Abstract
Purpose
To compare point shear wave elastography (pSWE, ElastPQ®) and transient elastography (TE) with Liver Biopsy in order to evaluate fibrosis stage in non-alcoholic fatty liver disease (NAFLD).
Methods
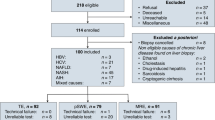
Our prospective study from September 2017 to October 2020 included 50 consecutively enrolled patients with NAFLD (52.2 ± 13.0 years, 32 male). All patients underwent clinical evaluation, B-mode ultrasound, pSWE, TE and liver biopsy in a single evaluation. The clinical, laboratory and liver biopsy data were compared with liver stiffness (LS) measurement obtained with pSWE and TE. TE and pSWE diagnostic accuracy for the diagnosis of the different fibrosis stages were evaluated using the area under receiver operating characteristic curve (AUROC).
Results
Only fibrosis stage was independently associated with TE and pSWE. The median liver stiffness measurement for fibrosis stages F0, F1, F2, F3, and F4 using TE was 4.8 (4.7–6.1) kPa, 5.5 (4.4–7.3) kPa, 7.7 (6.1–9.1) kPa, 9.9 (8.8–13.8) kPa, and 20.2 kPa, respectively. The corresponding median liver stiffness measurement using pSWE was 4.2 (4.0–4.8) kPa, 4.7 (4.2–5.8) kPa, 5.1 (4.1–6.9) kPa, 8.5 (5.2–13.3), and 15.1 kPa, respectively. The AUROC of TE for diagnosis of fibrosis stage F1, ≥ F2, ≥ F3, and F4 were 0.795, 0.867, 0.927, and 0.990, respectively. The corresponding AUROC of pSWE was 0.717, 0.733, 0.908, and 1.000, respectively. No association was observed with other histological parameters.
Conclusion
TE was significantly better than pSWE for the diagnosis of fibrosis stage ≥ F2. No statistically significant differences were found between TE and pSWE AUROC of fibrosis stage ≥ F1, ≥ F3, and F4.




Similar content being viewed by others
References
Younossi ZM, Koenig AB (2016) Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64:73–84. https://doi.org/10.1002/hep.28431
Loomba R, Sanyal AJ (2013) The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol (N Y) 350:1–5. https://doi.org/10.1038/nrgastro.2013.171
Bedogni G, Miglioli L (2005) Prevalence of and risk factors for nonalcoholic fatty liver disease: the dionysos nutrition and liver study. Hepatology 42:44–52. https://doi.org/10.1002/hep.20734
Araújo AR, Rosso N, Bedogni G et al (2018) Global epidemiology of non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: what we need in the future. Liver Int 38:47–51. https://doi.org/10.1111/liv.13643
Gunn NT, Shiffman ML (2018) The use of liver biopsy in nonalcoholic fatty liver disease: when to biopsy and in whom. Clin Liver Dis 22:109–119. https://doi.org/10.1016/j.cld.2017.08.006
Piccinino F, Sangelli F (1986) Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol 2(2):165–173. https://doi.org/10.1016/s0168-8278(86)80075-7
European Association for the Study of the Liver (EASL), The SEA for, Diabetes (EASD) of, Obesity (EASO) European Association for the Study of EASL–EASD–EASO (2016) Clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 64:1388–1402. https://doi.org/10.1016/j.jhep.2015.11.004
Cosgrove D, Piscaglia F, Bamber J et al (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: clinical applications. Ultraschall Med 34:238–253
Dietrich CF, Bamber J et al (2017) EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, update 2017 (Long Version). Ultraschall Med 2017:16–47
Argalia G, Tarantino G, Ventura C et al (2021) Shear wave elastography and transient elastography in HCV patients after direct—acting antivirals. Radiol Med 126(6):894–899. https://doi.org/10.1007/s11547-020-01326-4
Leong WL, Lai LL, Raihan N et al (2019) Comparing point shear wave elastography (ElastPQ) and transient elastography for diagnosis of fi brosis stage in non- alcoholic fatty liver disease. J Gastroenterol Hepatol. https://doi.org/10.1111/jgh.14782
Shen FF, Lu LG (2016) Advances in noninvasive methods for diagnosing nonalcoholic fatty liver disease. J Dig Dis. https://doi.org/10.1111/1751-2980.12384
Boursier J, Zarski JP, de Ledinghen V et al (2013) Multicentric group from ANRS/HC/EP23 FIBROSTAR studies. Determination of reliability criteria for liver stiffness evaluation by transient elastography. Hepatology 57(3):1182–1191. https://doi.org/10.1002/hep.25993
Ferraioli G, Parekh P, Levitov AB, Filice C (2014) Shear wave elastography for evaluation of liver fibrosis. J Ultrasound Med 33:197–203. https://doi.org/10.7863/ultra.33.2.197
Schiano TD, Azeem S, Bodian CA et al (2005) Importance of specimen size in accurate needle liver biopsy evaluation of patients with chronic hepatitis C. Clin Gastroenterol Hepatol 3:930–935. https://doi.org/10.1016/S1542-3565(05)00541-0
Kleiner DE, Brunt EM, Van NM et al (2005) Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41:1313–1321. https://doi.org/10.1002/hep.20701
Ferraioli G, De Silvestri A, Reiberger T et al (2018) Adherence to quality criteria improves concordance between transient elastography and ElastPQ for liver stiffness assessment—A multicenter retrospective study. Dig Liver Dis 50:1056–1061. https://doi.org/10.1016/j.dld.2018.03.033
Lee MS, Bae JM, Joo SK et al (2018) Correction: prospective comparison among transient elastography, supersonic shear imaging, and ARFI imaging for predicting fibrosis in nonalcoholic fatty liver disease. PLoS ONE 13:1–17. https://doi.org/10.1371/journal.pone.0200055
Cassinotto C, Boursier J, de Lédinghen V et al (2016) Liver stiffness in nonalcoholic fatty liver disease: a comparison of supersonic shear imaging, FibroScan, and ARFI with liver biopsy. Hepatology 63:1817–1827. https://doi.org/10.1002/hep.28394
Friedrich-Rust M, Romen D, Vermehren J et al (2012) Acoustic radiation force impulse-imaging and transient elastography for non-invasive assessment of liver fibrosis and steatosis in NAFLD. Eur J Radiol 81:325–331. https://doi.org/10.1016/j.ejrad.2011.10.029
Attia D, Bantel H, Lenzen H et al (2016) Liver stiffness measurement using acoustic radiation force impulse elastography in overweight and obese patients. Aliment Pharmacol Ther 44:366–379. https://doi.org/10.1111/apt.13710
Lefebvre T, Wartelle-Bladou C, Wong P et al (2019) Prospective comparison of transient, point shear wave, and magnetic resonance elastography for staging liver fibrosis. Eur Radiol 29:6477–6488. https://doi.org/10.1007/s00330-019-06331-4
Selvaraj EA, Mózes FE, Jayaswal ANA et al (2021) Diagnostic accuracy of elastography and magnetic resonance imaging in patients with NAFLD: a systematic review and meta-analysis. J Hepatol 75:770–785. https://doi.org/10.1016/j.jhep.2021.04.044
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
GA, GSB, and AG conceived the study. CV, NT, DC, MT, and MC were involved in data collection. CT analysed data. GA, GSB, CV and NT interpreted data. CV, NT were the major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interests associated with this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Argalia, G., Ventura, C., Tosi, N. et al. Comparison of point shear wave elastography and transient elastography in the evaluation of patients with NAFLD. Radiol med 127, 571–576 (2022). https://doi.org/10.1007/s11547-022-01475-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01475-8