Abstract
Background
This study aims to propose a novel classification system to standardize the treatment of hepatolithiasis.
Methods
A hepatolithiasis classification named LHO was proposed to represent the distribution of stones in the segmental bile ducts and the hepatic atrophy associated with the stones (L), the existence of stones or strictures in the hilar bile duct (H), and dysfunction of the Oddi sphincter (O), which can be used to formulate ideal surgical protocols. One hundred and forty-seven primary hepatolithiasis patients treated between 2013 and 2018 were classified into different types and divided into two groups. If the patient’s actual surgical procedure matched the ideal surgical protocol, the patients were included in the matching group; otherwise, patients were included in the nonmatching group. The rates of residual stones, recurrence, and a good quality of life (QOL) were analyzed among the patients in the matching and nonmatching groups and previous reports.
Results
According to the classification of each patient, 77.6% of the patients were included in the matching group, and 22.4% were included in the nonmatching group. The rates of residual stones, recurrence, and a good QOL were significantly better in the matching group than in the nonmatching group (9.6% vs. 27.3%; 8.0% vs. 35.0%; 89.5% vs. 65.4%); the rates of residual stones and a good QOL were also better than those in previous reports (9.6% vs. 19.1%; 89.5% vs. 61.6%).
Conclusions
The LHO classification can comprehensively reflect the key points of treatment, which is beneficial for formulating effective and standardized surgical plans of hepatolithiasis.


Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- MRCP:
-
Magnetic resonance cholangiopancreatography
- QOL:
-
Quality of life
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Author names in bold designate shared co-first authorship
Kim HJ, Kim JS, Joo MK, Lee BJ, Kim JH, Yeon JE, et al. Hepatolithiasis and intrahepatic cholangiocarcinoma: A review. World J Gastroenterol. 2015;21:13418-13431. [https://doi.org/10.3748/wjg.v21.i48.13418. PMID: 26730152; PMCID: PMC4690170.]
Feng X, Zheng S, Xia F, Ma K, Wang S, Bie P, et al. Classification and management of hepatolithiasis: A high-volume, single-center's experience. Intractable Rare Dis Res. 2012;1:151-156. [https://doi.org/10.5582/irdr.2012.v1.4.151. PMID: 25343089; PMCID: PMC4204570.]
Tsunoda T, Tsuchiya R, Harada N, Yoshino R, Noda T, Izawa K, et al. Long-term results of surgical treatment for intrahepatic stones. Jpn J Surg. 1985;15:455-462. [https://doi.org/10.1007/BF02470091. PMID: 3831500.]
Dong JH, Zheng SG, Chen P, Han DB. Guidelines for the diagnosis and treatment of hepatolithiasis. Zhonghua Xiaohua Waike Zazhi. 2007;6;156-161. [https://doi.org/10.3760/cma.j.issn.1673-9752.2007.02.028.]
Uenishi T, Hamba H, Takemura S, Oba K, Ogawa M, Yamamoto T, et al. Outcomes of hepatic resection for hepatolithiasis. Am J Surg. 2009;198:199–202. [https://doi.org/10.1016/j.amjsurg.2008.08.020. Epub 2009 Feb 27. PMID: 19249730.]
Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009;146:843–853. [https://doi.org/10.1016/j.surg.2009.04.009. Epub 2009 Jun 28. PMID: 19744434.]
Clavien PA, Petrowsky H, DeOliveira ML, Graf R. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med. 2007;356:1545-1559. [https://doi.org/10.1056/NEJMra065156. PMID: 17429086.]
Nakayama F. Intrahepatic calculi: a special problem in East Asia. World J Surg. 1982;6:802-804. [https://doi.org/10.1007/BF01655381. PMID: 7180014.]
Liu FB, Yu XJ, Wang GB, Zhao YJ, Xie K, Huang F, et al. Preliminary study of a new pathological evolution-based clinical hepatolithiasis classification. World J Gastroenterol. 2015;21:2169-2177. [https://doi.org/10.3748/wjg.v21.i7.2169. PMID: 25717253; PMCID: PMC4326155.]
Liang TB, Liu Y, Bai XL, Yu J, Chen W. Sphincter of Oddi laxity: an important factor in hepatolithiasis. World J Gastroenterol. 2010;16:1014-1018. [https://doi.org/10.3748/wjg.v16.i8.1014. PMID: 20180243; PMCID: PMC2828588.]
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [https://doi.org/10.1097/01.sla.0000133083.54934.ae. PMID: 15273542; PMCID: PMC1360123.]
Sakpal SV, Babel N, Chamberlain RS. Surgical management of hepatolithiasis. HPB (Oxford). 2009;11:194-202. [https://doi.org/10.1111/j.1477-2574.2009.00046.x. PMID: 19590647; PMCID: PMC2697895.]
Li C, Wen T. Surgical management of hepatolithiasis: A minireview. Intractable Rare Dis Res. 2017;6:102-105. [https://doi.org/10.5582/irdr.2017.01027. PMID: 28580209; PMCID: PMC5451740.]
Yang T, Lau WY, Lai EC, Yang LQ, Zhang J, Yang GS, et al. Hepatectomy for bilateral primary hepatolithiasis: a cohort study. Ann Surg. 2010;251:84-90. [https://doi.org/10.1097/SLA.0b013e3181b2f374. PMID: 20032719.]
Dong J, Lau WY, Lu W, Zhang W, Wang J, Ji W. Caudate lobe-sparing subtotal hepatectomy for primary hepatolithiasis. Br J Surg. 2012;99:1423-1428. [https://doi.org/10.1002/bjs.8888. PMID: 22961524.]
Wang W, Zhang Z, Wang J. Subtotal (segment II-VIII) hepatectomy for bilateral diffuse hepatolithiasis with compensatory caudate lobe hypertrophy: a report of two cases. BMC Gastroenterol. 2020;20:350. [https://doi.org/10.1186/s12876-020-01503-9. PMID: 33081716; PMCID: PMC7576830.]
Chen ZY, Yan LN, Zeng Y, Wen TF, Li B, Zhao JC, et al. Preliminary experience with indications for liver transplantation for hepatolithiasis. Transplant Proc. 2008;40:3517-3522. [https://doi.org/10.1016/j.transproceed.2008.07.142. PMID: 19100427.]
Tang DN, Wei JM, Liu YN, Qiao JC, Zhu MW, He XW. Liver transplantation in an adult patient with situs inversus: a case report and overview of the literature. Transplant Proc. 2008;40:1792-1795. [https://doi.org/10.1016/j.transproceed.2008.03.147. PMID: 18589199.]
Strong RW, Chew SP, Wall DR, Fawcett J, Lynch SV. Liver transplantation for hepatolithiasis. Asian J Surg. 2002;25:180-183. [https://doi.org/10.1016/S1015-9584(09)60170-6. PMID: 12376243.]
Wang J, Feng H. Chinese expert consensus on the clinical application path of peri-hepatic surgery technology (2020 edition). Zhongguo Shiyong Waike Zazhi. 2020;40:31–38. [https://doi.org/10.19538/j.cjps.issn1005-2208.2020.06.02.]
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease[J]. Hepatology, 2001, 33(2): 464-70. [https://doi.org/10.1053/jhep.2001.22172.]
Makuuchi M, Kokudo N. Clinical practice guidelines for hepatocellular carcinoma: the first evidence based guidelines from Japan[J]. World J Gastroenterol, 2006, 12(5): 828-9. [https://doi.org/10.3748/wjg.v12.i5.828.]
Zheng J, Dong J. Practice guideline for diagnosis and treatment of bile duct injury (2013 edition). Zhonghua Xiaohua Waike Zazhi. 2013,12:81–95. [https://doi.org/10.3760/cma.j.issn.1673-9752.2013.02.001.]
Acknowledgements
We thank Dr. Baosong Zhou for helping with reviewing the statistical methods of this study.
Funding
This work was supported by the National Natural Science Foundation of China [No. 81974370 and 81773184 to J.W., No. 81402472 to W.W.] and Shanghai Outstanding Academic Leaders Plan [No. 2016 to J.W.].
Author information
Authors and Affiliations
Contributions
(I) Conception and design: Jian Wang and Wei Wang. (II) Administrative support: Jian Wang. (III) Provision of study materials or patients: Jian Wang and Wei Wang. (IV) Collection and assembly of data: all authors. (V) Data analysis and interpretation: Wei Wang and Chuanxin Yang. (VI) Manuscript writing: all authors. (VII) Final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Shanghai Sixth People's Hospital Affiliated to Shanghai Jiao Tong University School of Medicine (registration number: 2022-KY-001), and individual consent for this retrospective analysis was waived.
Conflict of Interest
All authors have completed the ICMJE uniform disclosure form. The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

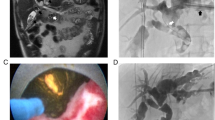
Supplementary Figure 1
LHO classification system and surgical strategy. The new classification consists of three aspects: the L type, lesions of the liver (stones and hepatic atrophy); the H type, lesions of the hilar bile duct (stones and strictures); and the O type, condition of the Oddi sphincter (relaxation or strictures). Through the evaluation of the above elements, each patient can be assigned an individual LHO type and a corresponding surgical strategy. (PNG 17 kb)

Supplementary Figure 1
Inclusion and exclusion criteria. (PNG 18 kb)
Supplementary Tables 1–3
(DOCX 22 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, W., Yang, C., Wang, J. et al. Hepatolithiasis Classification Based on Anatomical Hepatectomy. J Gastrointest Surg 27, 914–925 (2023). https://doi.org/10.1007/s11605-022-05572-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05572-x