Abstract
Background
Emerging evidence has revealed that obstructive sleep apnea (OSA) is associated with non-alcoholic fatty liver disease (NAFLD). However, the impact of OSA on NAFLD among obese patients undergoing metabolic and bariatric surgery (MBS), especially during follow-up period, remains unclear.
Objective
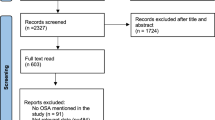
To analyze the correlation based on preoperative characteristics and postoperative conditions among bariatric patients with comorbid OSA and NAFLD. Methods: Clinical data of patients who underwent MBS in our institution between January 2016 and June 2019 were reviewed retrospectively. Correlation analysis and linear regressions were used to identify how OSA links with NAFLD before and after treatment of MBS.
Results
Of 308 patients, 181 were diagnosed with OSA and enrolled in the present study, and 127 completed follow-up visits at 6 months. The proportion of NAFLD in the mild-moderate OSA and severe OSA groups was 75.0% and 96.0%, respectively. MBS was effective at improving sleep apnea and nocturnal hypoxia, as well as liver steatosis and fibrosis (P < 0.05). And we also found that there were significant correlations not only between OSA- and NAFLD-related characteristics at baseline but also between their improvements after surgery, eventually leading to similar prognosis of NAFLD for both groups (P < 0.05), no matter what presurgical differences existed. In addition, the results of the univariate and multivariate linear regression analyses supported preoperative liver/spleen Hounsfield units ratio (LSR) by computerized tomography (CT) as an independent predictor of the effect of MBS on liver steatosis.
Conclusion
In conclusion, MBS plays a pivotal role in the control of medical conditions in obese patients with OSA and NAFLD. Given the correlation between OSA and NAFLD in the present study, in the case of both the severity at baseline as well as the improvement after surgery, OSA may pose an impact on the prognosis of NAFLD in bariatric patients.


Similar content being viewed by others
References
Thorpy M. International classification of sleep disorders: Springer New York; 2017. 1387–1394 p.
Tasali E, Ip MS. Obstructive sleep apnea and metabolic syndrome: alterations in glucose metabolism and inflammation. Proc Am Thorac Soc. 2008;5(2):207–17.
Mesarwi OA, Loomba R, Malhotra A. Obstructive sleep apnea, hypoxia, and nonalcoholic fatty liver disease. Am J Respir Crit Care Med. 2019;199(7):830–41.
Fan JG. Epidemiology of alcoholic and nonalcoholic fatty liver disease in China. J Gastroenterol Hepatol. 2013;28(Suppl 1):11–7.
Estes C, Razavi H, Loomba R, et al. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123–33.
Dulai PS, Singh S, Patel J, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 2017;65(5):1557–65.
Musso G, Olivetti C, Cassader M, et al. Obstructive sleep apnea-hypopnea syndrome and nonalcoholic fatty liver disease: emerging evidence and mechanisms. Semin Liver Dis. 2012;32(1):49–64.
Lemoine M, Serfaty L. Chronic intermittent hypoxia: a breath of fresh air in the understanding of NAFLD pathogenesis. J Hepatol. 2012;56(1):20–2.
Drager LF, Togeiro SM, Polotsky VY, et al. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62(7):569–76.
Aller R, Fernandez-Rodriguez C, Lo Iacono O, et al. Consensus document. Management of non-alcoholic fatty liver disease (NAFLD). Clinical practice guideline. Gastroenterol Hepatol. 2018;41(5):328–49.
Carneiro-Barrera A, Diaz-Roman A, Guillen-Riquelme A, et al. Weight loss and lifestyle interventions for obstructive sleep apnoea in adults: systematic review and meta-analysis. Obes Rev. 2019;4
Jakobsen GS, Smastuen MC, Sandbu R, et al. Association of bariatric surgery vs medical obesity treatment with long-term medical complications and obesity-related comorbidities. JAMA. 2018;319(3):291–301.
Salminen P, Helmio M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. JAMA. 2018;319(3):241–54.
Wong VW, Chan WK, Chitturi S, et al. Asia-Pacific Working Party on Non-alcoholic Fatty Liver Disease guidelines 2017-part 1: definition, risk factors and assessment. J Gastroenterol Hepatol. 2018;33(1):70–85.
Peromaa-Haavisto P, Tuomilehto H, Kossi J, et al. Obstructive sleep apnea: the effect of bariatric surgery after 12 months. A prospective multicenter trial. Sleep medicine (no pagination), 2017 [Internet]. 2017; Date of Publication: August 21. Available from: http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/941/CN-01372941/frame.html.
Nickel F, Tapking C, Benner L, et al. Bariatric surgery as an efficient treatment for non-alcoholic fatty liver disease in a prospective study with 1-year follow-up : BariScan Study. Obes Surg. 2018;28(5):1342–50.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–57.
Aminian A, Chang J, Brethauer SA, et al. ASMBS updated position statement on bariatric surgery in class I obesity (BMI 30-35 kg/m(2)). Surg Obes Relat Dis. 2018;14(8):1071–87.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253
Lee SS, Park SH, Kim HJ, et al. Non-invasive assessment of hepatic steatosis: prospective comparison of the accuracy of imaging examinations. J Hepatol. 2010;52(4):579–85.
Sakitani K, Enooku K, Kubo H, et al. Clinical characteristics of patients with diabetes mellitus and fatty liver diagnosed by liver/spleen Hounsfield units on CT scan. J Int Med Res. 2017;45(3):1208–20.
Zeng MD, Fan JG, Lu LG, et al. Guidelines for the diagnosis and treatment of nonalcoholic fatty liver diseases. J Dig Dis. 2008;9(2):108–12.
Hagstrom H, Nasr P, Ekstedt M, et al. Accuracy of non-invasive scoring systems in assessing risk of death and liver-related endpoints in patients with non-alcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2018;
Labenz C, Huber Y, Kalliga E, et al. Predictors of advanced fibrosis in non-cirrhotic non-alcoholic fatty liver disease in Germany. Aliment Pharmacol Ther. 2018;48(10):1109–16.
Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45(4):846–54.
Berry RB, Brooks R, Gamaldo C, et al. AASM scoring manual updates for 2017 (version 2.4). J Clin Sleep Med. 2017;13(5):665–6.
Musso G, Cassader M, Olivetti C, et al. Association of obstructive sleep apnoea with the presence and severity of non-alcoholic fatty liver disease. A systematic review and meta-analysis. Obes Rev. 2013;14(5):417–31.
Tanne F, Gagnadoux F, Chazouilleres O, et al. Chronic liver injury during obstructive sleep apnea. Hepatology. 2005;41(6):1290–6.
Savransky V, Nanayakkara A, Vivero A, et al. Chronic intermittent hypoxia predisposes to liver injury. Hepatology. 2007;45(4):1007–13.
Savransky V, Bevans S, Nanayakkara A, et al. Chronic intermittent hypoxia causes hepatitis in a mouse model of diet-induced fatty liver. Am J Physiol Gastrointest Liver Physiol. 2007;293(4):G871–7.
Bhatt SP, Guleria R, Vikram NK, et al. Association of inflammatory genes in obstructive sleep apnea and non alcoholic fatty liver disease in Asian Indians residing in north India. PLoS One. 2018;13(7):e0199599.
Xing T, Pilowsky PM, Fong AY. Mechanism of sympathetic activation and blood pressure elevation in humans and animals following acute intermittent hypoxia. Prog Brain Res. 2014;209:131–46.
Clanton J, Subichin M. The effects of metabolic surgery on fatty liver disease and nonalcoholic steatohepatitis. Surg Clin North Am. 2016;96(4):703–15.
Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism. 2016;65(8):1038–48.
Sundaram SS, Halbower A, Pan Z, et al. Nocturnal hypoxia-induced oxidative stress promotes progression of pediatric non-alcoholic fatty liver disease. J Hepatol. 2016;65(3):560–9.
Spahis S, Delvin E, Borys JM, et al. Oxidative stress as a critical factor in nonalcoholic fatty liver disease pathogenesis. Antioxid Redox Signal. 2017;26(10):519–41.
Doulberis M, Kotronis G, Gialamprinou D, et al. Non-alcoholic fatty liver disease: an update with special focus on the role of gut microbiota. Metabolism. 2017;71:182–97.
Nobili V, Alisi A, Cutrera R, et al. Altered gut-liver axis and hepatic adiponectin expression in OSAS: novel mediators of liver injury in paediatric non-alcoholic fatty liver. Thorax. 2015;70(8):769–81.
Zhang Y, Wang W, Yang C, et al. Improvement in nocturnal hypoxemia in obese patients with obstructive sleep apnea after bariatric surgery: a meta-analysis. Obes Surg. 2018;9
Schwarz AC, Billeter AT, Scheurlen KM, et al. Comorbidities as an indication for metabolic surgery. Visc Med. 2018;34(5):381–7.
Lassailly G, Caiazzo R, Buob D, et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology. 2015;149(2):379–88. quiz e315–376
Grimm IS, Schindler W, Haluszka O. Steatohepatitis and fatal hepatic failure after biliopancreatic diversion. Am J Gastroenterol. 1992;87(6):775–9.
Hocking MP, Davis GL, Franzini DA, et al. Long-term consequences after jejunoileal bypass for morbid obesity. Dig Dis Sci. 1998;43(11):2493–9.
Sundaram SS, Halbower AC, Klawitter J, et al. Treating obstructive sleep apnea and chronic intermittent hypoxia improves the severity of nonalcoholic fatty liver disease in children. J Pediatr. 2018;198:67–75. e1
Yeo SC, Ong WM, Cheng KSA, et al. Weight loss after bariatric surgery predicts an improvement in the non-alcoholic fatty liver disease (NAFLD) fibrosis score. Obes Surg. 2019;29(4):1295–300.
Zhang YX, Wang WY, Yang CC, et al. Evaluation of one-year effects of metabolic and bariatric surgery on obesity with nonalcoholic fatty liver disease. J Abdom Surg. 2019;32(3):172–176,176.
Funding
This work was supported by the Clinical Research Plan of SHDC (No.16CR2005A) and Clinical Research Program of 9th People’s Hospital affiliated to Shanghai Jiao Tong University School of Medicine (JYLJ0130).
Author information
Authors and Affiliations
Contributions
All authors were involved in drafting the article of revising it critically for important intellectual content, and all authors approved the final version to be published. ZYX and YL had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. WB, LXF, YCC, WWY, SJH, SML, YY, DQC, GY, and YJJ were responsible for study conception and design. HM, NJ, SJL, ZL, and SHX were responsible for data acquisition. YWW and YK were responsible for the analysis and interpretation of data.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest with the publication of this manuscript.
Informed Consent
Informed consent was obtained from all individual participants included in the study
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhang YX is the first author of this article, and Yang L is the co-first author of this article.
Electronic Supplementary Material
ESM 1
(DOCX 332 kb)
Rights and permissions
About this article
Cite this article
Zhang, Y.X., Yang, L., Yang, C.C. et al. Correlation between Obstructive Sleep Apnea and Non-Alcoholic Fatty Liver Disease before and after Metabolic Bariatric Surgery. OBES SURG 30, 3803–3812 (2020). https://doi.org/10.1007/s11695-020-04696-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04696-w