Abstract
Purpose
In spite of widespread recommendations for lifelong patient follow-up with a bariatric provider after bariatric surgery, attrition to follow-up is common. Over the past two decades, many programs have sought to expand access to care for patients lacking insurance coverage for bariatric surgery by offering “self-pay” packages; however, the impact of this financing on long-term follow-up is unclear. We sought to determine whether payer status impacts loss to follow-up within 1 year after bariatric surgery.
Materials and Methods
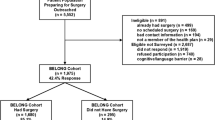
Records of 554 consecutive patients undergoing bariatric surgery who were eligible for 1-year post-surgical follow-up between 2014 and 2019 were retrospectively reviewed. Multiple logistic regression examined the relationship between demographics, psychological variables, payer status, and loss to follow-up.
Results
Self-pay status more than tripled the odds of loss to follow-up (OR = 3.44, p < 0.01) at 1 year following surgery. Males had more than double the odds of attrition (OR = 2.43, p < 0.01), and members of racial and ethnic minority groups (OR = 2.51, p < 0.05) were more likely to experience loss.
Conclusions
Self-pay patients, males and members of racial and ethnic minority groups, may face additional barriers to long-term access to postoperative bariatric care. Further investigation is greatly needed to develop strategies to overcome barriers to and disparities in long-term post-surgical care for more frequently lost groups.

Similar content being viewed by others
References
Harper J, Madan AK, Ternovits CA, et al. What happens to patients who do not follow-up after bariatric surgery? Am Surg. 2007;73(2):181–4.
Grossi E, Dalle Grave R, Mannucci E, et al. Complexity of attrition in the treatment of obesity: clues from a structured telephone interview. Int J Obes. 2002;30(7):1132.
Moroshko I, Brennan L, O’Brien P. Predictors of attrition in bariatric aftercare: a systematic review of the literature. Obes Surg. 2012;22(10):1640–7.
Sockalingam S, Cassin S, Hawa R, et al. Predictors of post-bariatric surgery appointment attendance: the role of relationship style. Obes Surg. 2013;23(12):2026–32.
Shen R, Dugay G, Rajaram K, et al. Impact of patient follow-up on weight loss after bariatric surgery. Obes Surg. 2004;14(4):514–9.
O'Brien PE, MacDonald L, Anderson M, et al. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257(1):87–94.
Higa K, Ho T, Tercero F, et al. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis. 2011;7(4):516–25.
Wheeler E, Prettyman A, Lenhard MJ, et al. Adherence to outpatient program postoperative appointments after bariatric surgery. Surg Obes Relat Dis. 2008;4(4):515–20.
Kolotkin RL, Crosby RD. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-lite) in a community sample. Qual Life Res. 2002;11(2):157–71.
Moos RH. Coping responses inventory: an update on research applications and validity. Odessa: Psychological Assessment Resources; 2004.
Parkerson Jr GR, Broadhead WE, Tse CK. Validation of the Duke Social Support and Stress Scale. Fam Med. 1991;23(5):357–60.
Sarason I, Sarason BR, Shearin EN, et al. A brief measure of social support: practical and theoretical implications. J Soc Pers Relat. 1987;
Spaniolas K, Kasten KR, Celio A, et al. Postoperative follow-up after bariatric surgery: effect on weight loss. Obes Surg. 2016;26(4):900–3.
Welbourn R, Pournaras D. Bariatric surgery: a cost-effective intervention for morbid obesity; functional and nutritional outcomes. Proc Nutr Soc. 2010;69(4):528–35.
Crémieux PY, Buchwald H, Shikora SA. A study on the economic impact of bariatric surgery. Am J Manag Care. 2008;14(9):589–96.
Powers KA, Rehrig ST, Jones DB. Financial impact of obesity and bariatric surgery. Med Clin N Am. 2007;91(3):321–38.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55.
Goode RW, Ye L, Sereika SM, et al. Socio-demographic, anthropometric, and psychosocial predictors of attrition across behavioral weight-loss trials. Eat Behav. 2016;20:27–33.
Ard JD, Emery M, Cook M, et al. Skin in the game: does paying for obesity treatment out of pocket lead to better outcomes compared to insurance coverage? Obesity. 2017;25(6):993–6.
Piette JD, Wagner TH, Potter MB, et al. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care. 2004;42(2):102–9. www.jstor.org/stable/4640706. Accessed 5 July 2020
Boddiger D. Lack of insurance hinders Americans’ diabetes care. Lancet. 2006;368(9529):15–6.
Hayes S, Napolitano MA, Lent MR, et al. The effect of insurance status on pre- and post-operative bariatric surgery outcomes. Obes Surg. 2015;25:191–4.
Takemoto E, Wolfe BM, Nagel CL, et al. Insurance status differences in weight loss and regain over 5 years following bariatric surgery. Int J Obes. 2018;42:1211–20.
Acknowledgments
The authors wish to acknowledge our patients and their families, from whom we are continually learning, and all those who advocate for and provide quality care to patients with obesity.
Funding
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs. Ibele, McGarrity, Volckmann, and Morrow and Ms. Kohler, Martinez, and Turner have no active or potential personal business or financial conflicts of interest related to the enclosed research. Ms. Martinez previously served part time as site coordinator for a clinical trial conducted by the Rhythm Pharmaceuticals which was unrelated to the content of this work.
Ethics and Consent
Institutional Review Board approval was obtained prior to the conduct of this research. As this was a retrospective study, informed consent for research participation was deemed exempt by our Institutional Review Board. This work has not been previously published, and consent to submit has been received from all co-authors and responsible authorities at the institution where this work has been carried out. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martinez, P.L., McGarrity, L.A., Turner, N.A. et al. Self-Pay Payer Status Predicts Long-Term Loss to Follow-Up After Bariatric Surgery. OBES SURG 31, 1590–1596 (2021). https://doi.org/10.1007/s11695-020-05161-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05161-4