH, Zhou J, Saghayam S, Vanar S, Phanuphak N, Chen YM, et al. Prevalence of and risk factors for lipodystrophy among HIV-infected patients receiving combined antiretroviral treatment in the Asia-Pacific region: results from the TREAT Asia HIV Observational Database (TAHOD). Endocr J. 2011;58(6):475–84. https://doi.org/10.1507/endocrj.k10e-407.
van Oosterhout JJ, Mallewa J, Kaunda S, Chagoma N, Njalale Y, Kampira E, et al. Stavudine toxicity in adult longer-term ART patients in Blantyre, Malawi. PLoS ONE. 2012;7(7): e42029. https://doi.org/10.1371/journal.pone.0042029.
Ammassari A, Antinori A, Cozzi-Lepri A, Trotta MP, Nasti G, Ridolfo AL, et al. Relationship between HAART adherence and adipose tissue alterations. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S140–4. https://doi.org/10.1097/00126334-200212153-00011.
World Health Organization. Rapid Advice: Antiretroviral therapy for HIV infection in adults and adolescents. 2009. https://www.who.int/hiv/pub/arv/rapid_advice_art.pdf. Accessed 1 Mar 2022.
Ruderman SA, Crane HM, Nance RM, Whitney BM, Harding BN, Mayer KH, et al. Brief report: weight gain following ART initiation in ART-naive people living with HIV in the current treatment era. J Acquir Immune Defic Syndr. 2021;86(3):339–43. https://doi.org/10.1097/QAI.0000000000002556.
• Calmy A, Tovar Sanchez T, Kouanfack C, Mpoudi-Etame M, Leroy S, Perrineau S, et al. Dolutegravir-based and low-dose efavirenz-based regimen for the initial treatment of HIV-1 infection (NAMSAL): week 96 results from a two-group, multicentre, randomised, open label, phase 3 non-inferiority trial in Cameroon. Lancet HIV. 2020;7(10):e677–87. https://doi.org/10.1016/S2352-3018(20)30238-1. This 96-week, phase 3 study found that people initiating ART on DTG/3TC/TDF (n = 310) gained significantly more weight and were more likely to develop obesity compared with people initiating ART on EFV/3TC/TDF (n = 303).
• Kerchberger AM, Sheth AN, Angert CD, Mehta CC, Summers NA, Ofotokun I, et al. Weight gain associated with integrase stand transfer inhibitor use in women. Clin Infect Dis. 2020;71(3):593–600. https://doi.org/10.1093/cid/ciz853. This cohort study of 1118 women living with HIV found that increases in body weight, BMI, percent body fat, waist circumference, arm circumference, and thigh circumference were significantly higher among women who started on INSTIs (either instead of or in addition to their prior ART regimen) compared to women who remained on non-INSTI-based ART. These findings provide important insights into INSTI-associated changes not only in overall body weight, but also in body composition.
Bakal DR, Coelho LE, Luz PM, Clark JL, De Boni RB, Cardoso SW, et al. Obesity following ART initiation is common and influenced by both traditional and HIV-/ART-specific risk factors. J Antimicrob Chemother. 2018;73(8):2177–85. https://doi.org/10.1093/jac/dky145.
Eckard AR, McComsey GA. Weight gain and integrase inhibitors. Curr Opin Infect Dis. 2020;33(1):10–9. https://doi.org/10.1097/QCO.0000000000000616.
Summers NA, Lahiri CD, Angert CD, Aldredge A, Mehta CC, Ofotokun I, et al. Metabolic changes associated with the use of integrase strand transfer inhibitors among virally controlled women. J Acquir Immune Defic Syndr. 2020;85(3):355–62. https://doi.org/10.1097/QAI.0000000000002447.
Norwood J, Turner M, Bofill C, Rebeiro P, Shepherd B, Bebawy S, et al. Brief report: weight gain in persons with HIV switched from Efavirenz-Based to integrase strand transfer inhibitor-based regimens. J Acquir Immune Defic Syndr. 2017;76(5):527–31. https://doi.org/10.1097/QAI.0000000000001525.
Taramasso L, Ricci E, Menzaghi B, Orofino G, Passerini S, Madeddu G, et al. Weight gain: a possible side effect of all antiretrovirals. Open Forum Infect Dis. 2017;4(4):ofx239. https://doi.org/10.1093/ofid/ofx239.
Bourgi K, Jenkins CA, Rebeiro PF, Palella F, Moore RD, Altoff KN, et al. Weight gain among treatment-naive persons with HIV starting integrase inhibitors compared to non-nucleoside reverse transcriptase inhibitors or protease inhibitors in a large observational cohort in the United States and Canada. J Int AIDS Soc. 2020;23(4): e25484. https://doi.org/10.1002/jia2.25484.
Burns JE, Stirrup OT, Dunn D, Runcie-Unger I, Milinkovic A, Candfield S, et al. No overall change in the rate of weight gain after switching to an integrase-inhibitor in virologically suppressed adults with HIV. AIDS. 2020;34(1):109–14. https://doi.org/10.1097/QAD.0000000000002379.
Landovitz RJ, Zangeneh SZ, Chau G, Grinsztejn B, Eron JJ, Dawood H, et al. Cabotegravir is not associated with weight gain in human immunodeficiency virus-uninfected individuals in HPTN 077. Clin Infect Dis. 2020;70(2):319–22. https://doi.org/10.1093/cid/ciz439.
U.S. Department of Health and Human Services Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents Living with HIV: Integrase Strand Transfer Inhibitor-Based Regimens. 2021. https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-arv/integrase-strand-transfer-inhibitor-based-regimens?view=full. Accessed 1 Mar 2022.
Lake JE, Wu K, Bares SH, Debroy P, Godfrey C, Koethe JR, et al. Risk factors for weight gain following switch to integrase inhibitor-based antiretroviral therapy. Clin Infect Dis. 2020;71(9):e471–7. https://doi.org/10.1093/cid/ciaa177.
Lahiri CD, Xu Y, Wang K, Alvarez JA, Sheth AN, O’Halloran J, et al. weight and body mass index change after switching to integrase inhibitors or tenofovir alafenamide among women living with HIV. AIDS Res Hum Retroviruses. 2021;37(6):461–7. https://doi.org/10.1089/AID.2020.0197.
Ruiz-Castell M, Samouda H, Bocquet V, Fagherazzi G, Stranges S, Huiart L. Estimated visceral adiposity is associated with risk of cardiometabolic conditions in a population based study. Sci Rep. 2021;11(1):9121. https://doi.org/10.1038/s41598-021-88587-9.
Lake JE. The fat of the matter: obesity and visceral adiposity in treated HIV infection. Curr HIV/AIDS Rep. 2017;14(6):211–9. https://doi.org/10.1007/s11904-017-0368-6.
Despres JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28(6):1039–49. https://doi.org/10.1161/ATVBAHA.107.159228.
Kammerlander AA, Lyass A, Mahoney TF, Massaro JM, Long MT, Vasan RS, et al. Sex differences in the associations of visceral adipose tissue and cardiometabolic and cardiovascular disease risk: The Framingham Heart Study. J Am Heart Assoc. 2021;10(11): e019968. https://doi.org/10.1161/JAHA.120.019968.
Ofotokun I, Na LH, Landovitz RJ, Ribaudo HJ, McComsey GA, Godfrey C, et al. Comparison of the metabolic effects of ritonavir-boosted darunavir or atazanavir versus raltegravir, and the impact of ritonavir plasma exposure: ACTG 5257. Clin Infect Dis. 2015;60(12):1842–51. https://doi.org/10.1093/cid/civ193.
Bhagwat P, Ofotokun I, McComsey GA, Brown TT, Moser C, Sugar CA, et al. Changes in waist circumference in HIV-infected individuals initiating a raltegravir or protease inhibitor regimen: effects of sex and race. Open Forum Infect Dis. 2018;5(11):ofy201. https://doi.org/10.1093/ofid/ofy201.
Domingo P, Gutierrez Mdel M, Gallego-Escuredo JM, Torres F, Mateo GM, Villarroya J, et al. Effects of switching from stavudine to raltegravir on subcutaneous adipose tissue in HIV-infected patients with HIV/HAART-associated lipodystrophy syndrome (HALS). A clinical and molecular study. PLoS One. 2014;9(2):e89088. https://doi.org/10.1371/journal.pone.0089088.
McComsey GA, Moser C, Currier J, Ribaudo HJ, Paczuski P, Dube MP, et al. Body composition changes after initiation of raltegravir or protease inhibitors: ACTG A5260s. Clin Infect Dis. 2016;62(7):853–62. https://doi.org/10.1093/cid/ciw017.
Schafer JJ, Sassa KN, O’Connor JR, Shimada A, Keith SW, DeSimone JA. Changes in body mass index and atherosclerotic disease risk score after switching from tenofovir disoproxil fumarate to tenofovir alafenamide. Open Forum Infect Dis. 2019;6(10):ofz414. https://doi.org/10.1093/ofid/ofz414.
Gomez M, Seybold U, Roider J, Harter G, Bogner JR. A retrospective analysis of weight changes in HIV-positive patients switching from a tenofovir disoproxil fumarate (TDF)- to a tenofovir alafenamide fumarate (TAF)-containing treatment regimen in one German university hospital in 2015–2017. Infection. 2019;47(1):95–102. https://doi.org/10.1007/s15010-018-1227-0.
Kileel EM, Lo J, Malvestutto C, Fitch KV, Zanni MV, Fichtenbaum CJ, et al. Assessment of obesity and cardiometabolic status by integrase inhibitor use in reprieve: a propensity-weighted analysis of a multinational primary cardiovascular prevention cohort of people with human immunodeficiency virus. Open Forum Infect Dis. 2021;8(12):ofab537. https://doi.org/10.1093/ofid/ofab537.
Kumar S, Samaras K. The impact of weight gain during HIV treatment on risk of pre-diabetes, diabetes mellitus, cardiovascular disease, and mortality. Front Endocrinol (Lausanne). 2018;9:705. https://doi.org/10.3389/fendo.2018.00705.
O’Brien ME, Clark RA, Besch CL, Myers L, Kissinger P. Patterns and correlates of discontinuation of the initial HAART regimen in an urban outpatient cohort. J Acquir Immune Defic Syndr. 2003;34(4):407–14. https://doi.org/10.1097/00126334-200312010-00008.
Glidden DV, Mulligan K, McMahan V, Anderson PL, Guanira J, Chariyalertsak S, et al. metabolic effects of preexposure prophylaxis with coformulated tenofovir disoproxil fumarate and emtricitabine. Clin Infect Dis. 2018;67(3):411–9. https://doi.org/10.1093/cid/ciy083.
Domingo P, Villarroya F, Giralt M, Domingo JC. Potential role of the melanocortin signaling system interference in the excess weight gain associated to some antiretroviral drugs in people living with HIV. Int J Obes (Lond). 2020;44(9):1970–3. https://doi.org/10.1038/s41366-020-0551-5.
McMahon C, Trevaskis JL, Carter C, Holsapple K, White K, Das M, et al. Lack of an association between clinical INSTI-related body weight gain and direct interference with MC4 receptor (MC4R), a key central regulator of body weight. PLoS ONE. 2020;15(2): e0229617. https://doi.org/10.1371/journal.pone.0229617.
Pickering R, Asundi A, Lin N. In Vitro model to assess antiretroviral therapy on adipocyte biology [abstract 514]. In: Conference on Retroviruses and Opportunistic Infections, Virtual. 2021.
European Medicines Agency Committee for Medicinal Products for Human Use. Tivicay Assessment report. 2014. https://www.ema.europa.eu/en/documents/assessment-report/tivicay-epar-public-assessment-report_en.pdf. Accessed 1 Mar 2022.
Gorwood J, Bourgeois C, Pourcher V, Pourcher G, Charlotte F, Mantecon M, et al. The integrase inhibitors dolutegravir and raltegravir exert proadipogenic and profibrotic effects and induce insulin resistance in human/simian adipose tissue and human adipocytes. Clin Infect Dis. 2020;71(10):e549–60. https://doi.org/10.1093/cid/ciaa259.
Jung I, Jin S, Tu-Sekine B, Anokye-Danso F, Brown T, Kim S. Integrase inhibitors target mitochondria in brown adipocytes disrupting thermogenesis [abstract 515]. In: Conference on Retroviruses and Opportunistic Infections, Virtual. 2021.
Tien PC, Schneider MF, Cole SR, Levine AM, Cohen M, DeHovitz J, et al. Antiretroviral therapy exposure and incidence of diabetes mellitus in the Women’s Interagency HIV Study. AIDS. 2007;21(13):1739–45. https://doi.org/10.1097/QAD.0b013e32827038d0.
Blumer RM, van Vonderen MG, Sutinen J, Hassink E, Ackermans M, van Agtmael MA, et al. Zidovudine/lamivudine contributes to insulin resistance within 3 months of starting combination antiretroviral therapy. AIDS. 2008;22(2):227–36. https://doi.org/10.1097/QAD.0b013e3282f33557.
Fleischman A, Johnsen S, Systrom DM, Hrovat M, Farrar CT, Frontera W, et al. Effects of a nucleoside reverse transcriptase inhibitor, stavudine, on glucose disposal and mitochondrial function in muscle of healthy adults. Am J Physiol Endocrinol Metab. 2007;292(6):E1666–73. https://doi.org/10.1152/ajpendo.00550.2006.
Murata H, Hruz PW, Mueckler M. The mechanism of insulin resistance caused by HIV protease inhibitor therapy. J Biol Chem. 2000;275(27):20251–4. https://doi.org/10.1074/jbc.C000228200.
Rebeiro PF, Jenkins CA, Bian A, Lake JE, Bourgi K, Moore RD, et al. Risk of incident diabetes mellitus, weight gain, and their relationships with integrase inhibitor-based initial antiretroviral therapy among persons with HIV in the US and Canada. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa1403.
Dirajlal-Fargo S, Moser C, Brown TT, Kelesidis T, Dube MP, Stein JH, et al. Changes in insulin resistance after initiation of raltegravir or protease inhibitors with tenofovir-emtricitabine: AIDS Clinical Trials Group A5260s. Open Forum Infect Dis. 2016;3(3):ofw174. https://doi.org/10.1093/ofid/ofw174.
McLaughlin M, Walsh S, Galvin S. Dolutegravir-induced hyperglycaemia in a patient living with HIV. J Antimicrob Chemother. 2018;73(1):258–60. https://doi.org/10.1093/jac/dkx365.
Fong PS, Flynn DM, Evans CD, Korthuis PT. Integrase strand transfer inhibitor-associated diabetes mellitus: A case report. Int J STD AIDS. 2017;28(6):626–8. https://doi.org/10.1177/0956462416675107.
Nolan NS, Adamson S, Reeds D, O’Halloran JA. Bictegravir-based antiretroviral therapy-associated accelerated hyperglycemia and diabetes mellitus. Open Forum Infect Dis. 2021;8(5):ofab077. https://doi.org/10.1093/ofid/ofab077.
Kamei S, Kaneto H, Hashiramoto M, Hisano Y, Tanabe A, Shimoda M, et al. Case of newly onset type 1 diabetes after highly active antiretroviral therapy against HIV infection. J Diabetes Investig. 2015;6(3):367–8. https://doi.org/10.1111/jdi.12286.
Hailu W, Tesfaye T, Tadesse A. Hyperglycemia after dolutegravir-based antiretroviral therapy. Int Med Case Rep J. 2021;14:503–7. https://doi.org/10.2147/IMCRJ.S323233.
Lamorde M, Atwiine M, Owarwo NC, Ddungu A, Laker EO, Mubiru F, et al. Dolutegravir-associated hyperglycaemia in patients with HIV. Lancet HIV. 2020;7(7):e461–2. https://doi.org/10.1016/S2352-3018(20)30042-4.
Lennox JL, Dejesus E, Berger DS, Lazzarin A, Pollard RB, Ramalho Madruga JV, et al. Raltegravir versus Efavirenz regimens in treatment-naive HIV-1-infected patients: 96-week efficacy, durability, subgroup, safety, and metabolic analyses. J Acquir Immune Defic Syndr. 2010;55(1):39–48. https://doi.org/10.1097/QAI.0b013e3181da1287.
Lewis W, Day BJ, Copeland WC. Mitochondrial toxicity of NRTI antiviral drugs: an integrated cellular perspective. Nat Rev Drug Discov. 2003;2(10):812–22. https://doi.org/10.1038/nrd1201.
Sangwung P, Petersen KF, Shulman GI, Knowles JW. Mitochondrial dysfunction, insulin resistance, and potential genetic implications. Endocrinology. 2020;161(4). https://doi.org/10.1210/endocr/bqaa017.
Patti ME, Butte AJ, Crunkhorn S, Cusi K, Berria R, Kashyap S, et al. Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: Potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A. 2003;100(14):8466–71. https://doi.org/10.1073/pnas.1032913100.
Woerle HJ, Mariuz PR, Meyer C, Reichman RC, Popa EM, Dostou JM, et al. Mechanisms for the deterioration in glucose tolerance associated with HIV protease inhibitor regimens. Diabetes. 2003;52(4):918–25. https://doi.org/10.2337/diabetes.52.4.918.
Hulgan T. Factors Associated With Insulin Resistance in Adults With HIV Receiving contemporary antiretroviral therapy: a brief update. Curr HIV/AIDS Rep. 2018;15(3):223–32. https://doi.org/10.1007/s11904-018-0399-7.
Korencak M, Byrne M, Richter E, Schultz BT, Juszczak P, Ake JA, et al. Effect of HIV infection and antiretroviral therapy on immune cellular functions. JCI Insight. 2019;4(12). https://doi.org/10.1172/jci.insight.126675.
Zhang E, Chai JC, Deik AA, Hua S, Sharma A, Schneider MF, et al. Plasma lipidomic profiles and risk of diabetes: 2 prospective cohorts of HIV-infected and HIV-uninfected individuals. J Clin Endocrinol Metab. 2021;106(4):999–1010. https://doi.org/10.1210/clinem/dgab011.
Lo J. Dyslipidemia and lipid management in HIV-infected patients. Curr Opin Endocrinol Diabetes Obes. 2011;18(2):144–7. https://doi.org/10.1097/MED.0b013e328344556e.
Grunfeld C, Kotler DP, Shigenaga JK, Doerrler W, Tierney A, Wang J, et al. Circulating interferon-alpha levels and hypertriglyceridemia in the acquired immunodeficiency syndrome. Am J Med. 1991;90(2):154–62.
Grunfeld C, Pang M, Doerrler W, Shigenaga JK, Jensen P, Feingold KR. Lipids, lipoproteins, triglyceride clearance, and cytokines in human immunodeficiency virus infection and the acquired immunodeficiency syndrome. J Clin Endocrinol Metab. 1992;74(5):1045–52. https://doi.org/10.1210/jcem.74.5.1373735.
Patel P, D’Amico R, Thiagarajah S, Wu S, Elliot E, Polli J et al. Weight and lipid changes in phase 3 cabotegravir and rilpivirine long-acting trials [abstract 505]. In: Conference on Retroviruses and Opportunistic Infections, Virtual. 2021.
Orkin C, DeJesus E, Sax PE, Arribas JR, Gupta SK, Martorell C, et al. Fixed-dose combination bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir-containing regimens for initial treatment of HIV-1 infection: week 144 results from two randomised, double-blind, multicentre, phase 3, non-inferiority trials. Lancet HIV. 2020;7(6):e389–400. https://doi.org/10.1016/S2352-3018(20)30099-0.
Aboud M, Kaplan R, Lombaard J, Zhang F, Hidalgo JA, Mamedova E, et al. Dolutegravir versus ritonavir-boosted lopinavir both with dual nucleoside reverse transcriptase inhibitor therapy in adults with HIV-1 infection in whom first-line therapy has failed (DAWNING): an open-label, non-inferiority, phase 3b trial. Lancet Infect Dis. 2019;19(3):253–64. https://doi.org/10.1016/S1473-3099(19)30036-2.
Orrell C, Hagins DP, Belonosova E, Porteiro N, Walmsley S, Falco V, et al. Fixed-dose combination dolutegravir, abacavir, and lamivudine versus ritonavir-boosted atazanavir plus tenofovir disoproxil fumarate and emtricitabine in previously untreated women with HIV-1 infection (ARIA): week 48 results from a randomised, open-label, non-inferiority, phase 3b study. Lancet HIV. 2017;4(12):e536–46. https://doi.org/10.1016/S2352-3018(17)30095-4.
Gotham D, Hill A, Pozniak AL. Candidates for inclusion in a universal antiretroviral regimen: tenofovir alafenamide. Curr Opin HIV AIDS. 2017;12(4):324–33. https://doi.org/10.1097/COH.0000000000000379.
Santos JR, Saumoy M, Curran A, Bravo I, Llibre JM, Navarro J, et al. The lipid-lowering effect of tenofovir/emtricitabine: a randomized, crossover, double-blind, placebo-controlled trial. Clin Infect Dis. 2015;61(3):403–8. https://doi.org/10.1093/cid/civ296.
Feingold KR, Grunfeld C. Effect of inflammation on HDL structure and function. Curr Opin Lipidol. 2016;27(5):521–30. https://doi.org/10.1097/MOL.0000000000000333.
Tall AR, Yvan-Charvet L. Cholesterol, inflammation and innate immunity. Nat Rev Immunol. 2015;15(2):104–16. https://doi.org/10.1038/nri3793.
McGillicuddy FC, de la Llera MM, Hinkle CC, Joshi MR, Chiquoine EH, Billheimer JT, et al. Inflammation impairs reverse cholesterol transport in vivo. Circulation. 2009;119(8):1135–45. https://doi.org/10.1161/CIRCULATIONAHA.108.810721.
Mujawar Z, Rose H, Morrow MP, Pushkarsky T, Dubrovsky L, Mukhamedova N, et al. Human immunodeficiency virus impairs reverse cholesterol transport from macrophages. PLoS Biol. 2006;4(11): e365. https://doi.org/10.1371/journal.pbio.0040365.
Riddle TM, Kuhel DG, Woollett LA, Fichtenbaum CJ, Hui DY. HIV protease inhibitor induces fatty acid and sterol biosynthesis in liver and adipose tissues due to the accumulation of activated sterol regulatory element-binding proteins in the nucleus. J Biol Chem. 2001;276(40):37514–9. https://doi.org/10.1074/jbc.M104557200.
Hwang YC, Fujimoto WY, Hayashi T, Kahn SE, Leonetti DL, Boyko EJ. Increased visceral adipose tissue is an independent predictor for future development of atherogenic dyslipidemia. J Clin Endocrinol Metab. 2016;101(2):678–85. https://doi.org/10.1210/jc.2015-3246.
Gan SK, Samaras K, Thompson CH, Kraegen EW, Carr A, Cooper DA, et al. Altered myocellular and abdominal fat partitioning predict disturbance in insulin action in HIV protease inhibitor-related lipodystrophy. Diabetes. 2002;51(11):3163–9. https://doi.org/10.2337/diabetes.51.11.3163.
Nielsen S, Guo Z, Johnson CM, Hensrud DD, Jensen MD. Splanchnic lipolysis in human obesity. J Clin Invest. 2004;113(11):1582–8. https://doi.org/10.1172/JCI21047.
Gwag T, Meng Z, Sui Y, Helsley RN, Park SH, Wang S, et al. Non-nucleoside reverse transcriptase inhibitor efavirenz activates PXR to induce hypercholesterolemia and hepatic steatosis. J Hepatol. 2019;70(5):930–40. https://doi.org/10.1016/j.jhep.2018.12.038.
Panza E, Wing EJ, Wing R. Behavioral Weight Loss: A promising treatment for obesity in adults with HIV. AIDS Behav. 2020;24(4):1085–91. https://doi.org/10.1007/s10461-019-02645-y.
Fitch KV, Anderson EJ, Hubbard JL, Carpenter SJ, Waddell WR, Caliendo AM, et al. Effects of a lifestyle modification program in HIV-infected patients with the metabolic syndrome. AIDS. 2006;20(14):1843–50. https://doi.org/10.1097/01.aids.0000244203.95758.db.
Lazzaretti RK, Kuhmmer R, Sprinz E, Polanczyk CA, Ribeiro JP. Dietary intervention prevents dyslipidemia associated with highly active antiretroviral therapy in human immunodeficiency virus type 1-infected individuals: a randomized trial. J Am Coll Cardiol. 2012;59(11):979–88. https://doi.org/10.1016/j.jacc.2011.11.038.
ACTG. Doravirine for persons with excessive weight gain on integrase inhibitors and tenofovir alafenamide (NCT04636437). ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT04636437. Accessed 1 Mar 2022.
Falutz J, Mamputu JC, Potvin D, Moyle G, Soulban G, Loughrey H, et al. Effects of tesamorelin (TH9507), a growth hormone-releasing factor analog, in human immunodeficiency virus-infected patients with excess abdominal fat: a pooled analysis of two multicenter, double-blind placebo-controlled phase 3 trials with safety extension data. J Clin Endocrinol Metab. 2010;95(9):4291–304. https://doi.org/10.1210/jc.2010-0490.
Thompson MA, Horberg MA, Agwu AL, Colasanti JA, Jain MK, Short WR, et al. Primary care guidance for persons with human immunodeficiency virus: 2020 Update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2021;73(11):e3572–605. https://doi.org/10.1093/cid/ciaa1391.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Supplement 1):S111-S24. https://doi.org/10.2337/dc21-S009.
Gervasoni C, Minisci D, Clementi E, Rizzardini G, Cattaneo D. How Relevant is the interaction between dolutegravir and metformin in real life? J Acquir Immune Defic Syndr. 2017;75(1):e24–6. https://doi.org/10.1097/QAI.0000000000001292.
Song IH, Zong J, Borland J, Jerva F, Wynne B, Zamek-Gliszczynski MJ, et al. The effect of dolutegravir on the pharmacokinetics of metformin in healthy subjects. J Acquir Immune Defic Syndr. 2016;72(4):400–7. https://doi.org/10.1097/QAI.0000000000000983.
Funding
Dr. Lo received funding from the National Institutes of Health and an investigator-initiated research grant from Viiv Healthcare for research and not for this review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Janet Lo has previously served as a consultant for Viiv Healthcare and on medical affairs advisory boards for Gilead Sciences. She is also a Co-Principal Investigator on an investigator-initiated research grant funded by Viiv Healthcare.
Caroline Diggins and Samuel Russo declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on HIV Pathogenesis and Treatment
Rights and permissions
About this article
Cite this article
Diggins, C.E., Russo, S.C. & Lo, J. Metabolic Consequences of Antiretroviral Therapy. Curr HIV/AIDS Rep 19, 141–153 (2022). https://doi.org/10.1007/s11904-022-00600-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-022-00600-6