Abstract
Purpose of Review
Patients with lower extremity peripheral artery disease (PAD) are at high risk for major adverse cardiovascular events (MACE) and major adverse limb events (MALE). This manuscript will review the current evidence for medical therapy in patients with PAD according to different clinical features and the overall cardiovascular (CV) risk.
Recent Findings
The management of PAD encompasses non-pharmacologic strategies, including lifestyle modification such as smoking cessation, supervised exercise, Mediterranean diet and weight loss as well as pharmacologic interventions, particularly for high risk patients. Benefits for reduction of CV and limb outcomes have been demonstrated for new therapies, including antithrombotic therapy (i.e., low-dose rivaroxaban plus aspirin), lipid lowering therapy (i.e., proprotein convertase subtilisin/kexin type 9 inhibitors), and glucose lowering therapy (i.e., sodium-glucose cotransporter-2 inhibitors and glucagon-like peptide-1 receptor agonists). However, the adoption of these therapies in PAD remains suboptimal in practice. Implementation science studies have recently shown promising results in PAD patients.
Summary
Comprehensive medical and non-medical management of PAD patients is crucial to improving patient outcomes, mitigating symptoms, and reducing the risk of MACE and MALE. A personalized approach, considering the patient's overall risk profile and preference, is essential for optimizing medical management of PAD.

Similar content being viewed by others
Data Availability
Data supporting the findings of the manuscript are available within the paper and its references.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Criqui MH, Matsushita K, Aboyans V, Hess CN, Hicks CW, Kwan TW, et al. Lower Extremity Peripheral Artery Disease: Contemporary Epidemiology, Management Gaps, and Future Directions: A Scientific Statement From the American Heart Association. Circulation. 2021;144(9). The paper provides updates on the epidemiology and current knowledge in PAD.
•• Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, et al. 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(12). The paper is the latest AHA/ACC LEPAD guidelines.
•• Aboyans V, Ricco JB, Bartelink MLEL, Björck M, Brodmann M, Cohnert T, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39(9):763–816. The paper is the latest ESC PAD guidelines.
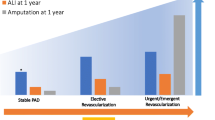
Hess CN, Huang Z, Patel MR, Baumgartner I, Berger JS, Blomster JI, et al. Acute Limb Ischemia in Peripheral Artery Disease. Circulation. 2019;140(7):556–65.
Kaplovitch E, Eikelboom JW, Dyal L, Aboyans V, Abola MT, Verhamme P, et al. Rivaroxaban and Aspirin in Patients With Symptomatic Lower Extremity Peripheral Artery Disease. JAMA Cardiol. 2020.
King RW, Canonico ME, Bonaca MP, Hess CN. Management of Peripheral Arterial Disease: Lifestyle Modifications and Medical Therapies. J Soc Cardiovasc Angiogr Interv. 2022;1(6):100513.
Berger JS, Abramson BL, Lopes RD, Heizer G, Rockhold FW, Baumgartner I, et al. Ticagrelor versus clopidogrel in patients with symptomatic peripheral artery disease and prior coronary artery disease: Insights from the EUCLID trial. Vasc Med. 2018;23(6):523–30.
•• Bonaca MP, Nault P, Giugliano RP, Keech AC, Pineda AL, Kanevsky E, et al. Low-Density Lipoprotein Cholesterol Lowering With Evolocumab and Outcomes in Patients With Peripheral Artery Disease. Circulation. 2018;137(4):338–50. The paper is a subgroup analysis from FOURIER demonstrating the efficacy of evolocumab in PAD patients.
• Narula N, Dannenberg AJ, Olin JW, Bhatt DL, Johnson KW, Nadkarni G, et al. Pathology of Peripheral Artery Disease in Patients With Critical Limb Ischemia. J Am Coll Cardiol. 2018;72(18):2152–63. The paper highlights the pathophysiology of ALI including the role of thrombo-embolism.
Creager MA, Hamburg NM. Smoking Cessation Improves Outcomes in Patients With Peripheral Artery Disease. JAMA Cardiol. 2022;7(1):15.
Ebbert J, Burke MV, Hays JT. Varenicline for smoking cessation: a narrative review of efficacy, adverse effects, use in at-risk populations, and adherence. Patient Prefer Adherence. 2016;435.
López-Laguna N, Martínez-González MA, Toledo E, Babio N, Sorlí JV, Ros E, et al. Risk of peripheral artery disease according to a healthy lifestyle score: The PREDIMED study. Atherosclerosis. 2018;275:133–40.
Treat-Jacobson D, McDermott MM, Beckman JA, Burt MA, Creager MA, Ehrman JK, et al. Implementation of Supervised Exercise Therapy for Patients With Symptomatic Peripheral Artery Disease: A Science Advisory From the American Heart Association. Circulation. 2019;140(13).
Fakhry F, Spronk S, van der Laan L, Wever JJ, Teijink JAW, Hoffmann WH, et al. Endovascular Revascularization and Supervised Exercise for Peripheral Artery Disease and Intermittent Claudication. JAMA. 2015;314(18):1936.
Belch J, MacCuish A, Campbell I, Cobbe S, Taylor R, Prescott R, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ. 2008;337:a1840–a1840.
Fowkes FGR, Price JF, Stewart MCW, Butcher I, Leng GC, Pell ACH, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010;303(9):841–8.
•• Aboyans V, Bauersachs R, Mazzolai L, Brodmann M, Palomares JFR, Debus S, et al. Antithrombotic therapies in aortic and peripheral arterial diseases in 2021: a consensus document from the ESC working group on aorta and peripheral vascular diseases, the ESC working group on thrombosis, and the ESC working group on cardiovascular pharmacotherapy. Eur Heart J. 2021;42(39):4013–24. The paper is the latest ESC consensus on antithrombotic therapy in PAD, including last evidence after LER.
CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee Lancet. 1996;348(9038):1329–39.
Canonico ME, Piccolo R, Avvedimento M, Leone A, Esposito S, Franzone A, et al. Antithrombotic Therapy in Peripheral Artery Disease: Current Evidence and Future Directions. J Cardiovasc Dev Dis. 2023;10(4):164.
Cacoub PP, Bhatt DL, Steg PG, Topol EJ, Creager MA. Patients with peripheral arterial disease in the CHARISMA trial. Eur Heart J. 2008;30(2):192–201.
Bonaca MP, Bhatt DL, Storey RF, Steg PhG, Cohen M, Kuder J, et al. Ticagrelor for Prevention of Ischemic Events After Myocardial Infarction in Patients With Peripheral Artery Disease. J Am Coll Cardiol. 2016;67(23):2719–28.
Steg PG, Bhatt DL, Simon T, Fox K, Mehta SR, Harrington RA, et al. Ticagrelor in Patients with Stable Coronary Disease and Diabetes. N Engl J Med. 2019;381(14):1309–20.
Warfarin Antiplatelet Vascular Evaluation Trial Investigators, Anand S, Yusuf S, Xie C, Pogue J, Eikelboom J, et al. Oral Anticoagulant and Antiplatelet Therapy and Peripheral Arterial Disease. N Eng J Med. 2007;357(3):217–27.
Bonaca MP, Scirica BM, Creager MA, Olin J, Bounameaux H, Dellborg M, et al. Vorapaxar in Patients With Peripheral Artery Disease. Circulation. 2013;127(14):1522–9.
Belch JJF, Dormandy J. Results of the randomized, placebo-controlled clopidogrel and acetylsalicylic acid in bypass surgery for peripheral arterial disease (CASPAR) trial. J Vasc Surg. 2010;52(4):825-833.e2.
Tepe G, Bantleon R, Brechtel K, Schmehl J, Zeller T, Claussen CD, et al. Management of peripheral arterial interventions with mono or dual antiplatelet therapy—the MIRROR study: a randomised and double-blinded clinical trial. Eur Radiol. 2012;22(9):1998–2006.
Efficacy of oral anticoagulants compared with aspirin after infrainguinal bypass surgery (The Dutch Bypass Oral anticoagulants or Aspirin study): a randomised trial. The Lancet. 2000;355(9201):346–51.
Moll F, Baumgartner I, Jaff M, Nwachuku C, Tangelder M, Ansel G, et al. Edoxaban Plus Aspirin vs Dual Antiplatelet Therapy in Endovascular Treatment of Patients With Peripheral Artery Disease: Results of the ePAD Trial. J Endovasc Ther. 2018;25(2):158–68.
•• Bonaca MP, Bauersachs RM, Anand SS, Debus ES, Nehler MR, Patel MR, et al. Rivaroxaban in Peripheral Artery Disease after Revascularization. N Engl J Med. 2020;382(21):1994–2004. The VOYAGER-PAD trial demonstrated the efficacy of DPI in symptomatic LEPAD patients undergoing LER.
Hiatt WR, Bonaca MP, Patel MR, Nehler MR, Debus ES, Anand SS, et al. Rivaroxaban and Aspirin in Peripheral Artery Disease Lower Extremity Revascularization. Circulation. 2020;142(23):2219–30.
Bauersachs RM, Szarek M, Brodmann M, Gudz I, Debus ES, Nehler MR, et al. Total Ischemic Event Reduction With Rivaroxaban After Peripheral Arterial Revascularization in the VOYAGER PAD Trial. J Am Coll Cardiol. 2021;78(4):317–26.
Östergren J. Impact of ramipril in patients with evidence of clinical or subclinical peripheral arterial disease. Eur Heart J. 2004;25(1):17–24.
Telmisartan R. or Both in Patients at High Risk for Vascular Events. N Engl J Med. 2008;358(15):1547–59.
Bavry AA, Anderson RD, Gong Y, Denardo SJ, Cooper-DeHoff RM, Handberg EM, et al. Outcomes Among Hypertensive Patients With Concomitant Peripheral and Coronary Artery Disease. Hypertension. 2010;55(1):48–53.
•• Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88. The paper is the latest ESC guidelines on dyslipidemia including LDL-C target in ASCVD patients.
MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebocontrolled trial. Lancet. 2002;360(9326):7–22.
Randomized trial of the effects of cholesterol-lowering with simvastatin on peripheral vascular and other major vascular outcomes in 20,536 people with peripheral arterial disease and other high-risk conditions. J Vasc Surg. 2007;45(4):645–654.e1.
Kumbhani DJ, Steg PhG, Cannon CP, Eagle KA, Smith SC, Goto S, et al. Statin therapy and long-term adverse limb outcomes in patients with peripheral artery disease: insights from the REACH registry. Eur Heart J. 2014;35(41):2864–72.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med. 2015;372(25):2387–97.
Bonaca MP, Gutierrez JA, Cannon C, Giugliano R, Blazing M, Park JG, et al. Polyvascular disease, type 2 diabetes, and long-term vascular risk: a secondary analysis of the IMPROVE-IT trial. Lancet Diabetes Endocrinol. 2018;6(12):934–43.
Lloyd-Jones DM, Morris PB, Ballantyne CM, Birtcher KK, Covington AM, DePalma SM, et al. 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk. J Am Coll Cardiol. 2022;80(14):1366–418.
•• Jukema JW, Szarek M, Zijlstra LE, de Silva HA, Bhatt DL, Bittner VA, et al. Alirocumab in Patients With Polyvascular Disease and Recent Acute Coronary Syndrome. J Am Coll Cardiol. 2019;74(9):1167–76. The paper is a subgroup analysis from ODYSSEY OUTCOMES demonstrating the efficacy of alirocumab in PAD patients.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome. N Engl J Med. 2018;379(22):2097–107.
Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med. 2019;380(1):11–22.
Niacin in Patients with Low HDL Cholesterol Levels Receiving Intensive Statin Therapy. N Engl J Med. 2011;365(24):2255–67.
•• Marx N, Federici M, Schütt K, Müller-Wieland D, Ajjan RA, Antunes MJ, et al. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J. 2023;44(39):4043–140. The paper is the latest ESC guidelines on CVD management in DM patients including the role of SGLT2i and GLP-1RA in ASCVD patients.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HAW. 10-Year Follow-up of Intensive Glucose Control in Type 2 Diabetes. N Engl J Med. 2008;359(15):1577–89.
Badjatiya A, Merrill P, Buse JB, Goodman SG, Katona B, Iqbal N, et al. Clinical Outcomes in Patients With Type 2 Diabetes Mellitus and Peripheral Artery Disease. Circ Cardiovasc Interv. 2019;12(12).
Verma S, Al-Omran M, Leiter LA, Mazer CD, Rasmussen S, Saevereid HA, et al. Cardiovascular efficacy of liraglutide and semaglutide in individuals with diabetes and peripheral artery disease. Diabetes Obes Metab. 2022;24(7):1288–99.
Dhatariya K, Bain SC, Buse JB, Simpson R, Tarnow L, Kaltoft MS, et al. The Impact of Liraglutide on Diabetes-Related Foot Ulceration and Associated Complications in Patients With Type 2 Diabetes at High Risk for Cardiovascular Events: Results From the LEADER Trial. Diabetes Care. 2018;41(10):2229–35.
• Sillesen H, Debus ES, Enggaard RBB, Frenkel O, Heled Y, Mansor-Lefebvre S, et al. Effects of semaglutide on functional capacity in patients with type 2 diabetes and peripheral arterial disease: rationale and design of the STRIDE trial. Eur Heart J. 2021;42(Supplement_1). This paper describes the design of the STRIDE trial investigating the role of GLP-1RA in PAD patients.
Verma S, Mazer CD, Al-Omran M, Inzucchi SE, Fitchett D, Hehnke U, et al. Cardiovascular Outcomes and Safety of Empagliflozin in Patients With Type 2 Diabetes Mellitus and Peripheral Artery Disease. Circulation. 2018;137(4):405–7.
Bonaca MP, Hamburg NM, Creager MA. Contemporary Medical Management of Peripheral Artery Disease. Circ Res. 2021;128(12):1868–84.
Barraclough JY, Yu J, Figtree GA, Perkovic V, Heerspink HJL, Neuen BL, et al. Cardiovascular and renal outcomes with canagliflozin in patients with peripheral arterial disease: Data from the <scp>CANVAS</scp> Program and <scp>CREDENCE</scp> trial. Diabetes Obes Metab. 2022;24(6):1072–83.
Bonaca MP, Wiviott SD, Zelniker TA, Mosenzon O, Bhatt DL, Leiter LA, et al. Dapagliflozin and Cardiac, Kidney, and Limb Outcomes in Patients With and Without Peripheral Artery Disease in DECLARE-TIMI 58. Circulation. 2020;142(8):734–47.
Dawson DL, Cutler BS, Hiatt WR, Hobson RW, Martin JD, Bortey EB, et al. A comparison of cilostazol and pentoxifylline for treating intermittent claudication. Am J Med. 2000;109(7):523–30.
McDermott MM, Criqui MH, Domanchuk K, Ferrucci L, Guralnik JM, Kibbe MR, et al. Cocoa to Improve Walking Performance in Older People With Peripheral Artery Disease. Circ Res. 2020;126(5):589–99.
Canonico ME, Hsia J, Hess CN, Bonaca MP. Sex differences in guideline-directed medical therapy in 2021–22 among patients with peripheral artery disease. Vasc Med. 2023;1358863X2311553.
Hess CN, Cannon CP, Beckman JA, Goodney PP, Patel MR, Hiatt WR, et al. Effectiveness of Blood Lipid Management in Patients With Peripheral Artery Disease. J Am Coll Cardiol. 2021;77(24):3016–27.
Sonderman M, Aday AW, Farber-Eger E, Mai Q, Freiberg MS, Liebovitz DM, et al. Identifying Patients With Peripheral Artery Disease Using the Electronic Health Record. JACC: Advances. 2023;2(7):100566.
• Hess CN, Nehler M, Daffron A, Morrison J, Buchanan C, Saseen JJ, et al. PRAGMATIC IMPLEMENTATION SCIENCE TO ASSESS LIPID OPTIMIZATION IN PERIPHERAL ARTERY DISEASE: PRIMARY RESULTS OF THE OPTIMIZE PAD-1 TRIAL. J Am Coll Cardiol. 2023;81(8):2105. This abstract includes the preliminary results of the OPTIMIZE PAD-1 trial, an implementation science study of lipid management in PAD patients.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
MEC and CNH wrote the main manuscript text and RKR and MPH critically reviewed the content. All authors approved the final version.
Corresponding author
Ethics declarations
Conflict of Interest
Drs Canonico, Hess, Rogers, Bonaca receive salary support from CPC, a non-profit academic research organization affiliated with the University of Colorado, that receives or has received research grant/consulting funding between July 2021 and July 2023 from the following organizations: Abbot Laboratories, Agios Pharmaceuticals, Inc., Alexion Pharma Godo Kaisha, Amgen Inc., Anthos Therapeutics, Inc., ARCA biopharma, Inc., AstraZeneca Pharma India, AstraZeneca Pharmaceuticals LP, AstraZeneca UK Ltd, AstraZeneca, Produtos Farmaceuticos, Lda, Atentiv, LLC, Bayer, Bayer (Proprietary) Limited, Bayer Aktiengesellschaft, Bayer Pharma AG, Beth Israel Deaconess Medical Center, Better Therapeutics, Boston Clinical Research Institute, LLC, Bristol-Myers Squibb, CellResearch Corporation Pte Ltd, Cleerly, Inc., Colorado Dept of Public Health and Environment, Cook Regentec LLC, CSL Behring LLC, Eidos Therapeutics, Inc., EPG Communication Holdings Ltd., Esperion Therapeutics, Inc, Faraday Pharmaceuticals, Inc., HeartFlow Inc, Insmed, Ionis Pharmaceuticals, IQVIA Inc., Janssen Pharmaceuticals, Inc, Janssen Research & Development, LLC, Janssen Scientific Affairs LLC, Lexicon Pharmaceuticals, Inc., LSG Corporation, MedImmune Limited, Medpace, Inc., Medscape, Merck Sharp & Dohme Corp., Nectero Medical Inc., Novartis Pharmaceuticals Corporation, Novo Nordisk, Osiris Therapeutics, Inc., Pfizer, PPD Development, L.P., Prothena Biosciences Limited, Regeneron, Regents of the University of Colorado (aka UCD), Sanifit Therapeutics S.A., Sanofi, Silence Therapeutics PLC, Stanford University, Stealth BioTherapeutics Inc., The Brigham & Women's Hospital, Inc., Thrombosis Research Institute, University of Colorado Denver, University of Pittsburgh, VarmX, WraSer, LLC. Dr. Bonaca receives support from the AHA SFRN under award numbers 18SFRN3390085 (BWH-DH SFRN Center) and 18SFRN33960262 (BWH-DH Clinical Project). Dr. Bonaca also reports stock in Medtronic and Pfizer.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclosures
Drs Canonico, Hess, Rogers, Bonaca receive salary support from CPC, a non-profit academic research organization affiliated with the University of Colorado, that receives or has received research grant/consulting funding between July 2021 and July 2023 from the following organizations: Abbot Laboratories, Agios Pharmaceuticals, Inc., Alexion Pharma Godo Kaisha, Amgen Inc., Anthos Therapeutics, Inc., ARCA biopharma, Inc., AstraZeneca Pharma India, AstraZeneca Pharmaceuticals LP, AstraZeneca UK Ltd, AstraZeneca, Produtos Farmaceuticos, Lda, Atentiv, LLC, Bayer, Bayer (Proprietary) Limited, Bayer Aktiengesellschaft, Bayer Pharma AG, Beth Israel Deaconess Medical Center, Better Therapeutics, Boston Clinical Research Institute, LLC, Bristol-Myers Squibb, CellResearch Corporation Pte Ltd, Cleerly, Inc., Colorado Dept of Public Health and Environment, Cook Regentec LLC, CSL Behring LLC, Eidos Therapeutics, Inc., EPG Communication Holdings Ltd., Esperion Therapeutics, Inc, Faraday Pharmaceuticals, Inc., HeartFlow Inc, Insmed, Ionis Pharmaceuticals, IQVIA Inc., Janssen Pharmaceuticals, Inc, Janssen Research & Development, LLC, Janssen Scientific Affairs LLC, Lexicon Pharmaceuticals, Inc., LSG Corporation, MedImmune Limited, Medpace, Inc., Medscape, Merck Sharp & Dohme Corp., Nectero Medical Inc., Novartis Pharmaceuticals Corporation, Novo Nordisk, Osiris Therapeutics, Inc., Pfizer, PPD Development, L.P., Prothena Biosciences Limited, Regeneron, Regents of the University of Colorado (aka UCD), Sanifit Therapeutics S.A., Sanofi, Silence Therapeutics PLC, Stanford University, Stealth BioTherapeutics Inc., The Brigham & Women's Hospital, Inc., Thrombosis Research Institute, University of Colorado Denver, University of Pittsburgh, VarmX, WraSer, LLC. Dr. Bonaca receives support from the AHA SFRN under award numbers 18SFRN3390085 (BWH-DH SFRN Center) and 18SFRN33960262 (BWH-DH Clinical Project). Dr. Bonaca also reports stock in Medtronic and Pfizer.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Canonico, M.E., Hess, C.N., Rogers, R.K. et al. Medical Therapy for Peripheral Artery Disease. Curr Cardiol Rep (2024). https://doi.org/10.1007/s11886-024-02065-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s11886-024-02065-y