Abstract
Background
Segmental resections of the duodenum are uncommonly performed and are technically challenging due to intimate relationships with the biliary tree, pancreas, and superior mesenteric vessels. The objective of this study was to assess indications, operative strategy, and outcomes of duodenal resections and to advocate that this form of resection deserves its own unique Current Procedural Terminology (CPT) and Relative Value Unit (RVU) structure.
Methods
Patients undergoing isolated and partial duodenal resection from 2008-2023 at University of Tennessee Health Science Center affiliated hospitals were retrospectively reviewed. Factors examined included clinical presentation, diagnostic evaluation, operative time, and technique, 90-day morbidity and mortality, and pathologic and survival outcomes.
Results
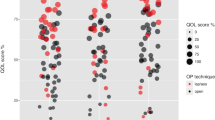
Thirty-one patients were identified with majority female and a median age of 61. Diagnostic studies included computed tomography and upper (including push) endoscopy. Reconstruction most often involved side-to-side duodenojejunostomy following distal duodenal resection. Intraoperative evaluation (IOE) of the biliary tree was utilized to assess and protect pancreaticobiliary structures in eleven patients. Median operative time was 206 min, increasing to 236 min when IOE was necessary. Procedure-related morbidity was 23% with one 90-day mortality. Median postoperative length of stay was 9 days. Pathology included benign adenoma, adenocarcinoma, GIST, neuroendocrine neoplasms, and erosive metastatic deposit.
Conclusion
Duodenal resections can be effectively employed to safely address diverse pathologies. These procedures are characterized by long operative times, extended hospital stays, and an incidence of postoperative complications that mimics that of pancreatic resection. This work highlights the need for modification to the CPT system to accurately define these distinct procedures for future research endeavors and development of a more accurate valuation unit.

Similar content being viewed by others
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary material. Raw data that suport the findings of this study are available from the corresponding author, upon reasonable request.
References
Bakaeen FG, Murr MM, Sarr MG, et al. What prognostic factors are important in duodenal adenocarcinoma? Arch Surg. Jun 2000;135(6):635-41; discussion 641-2. https://doi.org/10.1001/archsurg.135.6.635
Cloyd JM, Norton JA, Visser BC, Poultsides GA. Does the extent of resection impact survival for duodenal adenocarcinoma? Analysis of 1,611 cases. Ann Surg Oncol. Feb 2015;22(2):573-80. https://doi.org/10.1245/s10434-014-4020-z
Kaklamanos IG, Bathe OF, Franceschi D, Camarda C, Levi J, Livingstone AS. Extent of resection in the management of duodenal adenocarcinoma. Am J Surg. Jan 2000;179(1):37-41. https://doi.org/10.1016/s0002-9610(99)00269-x
Zhou B, Zhang M, Wu J, Yan S, Zhou J, Zheng S. Pancreaticoduodenectomy versus local resection in the treatment of gastrointestinal stromal tumors of the duodenum. World J Surg Oncol. Aug 2013;11:196. https://doi.org/10.1186/1477-7819-11-196
Blanco-Fernandez G, Rojas-Holguin A, De-Armas-Conde N, Gallarin-Salamanca I, Lopez-Guerra D, Jaen-Torrejimeno I. Side-to-side duodenojejunostomy after resection of third and fourth duodenal portions with pancreatic preservation. Updat Surg. Dec 2020;72(4):1105-1113. https://doi.org/10.1007/s13304-020-00823-5
Dorcaratto D, Heneghan HM, Fiore B, et al. Segmental duodenal resection: indications, surgical techniques and postoperative outcomes. J Gastrointest Surg. Apr 2015;19(4):736-42. https://doi.org/10.1007/s11605-015-2744-0
Mitchell WK, Thomas PF, Zaitoun AM, Brooks AJ, Lobo DN. Pancreas preserving distal duodenectomy: A versatile operation for a range of infra-papillary pathologies. World J Gastroenterol. Jun 21 2017;23(23):4252-4261. https://doi.org/10.3748/wjg.v23.i23.4252
Bourgouin S, Hornez E, Guiramand J, et al. Duodenal gastrointestinal stromal tumors (GISTs): arguments for conservative surgery. J Gastrointest Surg. Mar 2013;17(3):482-7. https://doi.org/10.1007/s11605-012-2075-3
Garcia-Molina FJ, Mateo-Vallejo F, Franco-Osorio Jde D, Esteban-Ramos JL, Rivero-Henandez I. Surgical approach for tumours of the third and fourth part of the duodenum. Distal pancreas-sparing duodenectomy. Int J Surg. Jun 2015;18:143-8. https://doi.org/10.1016/j.ijsu.2015.04.051
Golhar A, Mangla V, Mehrotra S, Lalwani S, Mehta N, Nundy S. Limited distal duodenal resection: Surgical approach and outcomes. A case series. Ann Med Surg (Lond). Jun 2018;30:36-41. https://doi.org/10.1016/j.amsu.2018.04.005
Sakr A, Emile SH, Abdallah E, Thabet W, Khafagy W. Predictive Factors for Small Intestinal and Colonic Anastomotic Leak: a Multivariate Analysis. Indian J Surg. Dec 2017;79(6):555-562. https://doi.org/10.1007/s12262-016-1556-0
Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg. Jul 2006;244(1):10-5. https://doi.org/10.1097/01.sla.0000217673.04165.ea
Penumadu P, Barreto SG, Goel M, Shrikhande SV. Pancreatoduodenectomy - preventing complications. Indian J Surg Oncol. Mar 2015;6(1):6-15. https://doi.org/10.1007/s13193-013-0286-z
Kim MJ, Choi SB, Han HJ, et al. Clinicopathological analysis and survival outcome of duodenal adenocarcinoma. Kaohsiung J Med Sci. May 2014;30(5):254-9. https://doi.org/10.1016/j.kjms.2013.12.006
Sun H, Liu Y, Lv L, Li J, Liao X, Gong W. Prognostic Factors and Clinical Characteristics of Duodenal Adenocarcinoma With Survival: A Retrospective Study. Front Oncol 2021;11:795891. https://doi.org/10.3389/fonc.2021.795891
Burch J, Ahmad I. Gastrointestinal Stromal Cancer. StatPearls. 2022.
Chok AY, Koh YX, Ow MY, Allen JC, Jr., Goh BK. A systematic review and meta-analysis comparing pancreaticoduodenectomy versus limited resection for duodenal gastrointestinal stromal tumors. Ann Surg Oncol. Oct 2014;21(11):3429-38. https://doi.org/10.1245/s10434-014-3788-1
Onkendi EO, Boostrom SY, Sarr MG, et al. 15-year experience with surgical treatment of duodenal carcinoma: a comparison of periampullary and extra-ampullary duodenal carcinomas. J Gastrointest Surg. Apr 2012;16(4):682-91. https://doi.org/10.1007/s11605-011-1808-z
Spalding DR, Isla AM, Thompson JN, Williamson RC. Pancreas-sparing distal duodenectomy for infrapapillary neoplasms. Ann R Coll Surg Engl. Mar 2007;89(2):130-5. https://doi.org/10.1308/003588407X155815
Otani K, Ishihara S, Nozawa H, et al. A retrospective study of laparoscopic surgery for small bowel obstruction. Ann Med Surg (Lond). Apr 2017;16:34-39. https://doi.org/10.1016/j.amsu.2017.02.045
Al Abbas AI, Wang C, Hamad AB, et al. Mentorship and formal robotic proficiency skills curriculum improve subsequent generations’ learning curve for the robotic distal pancreatectomy. HPB. Dec 2021;23(12):1849-55.
Author information
Authors and Affiliations
Contributions
DP and SB: conceptualization, methodology, data curation, writing and editing of the final manuscript. AA: writing and editing of the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Patel, D.D., Abdulkarim, A.B. & Behrman, S.W. Segmental Duodenal Resections: Toward Defining Indications, Complexity, and Coding. J Gastrointest Surg 27, 2373–2379 (2023). https://doi.org/10.1007/s11605-023-05837-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05837-z