Abstract
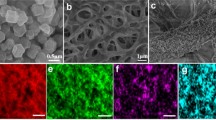
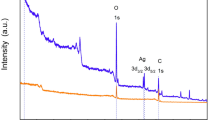
In the tissue remodeling stage of burns, excessive medical therapy can cause scarring by promoting excessive fibroblast proliferation and collagen deposition. Cold atmospheric plasma (CAP) has emerged in biomedicine for its excellent sterilization and wound-healing function, which is expected to reduce the use of drugs in burns treatment. Here, a novel therapy that could rapidly heal burns was developed using a combined self-adaption release system with CAP. The self-adaption release system (Cur-ZIF8@HA) used curcumin (Cur) as the therapeutic drug and ZIF-8 modified with hyaluronic acid (HA) as the carrier. In vitro study results showed that combined treatment methods can inactivate bacteria and enhance fibroblast cells’ migration and proliferation. In vivo animal wound healing studies have demonstrated that the synergistic treatment of Cur-ZIF8@HA and CAP can help fibroblast proliferation and stimulate angiogenesis, indicating effective wound healing. More importantly, CAP can reduce collagen synthesis in granulation tissue recombination and further inhibit scar formation by combining with Cur-ZIF8@HA. In the biomedical field, these findings underscore to a large extent that our research will open up new possibilities for the interaction of nanotechnology with new technologies of physical principles.
Similar content being viewed by others
References
Uberoi A, Bartow-McKenney C, Zheng Q, et al. Commensal micro-biota regulates skin barrier function and repair via signaling through the aryl hydrocarbon receptor. Cell Host Microbe, 2021, 29: 1235–1248.e8
Woodby B, Penta K, Pecorelli A, et al. Skin health from the inside out. Annu Rev Food Sci Technol, 2020, 11: 235–254
Mata I R, Mata S R, Menezes R C R, et al. Benefits of turmeric supplementation for skin health in chronic diseases: A systematic review. Crit Rev Food Sci Nutr, 2021, 61: 3421–3435
Lachiewicz A M, Hauck C G, Weber D J, et al. Bacterial infections after burn injuries: Impact of multidrug resistance. Clin Infect Dis, 2017, 65: 2130–2136
Nuutila K, Eriksson E. Moist wound healing with commonly available dressings. Adv Wound Care, 2021, 10: 685–698
Ostojic S M. Medical gases as an emerging topic in sports medicine. Sports Med, 2018, 48: 2677–2678
Kaushik N K, Bekeschus S, Tanaka H, et al. Plasma medicine technologies. Appl Sci, 2021, 11: 4584
Gan L, Zhang S, Poorun D, et al. Medical applications of nonthermal atmospheric pressure plasma in dermatology. JDDG-J der Deutschen Dermatol Gesellschaft, 2018, 16: 7–13
Sainz-García A, Toledano P, Muro-Fraguas I, et al. Mask disinfection using atmospheric pressure cold plasma. Int J Infect Dis, 2022, 123: 145–156
Lata S, Chakravorty S, Mitra T, et al. Aurora Borealis in dentistry: The applications of cold plasma in biomedicine. Mater Today Bio, 2022, 13: 100200
Busco G, Robert E, Chettouh-Hammas N, et al. The emerging potential of cold atmospheric plasma in skin biology. Free Radic Biol Med, 2020, 161: 290–304
Dubey S K, Parab S, Alexander A, et al. Cold atmospheric plasma therapy in wound healing. Process Biochem, 2022, 112: 112–123
Chen G, Chen Z, Wang Z, et al. Portable air-fed cold atmospheric plasma device for postsurgical cancer treatment. Sci Adv, 2021, 7: eabg5686
Zhao Y, Zhang Z, Pan Z, et al. Advanced bioactive nanomaterials for biomedical applications. Exploration, 2021, 1: 20210089
Chen Z, Duan J, Diao Y, et al. ROS-responsive capsules engineered from EGCG-Zinc networks improve therapeutic angiogenesis in mouse limb ischemia. Bioact Mater, 2021, 6: 1–11
Rather H A, Thakore R, Singh R, et al. Antioxidative study of cerium oxide nanoparticle functionalised PCL-gelatin electrospun fibers for wound healing application. Bioact Mater, 2018, 3: 201–211
Niethammer P, Grabher C, Look A T, et al. A tissue-scale gradient of hydrogen peroxide mediates rapid wound detection in zebrafish. Nature, 2009, 459: 996–999
Zhang W, Liu Z, Zhu L, et al. Combining micro-plasma radio-frequency with hypofractionated electron-beam radiation as a novel treatment of keloids. Medicine, 2019, 98: e18094
Wang X F, Fang Q Q, Jia B, et al. Potential effect of non-thermal plasma for the inhibition of scar formation: A preliminary report. Sci Rep, 2020, 10: 1064
Govindaraju P, Todd L, Shetye S, et al. CD44-dependent inflammation, fibrogenesis, and collagenolysis regulates extracellular matrix remodeling and tensile strength during cutaneous wound healing. Matrix Biol, 2019, 75–76: 314–330
Chin J S, Madden L, Chew S Y, et al. Drug therapies and delivery mechanisms to treat perturbed skin wound healing. Adv Drug Deliv Rev, 2019, 149–150: 2–18
Jeschke M G, van Baar M E, Choudhry M A, et al. Burn injury. Nat Rev Dis Primers, 2020, 6: 11
Friedrich E E, Washburn N R. Transport patterns of anti-TNF-α in burn wounds: Therapeutic implications of hyaluronic acid conjugation. Biomaterials, 2017, 114: 10–22
Gragnani A, Tonarelli E, Chomiski V, et al. Fibroblast growth factor in the treatment of burns: A systematic review. Burns, 2022, 48: 104–110
Li Z, Huang X, Lin L, et al. Polyphenol and Cu2+ surface-modified chitin sponge synergizes with antibacterial, antioxidant and pro-vascularization activities for effective scarless regeneration of burned skin. Chem Eng J, 2021, 419: 129488
Lu Y, Li H, Wang J, et al. Engineering bacteria-activated multi-functionalized hydrogel for promoting diabetic wound healing. Adv Funct Mater, 2021, 31: 2105749
Han Y, Huang K, Yao Q P, et al. Mechanobiology in vascular remodeling. Natl Sci Rev, 2018, 5: 933–946
Jiang D, Scharffetter-Kochanek K. Mesenchymal stem cells adaptively respond to environmental cues thereby improving granulation tissue formation and wound healing. Front Cell Dev Biol, 2020, 8: 697
Seo C H, Cui H S, Kim J B. Calpastatin-mediated inhibition of calpain ameliorates skin scar formation after burn injury. Int J Mol Sci, 2021, 22: 5771
Shook B A, Wasko R R, Rivera-Gonzalez G C, et al. Myofibroblast proliferation and heterogeneity are supported by macrophages during skin repair. Science, 2018, 362: eaar2971
Qu J, Zhao X, Liang Y, et al. Degradable conductive injectable hydrogels as novel antibacterial, anti-oxidant wound dressings for wound healing. Chem Eng J, 2019, 362: 548–560
Shen Y, Xu G, Huang H, et al. Sequential release of small extracellular vesicles from bilayered thiolated alginate/polyethylene glycol diacrylate hydrogels for scarless wound healing. ACS Nano, 2021, 15: 6352–6368
Li W, Yu H, Ding D, et al. Cold atmospheric plasma and iron oxide-based magnetic nanoparticles for synergetic lung cancer therapy. Free Radic Biol Med, 2019, 130: 71–81
Mamidi N, Romo I L, Barrera E V, et al. High throughput fabrication of curcumin embedded gelatin-polylactic acid forcespun fiber-aligned scaffolds for the controlled release of curcumin. MRS Commun, 2018, 8: 1395–1403
Dai L, Li R, Wei Y, et al. Fabrication of zein and rhamnolipid complex nanoparticles to enhance the stability and in vitro release of curcumin. Food Hydrocolloids, 2018, 77: 617–628
Yu J Y, Kim J A, Joung H J, et al. Preparation and characterization of curcumin solid dispersion using HPMC. J Food Sci, 2020, 85: 3866–3873
Wang S, Zhang S. Study on the structure activity relationship of ZIF-8 synthesis and thermal stability. J Inorg Organomet Polym, 2017, 27: 1317–1322
Karimi A, Khataee A, Vatanpour V, et al. High-flux PVDF mixed matrix membranes embedded with size-controlled ZIF-8 nano-particles. Sep Purif Tech, 2019, 229: 115838
Li H, Xue Y, Jia B, et al. The preparation of hyaluronic acid grafted pullulan polymers and their use in the formation of novel biocompatible wound healing film. Carbohydr Polym, 2018, 188: 92–100
Duan S, Zhao X, Su Z, et al. Layer-by-layer decorated nanoscale ZIF-8 with high curcumin loading effectively inactivates gram-negative and gram-positive bacteria. ACS Appl Bio Mater, 2020, 3: 3673–3680
Hasse S, Duong Tran T, Hahn O, et al. Induction of proliferation of basal epidermal keratinocytes by cold atmospheric-pressure plasma. Clin Exp Dermatol, 2016, 41: 202–209
Li X Y, Feng Z, Pu S C, et al. Cold atmospheric plasma jet-generated oxidized derivatives of tryptophan and their selective effects on murine melanoma and fibroblast cells. Plasma Chem Plasma Process, 2018, 38: 919–936
Xu G, Shi X, Cai J, et al. Dual effects of atmospheric pressure plasma jet on skin wound healing of mice. Wound Rep Reg, 2015, 23: 878–884
Wang Z, Hu W, Du Y, et al. Green gas-mediated cross-linking generates biomolecular hydrogels with enhanced strength and excellent hemostasis for wound healing. ACS Appl Mater Interfaces, 2020, 12: 13622–13633
Basha R Y, Sampath Kumar T S, Doble M. Electrospun nanofibers of curdlan (β-1,3 glucan) blend as a potential skin scaffold material. Macromol Mater Eng, 2017, 302: 1600417
Yan Y, Wu R, Bo Y, et al. Induced pluripotent stem cells-derived microvesicles accelerate deep second-degree burn wound healing in mice through miR-16-5p-mediated promotion of keratinocytes migration. Theranostics, 2020, 10: 9970–9983
Gai C, Yu M, Li Z, et al. Acetaminophen sensitizing erastin-induced ferroptosis via modulation of Nrf2/heme oxygenase-1 signaling pathway in non-small-cell lung cancer. J Cell Physiol, 2020, 235: 3329–3339
Shpichka A, Butnaru D, Bezrukov E A, et al. Skin tissue regeneration for burn injury. Stem Cell Res Ther, 2019, 10: 1–6
Ren W, Yan Y, Zeng L, et al. A near infrared light triggered hydro-genated black TiO2 for cancer photothermal therapy. Adv Healthc Mater, 2015, 4: 1526–1536
Author information
Authors and Affiliations
Corresponding authors
Additional information
This work was supported by the National Natural Science Foundation of China (Grant No. 81973671), the Natural Science Foundation of Shandong Province (Grant Nos. ZR2019BB071, ZR2019MC059, ZR2023QH038, and ZR2023MH037), the Traditional Chinese Medicine Science and Technology Project of Shandong Province (Grant Nos. M-2023084 and Q-2023047), and the Science and Technology Innovation Fund for College Students of Weifang Medical University.
Supporting Information
The supporting information is available online at https://tech.scichina.com and https://link.springer.com. The supporting materials are published as submitted, without typesetting or editing. The responsibility for scientific accuracy and content remains entirely with the authors.
Rights and permissions
About this article
Cite this article
Wang, X., Liu, Z., Zhao, L. et al. Synergetic burns treatment by self-adaption release system combined with cold atmospheric plasma. Sci. China Technol. Sci. 66, 2808–2823 (2023). https://doi.org/10.1007/s11431-022-2258-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11431-022-2258-x