Abstract
Purpose
Effective postoperative analgesia is paramount in patients undergoing bariatric surgery, given their increased predisposition to narcotic-induced respiratory depression. Transversus abdominis plane (TAP) block has shown promise in the enhanced recovery pathway for several abdominal procedures. We performed a systematic review and meta-analysis to compare the effectiveness of TAP block in laparoscopic bariatric surgery.
Materials and Methods
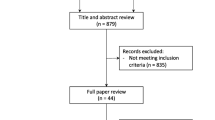
PubMed, EMBASE and Cochrane databases were searched for relevant articles from inception until June 2020. All randomized trials that compared TAP blocks versus none in laparoscopic bariatric procedures were included. The primary outcome was narcotic consumption at 24 h postoperatively, whilst secondary outcomes included postoperative pain scores at 24 h, time to ambulation, postoperative nausea and vomiting (PONV) and complication rates. Random effects models were used to calculate pooled effect size estimates.
Results
Seven randomized controlled trials were included, capturing 617 patients. There was high statistical heterogeneity across studies. On random effects analysis, there were no significant differences in narcotic consumption (MD −12.63 mg, 95% CI = −31.67 to 6.41, p = 0.19), pain scores (MD −0.71, 95% CI = −1.93 to 0.50, p = 0.25) or complications (RD = −0.00, 95% CI = −0.03 to 0.03, p = 0.87) between TAP and no TAP groups. However, TAP was associated with significantly less time to ambulation (MD −2.22 h, 95% CI = −3.89 to −0.56, p = 0.009) and PONV (OR = 0.13, 95% CI = 0.05 to 0.35, p < 0.0001).
Conclusions
TAP in laparoscopic bariatric surgery is associated with significantly less PONV and time to ambulation, but similar complication rates, narcotic usage and postoperative pain at 24 h compared to no TAP.







Similar content being viewed by others
References
Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33(7):673–89.
Booth HP, Khan O, Fildes A, et al. Changing epidemiology of bariatric surgery in the UK: cohort study using primary care electronic health records. Obes Surg. 2016;26(8):1900–5.
Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56(10):1024–6.
McDonnell JG, O'Donnell B, Curley G, et al. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104(1):193–7.
Milan Z, Tabor D, McConnell P, et al. Three different approaches to Transversus abdominis planeblock: a cadaveric study. Med Glas (Zenica). 2011;8(2):181–4.
Zaghiyan KN, Mendelson BJ, Eng MR, et al. Randomized clinical trial comparing laparoscopic versus ultrasound-guided transversus abdominis plane block in minimally invasive colorectal surgery. Dis Colon Rectum. 2019;62(2):203–10.
Niraj G, Searle A, Mathews M, et al. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br J Anaesth. 2009;103(4):601–5.
El-Dawlatly AA, Turkistani A, Kettner SC, et al. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102(6):763–7.
Ra YS, Kim CH, Lee GY, et al. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. 2010;58(4):362–8.
Niraj G, Kelkar A, Jeyapalan I, et al. Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia. 2011;66(6):465–71.
Belavy D, Cowlishaw PJ, Howes M, et al. Ultrasound-guided transversus abdominis plane block for analgesia after caesarean delivery. Br J Anaesth. 2009;103(5):726–30.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10.
DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45(Pt A):139–45.
Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Albrecht E, Kirkham KR, Endersby RV, et al. Ultrasound-guided transversus abdominis plane (TAP) block for laparoscopic gastric-bypass surgery: a prospective randomized controlled double-blinded trial. Obes Surg. 2013;23(8):1309–14.
Ruiz-Tovar J, Garcia A, Ferrigni C, et al. Laparoscopic-guided transversus abdominis plane (TAP) block as part of multimodal analgesia in laparoscopic Roux-en-Y gastric bypass within an enhanced recovery after surgery (ERAS) program: a prospective randomized clinical trial. Obes Surg. 2018;28(11):3374–9.
Said AM, Balamoun HA. Continuous transversus abdominis plane blocks via laparoscopically placed catheters for bariatric surgery. Obes Surg. 2017;27(10):2575–82.
Ari DE, Ar AY, Karip CS, et al. Ultrasound-guided subcostal-posterior transversus abdominis plane block for pain control following laparoscopic sleeve gastrectomy. Saudi Med J. 2017;38(12):1224–9.
Gupta C, Valecha UK, Singh SP, et al. Systemic lidocaine versus ultrasound-guided transversus abdominis plane block for postoperative analgesia: a comparative randomised study in bariatric surgical patients. Indian J Anaesth. 2020;64(1):31–6.
Ruiz-Tovar J, Gonzalez G, Sarmiento A, et al. Analgesic effect of postoperative laparoscopic-guided transversus abdominis plane (TAP) block, associated with preoperative port-site infiltration, within an enhanced recovery after surgery protocol in one-anastomosis gastric bypass: a randomized clinical trial. Surg Endosc. 2020;
Mittal T, Dey A, Siddhartha R, et al. Efficacy of ultrasound-guided transversus abdominis plane (TAP) block for postoperative analgesia in laparoscopic gastric sleeve resection: a randomized single blinded case control study. Surg Endosc. 2018;32(12):4985–9.
Sinha A, Jayaraman L, Punhani D. Efficacy of ultrasound-guided transversus abdominis plane block after laparoscopic bariatric surgery: a double blind, randomized, controlled study. Obes Surg. 2013;23(4):548–53.
Saber AA, Lee YC, Chandrasekaran A, et al. Efficacy of transversus abdominis plane (TAP) block in pain management after laparoscopic sleeve gastrectomy (LSG): a double-blind randomized controlled trial. Am J Surg. 2019;217(1):126–32.
Sherif AA, Koptan HM, Soliman SM. Feasibility and perioperative pain-relieving efficacy of ultrasound-guided transversus abdominis plane block in morbidly obese patients undergoing laparoscopic bariatric surgery. Research and Opinion in Anesthesia and Intensive Care. 2015;2(2):50.
Ibrahim M, Shamaa HE. Efficacy of ultrasound-guided oblique subcostal transversus abdominis plane block after laparoscopic sleeve gastrectomy: a double blind, randomized, placebo controlled study. Egyptian Journal of Anaesthesia. 2014;30(3):285–92.
Emile SH, Abdel-Razik MA, Elbahrawy K, et al. Impact of ultrasound-guided transversus abdominis plane block on postoperative pain and early outcome after laparoscopic bariatric surgery: a randomized double-blinded controlled trial. Obes Surg. 2019;29(5):1534–41.
Tülübaş EK, Seyit H, Bostancı İ, et al. Laparoskopik Transversus Abdominis Plan Bloğu Laparoskopik Sleeve Gastrektomi için Multimodal Analjezide Etkilidir. Bakırköy Tıp Dergisi. 15(3):198–203.
Joris J, Thiry E, Paris P, et al. Pain after laparoscopic cholecystectomy: characteristics and effect of intraperitoneal bupivacaine. Anesth Analg. 1995;81(2):379–84.
Mouton W, Bessel J, Otten KT, et al. Pain after laparoscopy. Surg Endosc. 1999;13:445–8.
Lee I-O, Kim S-H, Kong M-H, et al. Pain after laparoscopic cholecystectomy: the effect and timing of incisional and intraperitoneal bupivacaine. Can J Anesth. 2001;48(6):545–50.
Tam T, Harkins G, Wegrzyniak L, et al. Infiltration of bupivacaine local anesthetic to trocar insertion sites after laparoscopy: a randomized, double-blind, stratified, and controlled trial. J Minim Invasive Gynecol. 2014;21(6):1015–21.
Ortiz J, Suliburk JW, Wu K, et al. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. 2012;37(2):188–92.
Saranteas T. Limitations in ultrasound imaging techniques in anesthesia: obesity and muscle atrophy? Anesth Analg. 2009;109(3):993–4.
Shmulewitz A, Teefey SA, Robinson BS. Factors affecting image quality and diagnostic efficacy in abdominal sonography: a prospective study of 140 patients. J Clin Ultrasound. 1993;21(9):623–30.
Author information
Authors and Affiliations
Contributions
Conceived and designed experiments: MAA, SMS, HH.
Performed the experiments: MAA, SMS.
Analysed the data: MAA, SMS, HH.
Wrote the manuscript: MAA, SMS, HH.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interests.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Fig. 1
Sensitivity analysis of narcotic consumption at 24 h in ultrasound-guided TAP block only (PNG 1627 kb)
Supplementary Fig. 2
Sensitivity analysis of time to ambulation in laparoscopic sleeve gastrectomy only (PNG 233 kb)
Supplementary Fig. 3
Sensitivity analysis of complications in laparoscopic sleeve gastrectomy only (PNG 1592 kb)
Rights and permissions
About this article
Cite this article
Aamir, M.A., Sahebally, S.M. & Heneghan, H. Transversus Abdominis Plane Block in Laparoscopic Bariatric Surgery—a Systematic Review and Meta-Analysis of Randomized Controlled Trials. OBES SURG 31, 133–142 (2021). https://doi.org/10.1007/s11695-020-04898-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04898-2