Summary
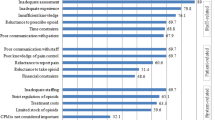
This cross-sectional study aimed to investigate cancer patients’ cognitive level of pain control and to evaluate the patient-related factors or barriers to effective cancer pain management in China. In seven tertiary hospitals across China, 372 patients experiencing cancer pain were surveyed through a self-designed questionnaire to assess the factors associated with effective pain control. Patients’ demographic data and pain control-related factors were recorded. Cluster sampling and binary logistic regression models were used to investigate the association between predictive factors and effective pain control. The survey showed that the majority of the patients were more than 45 years old (76.3%), and 64.4% had an average annual income of more than 20 000 RMB. One-third of the patients suffered from cancer pain for more than 3 months, and 75.1% received professional guidance during medication. The barriers to pain control for patients included preference to enduring pain and refusing analgesics (62.9%), negligence towards drug usage (28.5%), concerns about the addiction (48.2%) and adverse reaction (56.4%). The average annual family income, professional guidance, knowledge of pain medication, adherence to analgesics, and concerns about addiction to analgesics were significantly correlated to the effect of patients’ pain control. The study presents major barriers to optimal pain control among patients with cancer in China. Our findings suggest that educational programs and medical insurance reimbursement support from the government are urgently needed to overcome the cognitive barriers toward effective pain management and to relieve the economic burden among patients with cancer pain in China.
Similar content being viewed by others
References
van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol, 2007,18(9):1437–1449
van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, et al. Update on prevalence of pain in patients with cancer: Systematic review and meta-analysis. J Pain Symptom Manage, 2016,51(6):1070–1090
Inoue S, Kobayashi F, Nishihara M, et al. Chronic pain in the Japanese community-prevalence, characteristics and impact on quality of life. PLoS One, 2015,10(6):e0129262
Rau KM, Chen JS, Wu HB, et al. The impact of pain control on physical and psychiatric functions of cancer patients: a nation-wide survey in Taiwan. Jpn J Clin Oncol, 2015,45(11):1042–1049
Knaul FM, Farmer PE, Krakauer EL, et al. Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: the Lancet Commission report. Lancet, 2018,391(10128):1391–1454
Cancer pain relief. Geneva: World Health Organization; 1986.
Gao W, Gulliford M, Bennett MI, et al. Managing cancer pain at the end of life with multiple strong opioids: a population-based retrospective cohort study in primary care. PLoS One, 2014,9(1):e79266
Caraceni A, Hanks G, Kaasa S, et al. Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol, 2012,13(2):58–68
Jara C, Del Barco S, Grávalos C, et al. SEOM clinical guideline for treatment of cancer pain (2017). Clin Transl Oncol, 2018,20(1):97–107
Lara-Solares A, Ahumada Olea M, Basantes Pinos ALÁ, et al. Latin-American guidelines for cancer pain management. Pain Manag, 2017,7(4):287–298
Swarm RA, Paice JA, Anghelescu DL, et al. Adult Cancer Pain, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw, 2019,17(8):977–1007
Shute C. The challenges of cancer pain assessment and management. Ulster Med J, 2013,82(1):40–42
Mack KA, Jones CM, Ballesteros MF. Illicit Drug Use, Illicit Drug Use Disorders, and Drug Overdose Deaths in Metropolitan and Nonmetropolitan Areas-United States. Am J Transplant, 2017,17(12):3241–3252
Hamieh NM, Akel R, Anouti B, et al. Cancer-Related Pain: Prevalence, Severity and Management in a Tertiary Care Center in the Middle East. Asian Pac J Cancer Prev, 2018,19(3):769–775
Vuong S, Pulenzas N, DeAngelis C, et al. Inadequate pain management in cancer patients attending an outpatient palliative radiotherapy clinic. Support Care Cancer, 2016,24(2):887–892
Shen WC, Chen JS, Shao YY, et al. Impact of Undertreatment of Cancer Pain with Analgesic Drugs on Patient Outcomes: A Nationwide Survey of Outpatient Cancer Patient Care in Taiwan. J Pain Symptom Manage, 2017,54(1):55–65
Greco MT, Roberto A, Corli O, et al. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol, 2014,32(36):4149–4154
Sharkey L, Loring B, Cowan M, et al. National palliative care capacities around the world: results from the World Health Organization Noncom-municable Disease Country Capacity Survey. Palliat Med, 2018,32:106–113
Ministry of Health of the People’s Republic of China. Norms for cancer pain treatment, 2011. http://www.moh.gov.cn/mohyzs/s3585/201112/53838.
Xia Z. Cancer pain management in China: current status and practice implications based on the ACHEON survey. J Pain Res, 2017,10:1943–1952
Jamison RN, Sheehan KA, Scanlan E, et al. Beliefs and attitudes about opioid prescribing and chronic pain management: survey of primary care providers. J Opioid Manag, 2014,10(6):375–382
Alnajar MK, Darawad MW, Alshahwan SS, et al. Knowledge and Attitudes Toward Cancer Pain Management Among Nurses at Oncology Units. J Cancer Educ, 2019,34(1):186–193
Gunnarsdottir S, Donovan HS, Serlin RC, et al. Patient-related barriers to pain management: the Barriers Questionnaire II (BQ-II). Pain, 2002,99(3):385–396
Potter VT, Wiseman CE, Dunn SM, et al. Patient barriers to optimal cancer pain control. Psychooncology, 2003,12(2):153–160
Konstantis A, Exiara T. Family caregiver beliefs and barriers to effective pain management of cancer patients in home care settings. J BUON, 2018,23(7):144–152
Lee BO, Liu Y, Wang YH, et al. Mediating effect of family caregivers’ hesitancy to use analgesics on homecare cancer patients’ analgesic adherence. J Pain Symptom Manag, 2015,50(6):814–821
Wang NY, Liu YM, Zhao HJ, et al. The treatment effect analysis of related factors effecting chronic pain patients with moderately sever pain. Chin J Clin Oncol, 2014,41(10):655–658
Yanjun S, Changli W, Ling W, et al. A survey on physician knowledge and attitudes towards clinical use of morphine for cancer pain treatment in China. Support Care Cancer, 2010,18(11):1455–1460
Liu W, Xie S, Yue L, et al. Investigation and analysis of oncologists’ knowledge of morphine usage in cancer pain treatment. Onco Targets Ther, 2014,7:729–737
Zhang Q, Yu C, Feng S, et al. Physicians’ Practice, Attitudes Toward, and Knowledge of Cancer Pain Management in China. Pain Med, 2015,16(11):2195–203
Robinson JP, Dansie EJ, Wilson HD, et al. Attitudes and Beliefs of Working and WorkDisabled People with Chronic Pain Prescribed Long-Term Opioids. Pain Med, 2015,16(7):1311–1324
Cleary J, Powell RA, Munene G, et al. Formulary availability and regulatory barriers to accessibility of opioids for cancer pain in Africa: a report from the Global Opioid Policy Initiative (GOPI). Ann Oncol, 2013,24(Suppl 11):xi14–xi23
Liang SY, Chen KP, Tsay SL, et al. Relationship between belief about analgesics, analgesic adherence and pain experience in taiwanese cancer outpatients. Asian Pac J Cancer Prev, 2013,14(2):713–716
Al-Atiyyat NMH, Vallerand AH. Patient-related attitudinal barriers to cancer pain management among adult Jordanian patients. Eur J Oncol Nurs, 2018,33:56–61
Oldenmenger WH, Smitt PAS, van Dooren S, et al. A systematic review on barriers hindering adequate cancer pain management and interventions to reduce them: a critical appraisal. Eur J Cancer, 2009,45(8):1370–1380
Meghani SH, Thompson AM, Chittams J, et al. Adherence to analgesics for cancer pain: a comparative study of African Americans and Whites using an electronic monitoring device. J Pain, 2015,16(9):825–835
Wang Z, Chang R, Luo Y B, et al. Evaluation of Need and Distribution of National Essential Medicines List in Village Clinics: A Cross-sectional Study Based on the Perspective of Village Doctors in China. Curr Med Sci, 2019,39(4):663–669
Gunnarsdottir S, Serlin RC, Ward S. Patient-related barriers to pain management: the icelandic barriers questionnaire II. J Pain Symptom Manag, 2005,29(3):273–285
Gunnarsdottir S, Sigurdardottir V, Kloke M, et al. A multicenter study of attitudinal barriers to cancer pain management. Support Care Cancer, 2017,25(11):3595–3602
Tzeng JI, Chang CC, Chang HJ, et al. Assessing analgesic regimen adherence with the Morisky Medication Adherence Measure for Taiwanese patients with cancer pain. J Pain Symptom Manag, 2008,36(2):157–166
Chou WC, Chen JS, Hung CY, et al. A nationwide survey of adherence to analgesic drugs among cancer patients in Taiwan: prevalence, determinants, and impact on quality of life. Support Care Cancer, 2019,27(8):2857–2867
Im EO, Liu Y, Kim YH, et al. Asian American cancer patients’ pain experience. Cancer Nurs, 2008,31(3):E17–E23
Kim YC, Ahn JS, Calimag MMP, et al. Current practices in cancer pain management in Asia: a survey of patients and physicians across 10 countries. Cancer Med, 2015,4(8):1196–1204
Green CR, Hart- Johnson T. The adequacy of chronic pain management prior to presenting at a tertiary care pain center: the role of patient socio-demographic characteristics. J Pain, 2010,11(8):746–754
Lou F, Shang S. Attitudes towards pain management in hospitalized cancer patients and their influencing factors. Chin J Cancer Res, 2017,29(1):75–85
Xu X, Ou M, Xie C, et al. Pain Acceptance and Its Associated Factors among Cancer Patients in Mainland China: A Cross-Sectional Study. Pain Res Manag, 2019,2019:9458683
Jacobsen R, Moldrup C, Christrup C, et al. Patient-related barriers to cancer pain management: a systematic exploratory review. Scand J Caring Sci, 2009,23:190–208
Zeng D, Li K, Lin X, et al. Attitudinal Barriers to Pain Management and Associated Factors Among Cancer Patients in Mainland China: Implications for Cancer Education. J Cancer Educ, 2020,35(2):284–291
Rustoen T, Valeberg BT, Kolstad E, et al. The PRO-SELF((c)) Pain Control Program improves patients’ knowledge of cancer pain management. J Pain Symptom Manage, 2012,44(3):321–330
Adam R, Bond C, Murchie P. Educational interventions for cancer pain. A systematic review of systematic reviews with nested narrative review of randomized controlled trials. Patient Educ Couns, 2015,98(3):269–282
Padrnos L, Bennett R, Kosiorek H, et al. Living with Cancer: an Educational Intervention in Cancer Patients Can Improve Patient-Reported Knowledge Deficit. J Cancer Educ, 2018,33(3):653–659
Holtzman AL, Williams JP, Hutchinson DF, et al. Improving Patient-reported Pain During Radiotherapy Through Nurse Involvement and Patient Education. Am J Clin Oncol. 2018,41(10):1028–1030
Prevost V, Heutte N, Leconte A, et al. Effectiveness of a therapeutic patient education program in improving cancer pain management: EFFADOL, a stepped-wedge randomised controlled trial. BMC Cancer, 2019,19(1):673
Zhou L, Liu XL, Tan JY, et al. Nurse-led educational interventions on cancer pain outcomes for oncology outpatients: a systematic review. International Nursing Review. Int Nurs Rev, 2015,62(2):218–230
Wang Y, Huang H, Zeng Y, et al. Pharmacist-led medication education in cancer pain control: A multicentre randomized controlled study in Guangzhou, China. J Int Med Res, 2013,41(5):1462–1472
Edwards Z, Ziegler L, Craigs C, et al. Pharmacist educational interventions for cancer pain management: a systematic review and meta-analysis. Int J Pharm Pract, 2019,27(4):336–345
Acknowledgments
The authors would like to acknowledge the seven hospitals for their support to the project. We also thank all cancer patients who devoted their time to participate in this study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The authors declare that they have no conflict of interest.
Additional information
This work was financially supported by Hubei Provincial Natural Science Foundation of China (No. 2016CFB678).
Rights and permissions
About this article
Cite this article
Shangguan, Xf., Yu, Zq., Ji, L. et al. Cognition and Sociodemographic Determinants for Effective Pain Control in Patients with Cancer Pain: a Cross-sectional Survey in China. CURR MED SCI 40, 249–256 (2020). https://doi.org/10.1007/s11596-020-2167-3
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-020-2167-3