Abstract
Purpose of Review
This review intends to give an up-to-date overview of the current state of evidence in the treatment of coronary artery disease (CAD) in patients undergoing transcatheter aortic valve replacement (TAVR), focusing on percutaneous coronary interventions (PCI) pre-TAVR.
Recent Findings
The recently published ACTIVATION trial is the 1st randomized trial comparing coronary revascularization (PCI) versus medical treatment in patients with significant CAD undergoing TAVR. With the caveat of several major limitations of the trial, the results of this study raised the question about the appropriateness of the common practice to routinely revascularize coronary stenosis before TAVR.
Summary
Aortic valve stenosis is the most common valvular heart disease among the elderly and it often co-occurs with CAD. TAVR is increasingly considered an alternative to surgical aortic valve replacement not only in the elderly population but also in younger and lower-risk patients. The impact of co-existing CAD on clinical outcomes as well as the optimal timing of PCI in TAVR candidates is still unclear and the subject of ongoing randomized trials. Meanwhile, it is common practice in many centers to routinely perform invasive coronary angiography and PCI for significant coronary disease as part of the TAVR workup. While computed tomography angiography has emerged as a possible alternative to the invasive coronary angiography in patients with low pre-test probability for CAD, the value of functional invasive assessment of coronary lesions in the pre-TAVR setting has still to be clarified. Also, there is an increasing interest in the clinical relevance and optimal management of the potentially challenging coronary access post-TAVR, requiring further research.



Similar content being viewed by others
Abbreviations
- ACS:
-
Acute coronary syndrome
- CABG:
-
Coronary artery bypass grafting
- CAD:
-
Coronary artery disease
- CCS:
-
Canadian cardiovascular society
- cCT:
-
Coronary computed tomography
- CTA:
-
Computed tomography angiography
- FFR:
-
Fractional flow reserve
- iFR:
-
Instantaneous wave-free ratio
- LAD:
-
Left anterior descending artery
- NSTEMI:
-
Non-ST-elevation myocardial infarction
- MACCE:
-
Major adverse cardiac and cerebrovascular events
- PCI:
-
Percutaneous coronary intervention
- rSS:
-
Residual Syntax Score
- SAVR:
-
Surgical aortic valve replacement
- STEMI:
-
ST-elevation myocardial infarction
- SYNTAX:
-
Synergy Between PCI With Taxus and Cardiac Surgery
- TAVR:
-
Transcatheter aortic valve replacement
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study, (in eng). Lancet. 2006;368(9540):1005–11. https://doi.org/10.1016/S0140-6736(06)69208-8.
Leon MB, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery, (in eng). N Engl J Med. 2010;363(17):1597–607. https://doi.org/10.1056/NEJMoa1008232.
Popma JJ, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients, (in eng). N Engl J Med 2019;380(180:1706–1715. https://doi.org/10.1056/NEJMoa1816885.
Smith CR, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients, (in eng). N Engl J Med. 2011;364(23):2187–98. https://doi.org/10.1056/NEJMoa1103510.
Mack MJ, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients, (in eng). N Engl J Med 2019;380(18):1695–1705. https://doi.org/10.1056/NEJMoa1814052.
Vahanian A, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease, (in eng). Eur Heart J. 2021;08:28. https://doi.org/10.1093/eurheartj/ehab395.
Otto CM, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the american college of cardiology/american heart association joint committee on clinical practice guidelines, (in eng). J Am Coll Cardiol. 2021;77(4):450–500. https://doi.org/10.1016/j.jacc.2020.11.035.
Paradis JM, et al. Impact of coronary artery disease severity assessed with the SYNTAX score on outcomes following transcatheter aortic valve replacement. J Am Heart Assoc. 2017;6(2):02–20. https://doi.org/10.1161/JAHA.116.005070.
Stefanini GG, et al. Coronary artery disease severity and aortic stenosis: clinical outcomes according to SYNTAX score in patients undergoing transcatheter aortic valve implantation, (in eng). Eur Heart J. 2014;35(37):2530–40. https://doi.org/10.1093/eurheartj/ehu074.
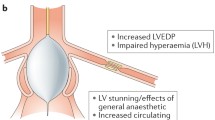
Di Gioia G, et al. Pathophysiology, diagnosis, and treatment of patients with concomitant severe aortic stenosis and coronary artery disease: a closer look to the unresolved perplexity. J Clin Med. 2021;10(8). https://doi.org/10.3390/jcm10081617.
Pepe M, et al. Degenerative severe aortic stenosis and concomitant coronary artery disease: what is changing in the era of the transcatheter revolution? Curr Atheroscler Rep 2020;22(5):17. https://doi.org/10.1007/s11883-020-0835-1.
Linke A, et al. Treatment of aortic stenosis with a self-expanding transcatheter valve: the International Multi-centre ADVANCE Study, (in eng). Eur Heart J. 2014;35(38):2672–84. https://doi.org/10.1093/eurheartj/ehu162.
Adams DH, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis, (in eng). N Engl J Med. 2014;370(19):1790–8. https://doi.org/10.1056/NEJMoa1400590.
Hamm CW, et al. The German Aortic Valve Registry (GARY): in-hospital outcome, (in eng). Eur Heart J. 2014;35(24):1588–98. https://doi.org/10.1093/eurheartj/eht381.
Leon MB, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med 2016;374(17):1609–20. https://doi.org/10.1056/NEJMoa1514616.
Wendler O, et al. SOURCE 3 registry: design and 30-day results of the European postapproval registry of the latest generation of the SAPIEN 3 transcatheter heart valve, (in eng). Circulation. 2017;135(12):1123–32. https://doi.org/10.1161/CIRCULATIONAHA.116.025103.
Reardon MJ, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376(14):1321–1331. https://doi.org/10.1056/NEJMoa1700456.
Kotronias RA, et al. Transcatheter aortic valve implantation with or without percutaneous coronary artery revascularization strategy: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6(6). https://doi.org/10.1161/JAHA.117.005960.
D’Ascenzo F, et al. Independent impact of extent of coronary artery disease and percutaneous revascularisation on 30-day and one-year mortality after TAVI: a meta-analysis of adjusted observational results, (in eng). EuroIntervention. 2018;14(11):e1169–77. https://doi.org/10.4244/EIJ-D-18-00098.
Sankaramangalam K, et al. Impact of coronary artery disease on 30-day and 1-year mortality in patients undergoing transcatheter aortic valve replacement: a meta-analysis. J Am Heart Assoc. 2017;6(10). https://doi.org/10.1161/JAHA.117.006092.
D’Ascenzo F, et al. Mid-term prognostic value of coronary artery disease in patients undergoing transcatheter aortic valve implantation: a meta-analysis of adjusted observational results, (in eng). Int J Cardiol. 2013;168(3):2528–32. https://doi.org/10.1016/j.ijcard.2013.03.062.
Weferling M, Hamm CW, Kim WK. Percutaneous coronary intervention in transcatheter aortic valve implantation patients: overview and practical management, (in eng). Front Cardiovasc Med. 2021;8: 653768. https://doi.org/10.3389/fcvm.2021.653768.
Witberg G, et al. The Prognostic effects of coronary disease severity and completeness of revascularization on mortality in patients undergoing transcatheter aortic valve replacement. JACC Cardiovasc Interv 2017;10(14):1428–1435. https://doi.org/10.1016/j.jcin.2017.04.035.
Pontone G, et al. Feasibility and accuracy of a comprehensive multidetector computed tomography acquisition for patients referred for balloon-expandable transcatheter aortic valve implantation, (in eng). Am Heart J. 2011;161(6):1106–13. https://doi.org/10.1016/j.ahj.2011.03.003.
Andreini D, et al. Diagnostic accuracy of multidetector computed tomography coronary angiography in 325 consecutive patients referred for transcatheter aortic valve replacement, (in eng). Am Heart J. 2014;168(3):332–9. https://doi.org/10.1016/j.ahj.2014.04.022.
Hamdan A, et al. Coronary CT angiography for the detection of coronary artery stenosis in patients referred for transcatheter aortic valve replacement. J Cardiovasc Comput Tomogr. 2015;9(1):31–41. https://doi.org/10.1016/j.jcct.2014.11.008.
Harris BS, et al. Dual-source CT imaging to plan transcatheter aortic valve replacement: accuracy for diagnosis of obstructive coronary artery disease, (in eng). Radiology. 2015;275(1):80–8. https://doi.org/10.1148/radiol.14140763.
Opolski MP, et al. Diagnostic accuracy of computed tomography angiography for the detection of coronary artery disease in patients referred for transcatheter aortic valve implantation, (in eng). Clin Res Cardiol. 2015;104(6):471–80. https://doi.org/10.1007/s00392-014-0806-z.
Matsumoto S, et al. CT imaging before transcatheter aortic valve implantation (TAVI) using variable helical pitch scanning and its diagnostic performance for coronary artery disease, (in eng). Eur Radiol. 2017;27(5):1963–70. https://doi.org/10.1007/s00330-016-4547-4.
Strong C, et al. Diagnostic accuracy of computed tomography angiography for the exclusion of coronary artery disease in candidates for transcatheter aortic valve implantation. Sci Rep. 2019;9(1):19942. https://doi.org/10.1038/s41598-019-56519-3.
Meier D, et al. Computed tomography angiography for the diagnosis of coronary artery disease among patients undergoing transcatheter aortic valve implantation. J Cardiovasc Transl Res. 2021;14(5):894–901. https://doi.org/10.1007/s12265-021-10099-8.
Chieffo A, et al. Routine screening of coronary artery disease with computed tomographic coronary angiography in place of invasive coronary angiography in patients undergoing transcatheter aortic valve replacement, (in eng). Circ Cardiovasc Interv. 2015;8(7): e002025. https://doi.org/10.1161/CIRCINTERVENTIONS.114.002025.
van den Boogert TPW, et al. CTCA for detection of significant coronary artery disease in routine TAVI work-up : a systematic review and meta-analysis, (in eng). Neth Heart J. 2018;26(12):591–9. https://doi.org/10.1007/s12471-018-1149-6.
Fihn SD, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons, (in eng). J Am Coll Cardiol. 2014;64(18):1929–49. https://doi.org/10.1016/j.jacc.2014.07.017.
Neumann FJ, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165. https://doi.org/10.1093/eurheartj/ehy394.
Lunardi M, et al. Physiological versus angiographic guidance for myocardial revascularization in patients undergoing transcatheter aortic valve implantation. J Am Heart Assoc. 2019;8(22):e012618. https://doi.org/10.1161/JAHA.119.012618.
Stanojevic D, et al. Intravenous adenosine infusion is safe and well tolerated during coronary fractional flow reserve assessment in elderly patients with severe aortic stenosis, (in eng). J Invasive Cardiol. 2016;28(9):357–61.
Pesarini G, et al. Functional assessment of coronary artery disease in patients undergoing transcatheter aortic valve implantation: influence of pressure overload on the evaluation of lesions severity, (in eng). Circ Cardiovasc Interv. 2016;9(11):11. https://doi.org/10.1161/CIRCINTERVENTIONS.116.004088.
Scarsini R, et al. Observations from a real-time, iFR-FFR hybrid approach in patients with severe aortic stenosis and coronary artery disease undergoing TAVI," (in eng), Cardiovasc Revasc Med. 2018;19(3 Pt B):355–359. https://doi.org/10.1016/j.carrev.2017.09.019.
Ahmad Y, et al. Coronary hemodynamics in patients with severe aortic stenosis and coronary artery disease undergoing transcatheter aortic valve replacement: implications for clinical indices of coronary stenosis severity. JACC Cardiovasc Interv. 2018;11(20):2019–2031. https://doi.org/10.1016/j.jcin.2018.07.019.
Decision memo for transcatheter aortic valve replacement (TAVR) (CAG- 00430N). https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=257. (Accessed 14 Nov 2016)
Wendt D, et al. Management of high-risk patients with aortic stenosis and coronary artery disease, (in eng). Ann Thorac Surg. 2013;95(2):599–605. https://doi.org/10.1016/j.athoracsur.2012.07.075.
Alperi A, et al. Transcatheter versus surgical aortic valve replacement in patients with complex coronary artery disease, (in eng). JACC Cardiovasc Interv. 2021;14(22):2490–9. https://doi.org/10.1016/j.jcin.2021.08.073.
Faroux L, et al. Coronary artery disease and transcatheter aortic valve replacement: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74(3):362–372. https://doi.org/10.1016/j.jacc.2019.06.012.
Lateef N, et al. Meta-analysis comparing outcomes in patients undergoing transcatheter aortic valve implantation with versus without percutaneous coronary intervention. Am J Cardiol. 2019;124(11):1757–1764. https://doi.org/10.1016/j.amjcard.2019.08.024.
•• Patterson T, et al. ACTIVATION (PercutAneous Coronary inTervention prIor to transcatheter aortic VAlve implantaTION): a randomized clinical trial, (in eng), JACC Cardiovasc Interv. 2021;14(18):1965–1974. https://doi.org/10.1016/j.jcin.2021.06.041. ACTIVATION is the 1st randomized trial comparing coronary revascularization (PCI) versus medical treatment in patients with significant CAD undergoing TAVR.
Chakravarty T, et al. Outcomes in patients with transcatheter aortic valve replacement and left main stenting: the TAVR-LM registry, (in eng). J Am Coll Cardiol. 2016;67(8):951–60. https://doi.org/10.1016/j.jacc.2015.10.103.
• Faroux L, et al. Procedural characteristics and late outcomes of percutaneous coronary intervention in the workup pre-TAVR. JACC Cardiovasc Interv. 2020;13(22):2601–2613. https://doi.org/10.1016/j.jcin.2020.07.009. This study showed that pre-TAVR PCI is feasible and safe, even in multivessel disease, left main disease and calcified lesions.
Allende R, et al. Advanced chronic kidney disease in patients undergoing transcatheter aortic valve implantation: insights on clinical outcomes and prognostic markers from a large cohort of patients, (in eng). Eur Heart J. 2014;35(38):2685–96. https://doi.org/10.1093/eurheartj/ehu175.
van Rosendael PJ, et al. Timing of staged percutaneous coronary intervention before transcatheter aortic valve implantation, (in eng). Am J Cardiol. 2015;115(12):1726–32. https://doi.org/10.1016/j.amjcard.2015.03.019.
Yang Y, et al. The safety of concomitant transcatheter aortic valve replacement and percutaneous coronary intervention: a systematic review and meta-analysis, (in eng). Medicine (Baltimore). 2017;96(48): e8919. https://doi.org/10.1097/MD.0000000000008919.
Vilalta V, et al. Incidence, clinical characteristics, and impact of acute coronary syndrome following transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2018;11(24):2523–2533. https://doi.org/10.1016/j.jcin.2018.09.001.
Blumenstein J, et al. Challenges of coronary angiography and intervention in patients previously treated by TAVI, (in eng). Clin Res Cardiol. 2015;104(8):632–9. https://doi.org/10.1007/s00392-015-0824-5.
Yudi MB, Sharma SK, Tang GHL, Kini A. Coronary angiography and percutaneous coronary intervention after transcatheter aortic valve replacement. J Am Coll Cardiol. 2018;71(12):1360–78. https://doi.org/10.1016/j.jacc.2018.01.057.
Faroux L, et al. ST-segment elevation myocardial infarction following transcatheter aortic valve replacement. J Am Coll Cardiol. 2021;77(17):2187–99. https://doi.org/10.1016/j.jacc.2021.03.014.
Tang GHL, et al. Alignment of transcatheter aortic-valve neo-commissures (ALIGN TAVR): impact on final valve orientation and coronary artery overlap. JACC Cardiovasc Interv. 2020;13(9):1030–1042. https://doi.org/10.1016/j.jcin.2020.02.005.
Walther T, et al. Perioperative results and complications in 15,964 transcatheter aortic valve replacements: prospective data from the GARY registry, (in eng). J Am Coll Cardiol. 2015;65(20):2173–80. https://doi.org/10.1016/j.jacc.2015.03.034.
Acknowledgements
Dr. Rodés-Cabau holds the Research Chair “Fondation Famille Jacques Larivière” for the Development of Structural Heart Interventions. Dr. Keller has received a research grant from “KK Stiftung für Kardiologie und Kreislauf” (Switzerland). Dr. Panagides has received a research grant from the “Mediterranean Academic Research and Studies in Cardiology Association” (MARS Cardio). Dr. Mesnier reports a research grant from “Federation Française de Cardiologie”. Dr. Nuche has received a research grant from the “Fundación Alfonso Martín Escudero” (Madrid, Spain).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
Dr. Rodés-Cabau has received institutional research grants and speaker fees from Edwards Lifesciences and Medtronic. Dr. Panagides has received institutional research grants from Medtronic, Boston scientific and Microport.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Valvular Heart Disease
Rights and permissions
About this article
Cite this article
Keller, L.S., Panagides, V., Mesnier, J. et al. Percutaneous Coronary Intervention Pre-TAVR: Current State of the Evidence. Curr Cardiol Rep 24, 1011–1020 (2022). https://doi.org/10.1007/s11886-022-01717-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01717-1