Abstract
The stent implantation may alter the post-operative patient’s blood pressure, and bioresorbable vascular stents (BVS) as a candidate to treat vascular diseases, its degradation is affected by mechanical stress, thus, the altered pressure representing varying stress level will result in different degradation behaviors of the BVS. This paper first proposed a novel stress-regulated PLA degradation model that included swelling factor, and then the degradation evolutions of a PLA BVS within 180 days under normal and high blood pressures were simulated by finite element method, and more four degradation indexes were defined to study the effects of the two blood pressures on the degradation of the PLA BVS. The results showed that the high pressure weakly accelerated the degradation of the PLA BVS with respect to the normal pressure by examining the four indexes, e.g., the residual stent volume \({v}_{r}(t)\) decreased to 0.72 and 0.69, respectively for the normal and high pressures at day 180. The current finding provided a theoretical understanding of the PLA BVS degradation, and hinted that the PLA BVS may not need to be elaborately selected in clinical practices for treating hypertensive patients.
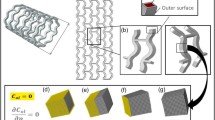
Graphical abstract








Similar content being viewed by others
References
Amirjani A, Yousefi M, Cheshmaroo M (2014) Parametrical optimization of stent design; a numerical-based approach. Comput Mater Sci 90:210–220. https://doi.org/10.1016/j.commatsci.2014.04.002
Hermawan H, Dube D, Mantovani D (2010) Developments in metallic biodegradable stents. Acta Biomater 6(5):1693–1697. https://doi.org/10.1016/j.actbio.2009.10.006
Li N, Zhang H, Ouyang H (2009) Shape optimization of coronary artery stent based on a parametric model. Finite Elem Anal Des 45(6–7):468–475. https://doi.org/10.1016/j.finel.2009.01.001
Boland EL, Shine R, Kelly N et al (2016) A review of material degradation modelling for the analysis and design of bioabsorbable stents. Ann Biomed Eng 44(2):341–356. https://doi.org/10.1007/s10439-015-1413-5
Singh R, Bathaei MJ, Istif E et al (2020) A review of bioresorbable implantable medical devices: materials, fabrication, and implementation. Adv Healthc Mater 9(18):e2000790. https://doi.org/10.1002/adhm.202000790
Park H, Hong YJ, Cho JY et al (2017) Blood pressure targets and clinical outcomes in patients with acute myocardial infarction. Korean Circ J 47(4):446–454. https://doi.org/10.4070/kcj.2017.0008
Tsai TY, Leu HB, Hsu PF et al (2022) Association between visit-to-visit blood pressure variability and adverse events in coronary artery disease patients after coronary intervention. J Clin Hypertens 24(10):1327–1338. https://doi.org/10.1111/jch.14565
Rosendorff C, Lackland DT, Allison M et al (2015) Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. Circulation 131(19):e435-470. https://doi.org/10.1161/CIR.0000000000000207
Lee CW, Lee JK, Choi YJ et al (2022) Blood pressure and mortality after percutaneous coronary intervention: a population-based cohort study. Sci Rep 12(1):2768. https://doi.org/10.1038/s41598-022-06627-4
Clark D, Nicholls SJ, St John J et al (2019) Visit-to-visit blood pressure variability, coronary atheroma progression, and clinical outcomes. JAMA Cardiol 4(5):437–443. https://doi.org/10.1001/jamacardio.2019.0751
Chen H, Shi Q, Shui H et al (2021) Degradation of 3D-printed porous polylactic acid scaffolds under mechanical stimulus. Front Bioeng Biotechnol 9:691834. https://doi.org/10.3389/fbioe.2021.691834
Shi Q, Chen Q, Pugno N et al (2018) Effect of rehabilitation exercise durations on the dynamic bone repair process by coupling polymer scaffold degradation and bone formation. Biomech Model Mechanobiol 17(3):763–775. https://doi.org/10.1007/s10237-017-0991-6
Shui H, Shi Q, Pugno NM et al (2019) Effect of mechanical stimulation on the degradation of poly(lactic acid) scaffolds with different designed structures. J Mech Behav Biomed Mater 96:324–333. https://doi.org/10.1016/j.jmbbm.2019.04.028
Li X, Chu C, Wei Y et al (2017) In vitro degradation kinetics of pure PLA and Mg/PLA composite: effects of immersion temperature and compression stress. Acta Biomater 48:468–478. https://doi.org/10.1016/j.actbio.2016.11.001
Wu Z, Wang L, Fan Y (2023) Effect of static tensile stress on enzymatic degradation of poly(glycerol sebacate). J Biomed Mater Res A. https://doi.org/10.1002/jbm.a.37550
Han XX, Pan JZ (2009) A model for simultaneous crystallisation and biodegradation of biodegradable polymers. Biomaterials 30(3):423–430. https://doi.org/10.1016/j.biomaterials.2008.10.001
Beyer MK, Clausen-Schaumann H (2005) Mechanochemistry: The mechanical activation of covalent bonds. Chem Rev 105(8):2921–2948. https://doi.org/10.1021/cr030697h
Gong Y, Zhou Q, Gao C et al (2007) In vitro and in vivo degradability and cytocompatibility of poly(l-lactic acid) scaffold fabricated by a gelatin particle leaching method. Acta Biomater 3(4):531–540. https://doi.org/10.1016/j.actbio.2006.12.008
Liu G, Zhang X, Wang D (2014) Tailoring crystallization: towards high-performance poly(lactic acid). Adv Mater 26(40):6905–6911. https://doi.org/10.1002/adma.201305413
Zolnik BS, Burgess DJ (2007) Effect of acidic pH on PLGA microsphere degradation and release. J Control Release 122(3):338–344. https://doi.org/10.1016/j.jconrel.2007.05.034
Bode C, Kranz H, Fivez A et al (2019) Often neglected: PLGA/PLA swelling orchestrates drug release: HME implants. J Control Release 306:97–107. https://doi.org/10.1016/j.jconrel.2019.05.039
Gopferich A, Langer R (1993) Modeling of polymer erosion. Macromolecules 26:4105–4112. https://doi.org/10.1021/ma00068a006
Ebrahimi-Nozari T, Imani R, Haghbin-Nazarpak M et al (2023) Multimodal effects of asymmetric coating of coronary stents by electrospinning and electrophoretic deposition. Int J Pharm 630:122437. https://doi.org/10.1016/j.ijpharm.2022.122437
Iñiguez-Franco F, Auras R, Burgess G et al (2016) Concurrent solvent induced crystallization and hydrolytic degradation of PLA by water-ethanol solutions. Polymer 99:315–323. https://doi.org/10.1016/j.polymer.2016.07.018
Bose SM, Git Y (2004) Mathematical modelling and computer simulation of linear polymer degradation: simple scissions. Macromol Theor Simul 13(5):453–473. https://doi.org/10.1002/mats.200300036
Thombre AG, Himmelstein KJ (1985) A simultaneous transport-reaction model for controlled drug delivery from catalyzed bioerodible polymer matrices. AIChE J 31(5):759–766. https://doi.org/10.1002/aic.690310509
Chen Y, Zhou S, Li Q (2011) Mathematical modeling of degradation for bulk-erosive polymers: applications in tissue engineering scaffolds and drug delivery systems. Acta Biomater 7(3):1140–1149. https://doi.org/10.1016/j.actbio.2010.09.038
Vieira AC, Vieira JC, Ferra JM et al (2011) Mechanical study of PLA-PCL fibers during in vitro degradation. J Mech Behav Biomed Mater 4(3):451–460. https://doi.org/10.1016/j.jmbbm.2010.12.006
Zhang H, Du T, Chen S et al (2022) Finite element analysis of the non-uniform degradation of biodegradable vascular stents. J Funct Biomater 13(3):152. https://doi.org/10.3390/jfb13030152
Gao YM, Wang LZ, Gu XN et al (2018) A quantitative study on magnesium alloy stent biodegradation. J Biomech 74:98–105. https://doi.org/10.1016/j.jbiomech.2018.04.027
Resnick N, Yahav H, Shay-Salit A et al (2003) Fluid shear stress and the vascular endothelium: for better and for worse. Prog Biophys Molecul Biol 81(3):177–199. https://doi.org/10.1016/S0079-6107(02)00052-4
Proikakis CS, Mamouzelos NJ, Tarantili PA et al (2006) Swelling and hydrolytic degradation of poly(d, l-lactic acid) in aqueous solutions. Polym Degrad Stab 91(3):614–619. https://doi.org/10.1016/j.polymdegradstab.2005.01.060
David Chua SN, Mac Donald BJ, Hashmi MSJ (2003) Finite element simulation of stent and balloon interaction. J Mater Process Tech 143–144:591–597. https://doi.org/10.1016/s0924-0136(03)00435-7
Grabow N, Schlun M, Sternberg K et al (2005) Mechanical properties of laser cut poly(L-lactide) micro-specimens: implications for stent design, manufacture, and sterilization. J Biomech Eng-T ASME 127(1):25–31. https://doi.org/10.1115/1.1835349
Dumitru AC, Espinosa FM, Garcia R et al (2015) In situ nanomechanical characterization of the early stages of swelling and degradation of a biodegradable polymer. Nanoscale 7(12):5403–5410. https://doi.org/10.1039/c5nr00265f
Khalaj Amnieh S, Mashayekhi M, Shahnooshi E et al (2021) Biodegradable performance of PLA stents affected by geometrical parameters: the risk of fracture and fragment separation. J Biomech 122:110489. https://doi.org/10.1016/j.jbiomech.2021.110489
Guo M, Chu Z, Yao J et al (2016) The effects of tensile stress on degradation of biodegradable PLGA membranes: a quantitative study. Polym Degrad Stabil 124:95–100. https://doi.org/10.1016/j.polymdegradstab.2015.12.019
Cui X, Peng K, Liu S et al (2019) A computational modelling of the mechanical performance of a bioabsorbable stent undergoing cyclic loading. Procedia Struct Integr 15:67–74. https://doi.org/10.1016/j.prostr.2019.07.013
Lin S, Dong P, Zhou C et al (2020) Degradation modeling of poly-l-lactide acid (PLLA) bioresorbable vascular scaffold within a coronary artery. Nanotechnol Rev 9(1):1217–1226. https://doi.org/10.1515/ntrev-2020-0093
Li Y, Chu Z, Li X et al (2017) The effect of mechanical loads on the degradation of aliphatic biodegradable polyesters. Regen Biomater 4(3):179–190. https://doi.org/10.1093/rb/rbx009
Li X, Yu W, Han L et al (2019) Degradation behaviors of Mg alloy wires/PLA composite in the consistent and staged dynamic environments. Mater Sci Eng C Mater Biol Appl 103:109765. https://doi.org/10.1016/j.msec.2019.109765
Li X, Qi C, Han L et al (2017) Influence of dynamic compressive loading on the in vitro degradation behavior of pure PLA and Mg/PLA composite. Acta Biomater 64:269–278. https://doi.org/10.1016/j.actbio.2017.08.004
Liu L, Shi Q, Chen Q et al (2019) Mathematical modeling of bone in-growth into undegradable porous periodic scaffolds under mechanical stimulus. J Tissue Eng 10:2041731419827167. https://doi.org/10.1177/2041731419827167
Acknowledgements
The authors thank the School of Civil Engineering of Southeast University for the commercial software ABAQUS.
Funding
The research was supported by the National Natural Science Foundation of China (32171307, 12372307, 61821002, 12172089) and ARC (DP200103492).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
He, S., Liu, W., Wei, L. et al. A phenomenological model of pulsatile blood pressure-affected degradation of polylactic acid (PLA) vascular stent. Med Biol Eng Comput 62, 1347–1359 (2024). https://doi.org/10.1007/s11517-023-02998-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-023-02998-6