Abstract
Objective
To evaluate the efficacy and safety of a hospital-made resuscitation pack, a Chinese medicinal herbal compound formula designed to enhance recovery in post-bronchoscopy patients.
Methods
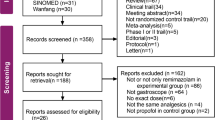
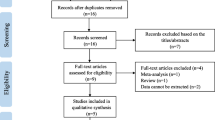
In this randomized, single-blind, placebo-controlled clinical trial, eligible patients were randomly assigned 1:1 to either the treatment or control groups. The patients in the treatment group applied the resuscitation pack, which contained aromatic compounded Chinese herbs. The patients in the control group applied a hospital-made, single herb placebo pack. Packs were placed on the Tiantu (CV 22) acupuncture point for 4 h as soon as the bronchoscopy finished. Efficacy indicators, such as recovery time, patients’ symptoms including nausea and dizziness, and adverse events (AEs) were observed and compared. The outcome indices were evaluated at baseline, 1 and 24 h after the bronchoscopy. Subgroup analysis was further performed by patients’ age and depth of sedation.
Results
When applying generalized estimating equations (GEE) to evaluate the intensity of post-bronchoscopy nausea and vomiting, the intensity was lower in the treatment group (163 cases) compared with the control group (162 cases; 95% CI: 0.004, 0.099, P=0.03]. Also, significantly lower intensity of nausea was observed in the 60–70 years of age subgroup (95% CI: 0.029, 0.169, P=0.006) and deep sedation subgroup (95% CI: 0.002, 0.124; P=0.04). There was no significant difference in dizziness between two groups by GEE (95% CI: −0.134, 0.297; P=0.459). In addition, no serious AEs were observed in either group.
Conclusions
Our study found that the resuscitation pack markedly improved patients’ symptoms by reducing nausea and vomiting after bronchoscopy without AEs, compared with placebo in the perioperative period. (Trial registration No. ChiCTR2000038299)
Similar content being viewed by others
References
Clark G, Licker M, Younossian AB, Soccal PM, Frey JG, Rochat T, et al. Titrated sedation with propofol or midazolam for flexible bronchoscopy: a randomized trial. Eur Respir J 2009;34:1277–1283.
Yao Y, Su Z, Chen Y, Ye Y, Lu L, Zhong C, et al. Safety and efficacy of sufentanil combined with midazolam in bronchoscopy under conscious sedation: a retrospective study of 11,158 cases. J Thorac Dis 2019;11:4127–4134.
Kern M, Kerner T, Tank S. Sedation for advanced procedures in the bronchoscopy suite: proceduralist or anesthesiologist?. Curr Opin Anaesthesiol 2017;30:490–495.
Pawlowski J. Anesthetic considerations for interventional pulmonary procedures. Thorac Anesthes 2013;26:6–12.
Bowling MR, Kohan MW, Walker P, Efird J, Ben Or S. The effect of general anesthesia versus intravenous sedation on diagnostic yield and success in electromagnetic navigation bronchoscopy. Brochol Interv Pulmonol 2015;22:5–13.
Gan TJ. Postoperative nausea and vomiting—Can it be eliminated? JAMA 2002;287:1233–1236.
Obrink E, Jildenstal P, Oddby E, Jakobsson JG. Postoperative nausea and vomiting: update on predicting the probability and ways to minimize its occurrence, with focus on ambulatory surgery. Int J Surg 2015;15:100–106.
Horn CC, Wallisch WJ, Homanics GE, Williams JP. Pathophysiological and neurochemical mechanisms of postoperative nausea and vomiting. Eur J Pharmacol 2014;5:55–66.
Kovac AL. Update on the management of postoperative nausea and vomiting. Drugs 2013;73:1525–1547.
De Oliveira GS Jr, Castro-Alves LJ, Chang R, Yaghmour E, McCarthy RJ. Systemic metoclopramide to prevent postoperative nausea and vomiting: a meta-analysis without Fujii’s studies. Br J Anaesth 2012;109:688–697.
Liodden I, Norheim AJ. Acupuncture and related techniques in ambulatory anesthesia. Curr Opin Anaesthesiol 2013;26:661–668.
Hurwitz Erin E, Michelle S, Vinta Sandhya R, Zehm Charles F, Shabot Sarah M, Minhajuddin Abu, et al. Adding examples to the ASA-physical status classification improves correct assignment to patients. Anesthesiology 2017;126:614–622.
Dixon JS, Bird HA. Reproducibility along a 10 cm vertical visual analogue scale. Ann Rheum Dis 1981;40:87–89.
Seijo LM, Sterman DH. Interventional pulmonology. N Engl J Med 2001;344:740–749.
José RJ, Shaefi S, Navani N. Sedation for flexible bronchoscopy: current and emerging evidence. Eur Respir Rev 2013;128:106–116.
McCambridge AJ, Boesch RP, Mullon JJ. Sedation in bronchoscopy: a review. Clin Chest Med 2018;39:65–77.
Strohleit D, Galetin T, Kosse N, Lopez-Pastorini A, Stoelben E. Guidelines on analgosedation, monitoring, and recovery time for flexible bronchoscopy: a systematic review. BMC Pulm Med 2021;21:198–211.
Kim SH, Cho JY, Kim M, Chung JM, Yang J, Seong C, et al. Safety and efficacy of remimazolam compared with midazolam during bronchoscopy: a single-center, randomized controlled study. Sci Rep 2023;13:20498–20506.
Wang LP, Feng JF, Hu KL. Progress in regulation effect of aromatic refreshing traditional Chinese medicine on BBB permeability and its mechanism. China J Chin Mater Med (Chin) 2014;39:949–954.
Acknowledgments
The authors thank the patients for participating in this trial and the study investigators at the hospital centers for their role in data collection.
Author information
Authors and Affiliations
Contributions
Conception and design, writing the original draft: Tan XY; methodology and investigation: Xu YJ; methodology and formal analysis: Yao Y and Xiao JM; provision of materials: Zhang XS; investigation (participant enrolment, experimental intervention, and follow-up): Chai DY and Fan FT; paper review and editing: Wu ZH; data management: Sun LL; operation: Tan XY; anesthetization: Lin M. All authors read and approved the final version for publication.
Corresponding author
Ethics declarations
There are no known conflicts of interest associated with this publication and there has no financial support for this work that could have influenced its outcome.
Additional information
Supported by the Specific Research Fund for TCM Science and Technology of Guangdong Provincial Hospital of Chinese Medicine (No. YN2018QL02)
Rights and permissions
About this article
Cite this article
Tan, Xy., Yao, Y., Xiao, Jm. et al. Efficacy and Safety of Chinese Medicine Resuscitation Pack for Enhanced Recovery after Bronchoscopy: A Randomized, Single-Blind, Placebo-Controlled Clinical Trial. Chin. J. Integr. Med. (2024). https://doi.org/10.1007/s11655-024-3569-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s11655-024-3569-z