Abstract
Objective
To evaluate the effects of interactive dynamic scalp acupuncture (IDSA), simple combination therapy (SCT), and traditional scalp acupuncture (TSA) on motor function and gait of the lower limbs in post-stroke hemiplegia patients.
Methods
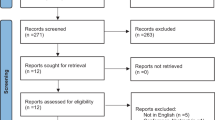
A total of 231 patients with post-stroke hemiplegia was randomly divided into IDSA (78 cases), SCT (78 cases), and TSA (75 cases) groups by a random number table. Scalp acupuncture (SA) and lower-limb robot training (LLRT) were both performed in the IDSA and SCT groups. The patients in the TSA group underwent SA and did not receive LLRT. The treatment was administered once daily and 6 times weekly for 8 continuous weeks, each session lasted for 30 min. The primary outcome measures included Fugl-Meyer assessment of the lower extremity (FMA-LE), berg balance scale (BBS), modified barthel index (MBI), and 6-min walking test (6MWT). The secondary outcome measures included stride frequency (SF), stride length (SL), stride width (SW), affected side foot angle (ASFA), passive range of motion (PROM) of the affected hip (PROM-H), knee (PROM-K) and ankle (PROM-A) joints. The patients were evaluated before treatment, at 1- and 2-month treatment, and 1-, and 2-month follow-up visits, respectively. Adverse events during 2-month treatment were observed.
Results
Nineteen patients withdrew from the trial, with 8 in the IDSA and 5 in the SCT groups, 6 in the TSA group. The FMA-LE, BBS, 6MWT and MBI scores in the IDSA group were significantly increased after 8-week treatment and 2 follow-up visits compared with the SCT and TSA groups (P<0.05 or P<0.01). Compared with pre-treatment, the grade distribution of BBS and MBI scores in the 3 groups were significantly improved at 1, 2-month treatment and 2 follow-up visits (P<0.05 or P<0.01). The SF, PROM-H, PROM-K and PROM-A in the IDSA group was significantly increased compared with the SCT and TSA groups after 8-week of treatment (P<0.05 or P<0.01). Compared with the SCT group, ASFA of the IDSA group was significantly reduced after 8-week of treatment (P<0.05). SF, SL, PROM-K and PROM-A were significantly increased at the 2nd follow-up visit whereas the ASFA was significantly reduced in the IDSA group compared with the SCT groups at 1st follow-up visit (P<0.05 or P<0.01). The SF was significantly increased in the SCT group compared with the TSA group after 8-week treatment (P<0.05). Compared with the TSA group, PROM-K, PROM-A were significantly increased at the 2nd follow-up visit (P<0.05).
Conclusions
The effects of IDSA on lower-limb motor function and walking ability of post-stroke patients were superior to SCT and TSA. The SCT was comparable to TSA treatment, and appeared to be superior in improving the motion range of the lower extremities. (Registration No. ChiCTR1900027206)
Similar content being viewed by others
Availability of Data and Material
The authors are available to provide data on request.
References
Hay SL, Abajobir AA, Abate KH. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1260–1344.
Woodbury ML, Howland DR, McGuirk TE, Davis SB, Senesac CR, Kautz S, et al. Effects of trunk restraint combined with intensive task practice on poststroke upper extremity reach and function: a pilot study. Neurorehabil Neural Repair 2009;23:78–91.
Gama GL, de Lucena Trigueiro LC, Simão CR, de Sousa AV, de Souza E Silva EM, Galvão ÉR, et al. Effects of treadmill inclination on hemiparetic gait: controlled and randomized clinical trial. Am J Phys Med Rehabil 2015;94:718–727.
Nikamp CDM, Hobbelink MSH, van der Palen J, Hermens HJ, Rietman JS, Buurke JH. A randomized controlled trial on providing ankle-foot orthoses in patients with (sub-)acute stroke: short-term kinematic and spatiotemporal effects and effects of timing. Gait Posture 2017;55:15–22.
Schwartz I, Sajin A, Fisher I, Neeb M, Shochina M, Katz-Leurer M, et al. The effectiveness of locomotor therapy using robotic-assisted gait training in subacute stroke patients: a randomized controlled trial. PM R 2009;1:516–523.
Verniba D, Vergara ME, Gage WH. Force plate targeting has no effect on spatiotemporal gait measures and their variability in young and healthy population. Gait Posture 2015;41:551–556.
Hesse S, Waldner A, Tomelleri C. Innovative gait robot for the repetitive practice of floor walking and stair climbing up and down in stroke patients. J Neuroeng Rehabil 2010;28;7:30.
Orand A, Erdal Aksoy E, Miyasaka H, Weeks Levy C, Zhang X, Menon C. Bilateral tactile feedback-enabled training for stroke survivors using microsoft Kinect™. Sensors (Basel) 2019; 9:3474.
Noble S, Pearcey GEP, Quartly C, Zehr EP. Robot controlled, continuous passive movement of the ankle reduces spinal cord excitability in participants with spasticity: a pilot study. Exp Brain Res 2019; 37:3207–3220.
Colombo G, Joerg M, Schreier R, Dietz V. Treadmill training of paraplegic patients using a robotic orthosis. J Rehabil Res Dev 2000;37:693–700.
Moore JL, Roth EJ, Killian C, Hornby TG. Locomotor training improves daily stepping activity and gait efficiency in individuals poststroke who have reached a “plateau” in recovery. Stroke 2010;41:129–135.
van Kammen K, Boonstra AM, van der Woude LHV, Reinders-Messelink HA, den Otter R. Differences in muscle activity and temporal step parameters between Lokomat guided walking and treadmill walking in post-stroke hemiparetic patients and healthy walkers. J Neuroeng Rehabil 2017;14:32.
Chang WH, Kim MS, Huh JP, Lee PK, Kim YH. Effects of robot-assisted gait training on cardiopulmonary fitness in subacute stroke patients: a randomized controlled study. Neurorehabil Neural Repair 2012;26:318–324.
Wang J, Pei J, Cui X, Sun K, Ni H, Zhou C, et al. Interactive dynamic scalp acupuncture combined with occupational therapy for upper limb motor impairment in stroke: a randomized controlled trial. Chin Acupunct Moxibust (Chin) 2015;35:983–989.
Chinese Association for Neurosciences, China Neurosurgery Association. Keypoints in diagnosis for various types of cerebrovascular disease. Chin J Neurol (Chin) 1996;29:379–380.
Zhang SH, Zhang TF, Wang YL, Xiao P. Effect of interactive dynamic scalp acupuncture on plantar pressure distribution during walking in stroke patients with hemiplegia. J Basic Chin Med (Chin) 2018;24:1109–1112.
Liu JP. Calculation of sample content in clinical trials. Chin J Integr Med (Chin) 2003;7:57–59.
Hao JJ, Hao LL. Review of clinical applications of scalp acupuncture for paralysis: an excerpt from Chinese scalp acupuncture. Glob Adv Health Med 2012;1:102–121.
Young-Nim Y, Gwang-Cheon P, Myung-Rae C, Min-Yeong S, Chang-Su N, Jae-Young H, et al. Meta-analysis on randomized controlled trials for scalp acupuncture treatment of stroke: a systematic review. J Tradit Chin Med 2018;38:465–479.
Sullivan KJ, Tilson JK, Cen SY, Rose DK, Hershberg J, Correa A, et al. Fugl-Meyer assessment of sensorimotor function after stroke: standardized training procedure for clinical practice and clinical trials. Stroke 2011;42:427–432.
Berg KO, Wood-Dauphinee SL, Williams JL. The balance scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med 1995;27:27–36.
Stevenson TJ, Garland SJ. Standing balance during internally produced perturbations in subjects with hemiplegia: validation of the balance scale. Arch Phys Med Rehabil 1996;77:656–662.
Agarwala P, Salzman SH. Six-minute walk test: clinical role, technique, coding, and reimbursement. Chest 2020;157:603–611.
Mahoney FL. Functional evaluation: the Barthel Index. Maryland St Med J 1965;14:61–65.
Carozzo S, Serra S, Pignolo L, Tonin P, Cerasa A. The assessment of trunk recovery in stroke patients using 3D kinematic measures. Med Eng Phys 2020;78:98–105.
Jamari J, Anwar IB, Saputra E, van der Heide E. Range of motion simulation of hip joint movement during salat activity. J Arthroplasty 2017;32:2898–2904.
Wang JX, Ma LX, Song Y, Mu JD, Gan YY. Analysis of the significance of kinetic needling in the treatment of spasm. Chin Acupunct Moxibust (Chin) 2019;39:1335–1338.
Huang G, Ceccarelli M, Huang Q, Zhang W, Yu Z, Chen X, et al. Design and feasibility study of a leg-exoskeleton assistive wheelchair robot with tests on gluteus medius muscles. Sensors (Basel) 2019; 28;19:548.
Yao XQ, Li XL, Du XZ, Wang JH, Yuan B, Zhang TZ, et al. Effect of scalp acupuncture stimulation on expression of pentraxin 3 in striatum in acute ischemic cerebrovascular disease rats. Acupunct Res (Chin) 2019;44:793–798.
Xiong J, Zhang Z, Ma Y, Li Z, Zhou F, Qiao N, et al. The effect of combined scalp acupuncture and cognitive training in patients with stroke on cognitive and motor functions. Neurorehabilitation 2020;46:75–82.
Lee GE, Lee PT, Ran N, Zhou J. Scalp acupuncture for children with cerebral palsy: a protocol for a systematic review. Medicine (Baltimore) 2019;98:e18062.
Kao TC, Yang CM. The role of Yamamoto new scalp acupuncture as an independent treatment for sudden sensorineural hearing loss: a case report. Acupunct Med 2020;38:126–128.
Wang J, Pei J, Cui X, Sun K, Fu Q, Xing C, et al. Individualized scalp acupuncture for motor dysfunction in stroke: a randomized controlled trial. Chin Acupunct Moxibust (Chin) 2017;37:918–924.
Han JY, Kim JH, Park JH, Song MY, Song MK, Kim DJ, et al. Scalp acupuncture and electromagnetic convergence stimulation for patients with cerebral infarction: study protocol for a randomized controlled trial. Trials 2016;17:490.
Yan RJ, Cheng B, Chen LS, Shen XY, Zong L. Clinical observation of relaxing needling plus joint needling from the internal medicine for post-stroke spastic hemiplegia. Shanghai J Acu-Mox (Chin) 2016;35:930–934.
Zanella AK, Gutierres JM, Stigger F. Effects of scalp acupuncture on functional deficits induced by early sensorimotor restriction. J Acupunct Meridian Stud 2019;12:77–83.
Hsing WT, Imamura M, Weaver K, Fregni F, Azevedo Neto RS. Clinical effects of scalp electrical acupuncture in stroke: a sham-controlled randomized clinical trial. J Altern Complement Med 2012;18:341–346.
Zhang CX, Zhang SH, Wang YL, Zhang CP, Li QF, Pan WY, et al. Interactive scalp acupuncture for cognitive dysfunction after stroke: a randomized controlled trial. Chin Acupunct Moxibust (Chin) 2021;41:252–256.
Qi L, Han Z, Zhou Y, Chen W, Chu L, Lu J, et al. Dynamic scalp acupuncture combined with PNF therapy for upper limb motor impairment in ischemic stroke spastic hemiplegia. Chin Acupunct Moxibust (Chin) 2018;38:234–238.
Du XZ, Bao CL, Dong GR, Yang XM. Immediate effects of scalp acupuncture with twirling reinforcing manipulation on hemiplegia following acute ischemic stroke: a hidden association study. Neural Regen Res 2016;11:758–764.
Fang Z, Ning J, Xiong C, Yao SL. Effects of electroacupuncture at head points on the function of cerebral motor areas in stroke patients: a PET study. Evid-Based Complement Alternat Med 2012; 2012:214–215.
Zhuang Y, Lu JJ, Meng FP, Sun KX, Zhan Q. Rehabilitation evaluation of interactive scalp acupuncture therapy for post-stroke gait in hemiplegia. J Neurol Neurorehabil 2016;12:71–75.
Acknowledgements
The authors thank all the participants in present study for their participation and valuable feedbacks. as well as the physical therapist at the rehabilitation hospital for performing the conventional training.
Author information
Authors and Affiliations
Contributions
Zhang SH designed the experiment, analyzed and interpreted the data, and drafted the manuscript. Wang YL contributed to the study design. Zhang CX collected and analyzed the data. Zhang CP, Xiao P and Li QF assisted the conduction of the trials and the improvement of the test protocol. Liang WR and Pan XH contributed to the interpretation and revision of manuscript. Zhou M contributed to proofreading the paper. All authors have read and approved the final manuscript for publication.
Corresponding author
Additional information
Conflict of Interest
All the authors have no possible conflicts of interest.
Supported by Medical Research Fund of Guangdong, China (No. A2020448), Special Fund Support Project for Industrial Development in Dapeng New District, Shenzhen of Guangdong Province, China (No. YL202001-16), Medical and Health Research Fund Project of Medical and Health Group in Dapeng New District, Shenzhen, Guangdong Province, China (No. 2019JTYM003, 2019JTYM004)
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Zhang, Sh., Wang, Yl., Zhang, Cx. et al. Effects of Interactive Dynamic Scalp Acupuncture on Motor Function and Gait of Lower Limbs after Stroke: A Multicenter, Randomized, Controlled Clinical Trial. Chin. J. Integr. Med. 28, 483–491 (2022). https://doi.org/10.1007/s11655-021-3525-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11655-021-3525-0