Abstract
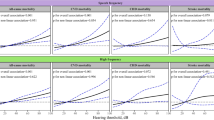
Hearing loss has been associated with increased risk of cardiovascular disease (CVD) prevalence in cross-sectional studies. However, little is known about the prospective association between hearing loss and CVD incidence. We aimed to examine the associations of hearing loss with risk of incident CVD, coronary heart disease (CHD), and stroke in a Chinese population. We included 13,880 individuals aged 63.3 years from the Dongfeng-Tongji cohort study (2013–2018). Hearing loss was categorized into normal, mild, moderate, severe, or greater by the pure-tone average of thresholds at speech and high frequency in both ears. Cox proportional hazard models and linear regression models were used for multivariate longitudinal analyses. After multivariate adjustments, we observed suggestive dose–response associations of increased high-frequency hearing loss with elevated risk of CVD and stroke incidence. Compared with normal hearing loss at high frequency, those with moderate and severe or greater hearing loss had a 4% (95% CI: 0.92, 1.18) or 13% (95% CI: 0.98, 1.30) higher risk of CVD and 52% (95% CI: 1.06, 2.17) or 51% (95% CI: 1.03, 2.20) higher risk of stroke, while the associations were almost consistent across most subgroups. No significant associations were observed for CHD and high-frequency hearing loss, as well as CVD and speech-frequency hearing loss. In addition, higher high-frequency hearing loss was related to unfavorably altered lipid profiles and fasting glucose. Our data suggested that increased hearing loss might increase the risk of incident CVD and stroke among middle-aged and older Chinese, which was partially explained by altered CVD-related biomarkers.

Similar content being viewed by others
Data Availability
No additional data available.
All participants gave written informed content on document approved by the Ethics and Human Subject Committee of Tongji Medical College and Dongfeng General Hospital.
Abbreviations
- BMI:
-
Body mass index
- CHD:
-
Coronary heart disease
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- DMC:
-
Dongfeng Motor Corporation
- HDL-c:
-
High-density lipoprotein cholesterol
- HR:
-
Hazard ratio
- LDL-c:
-
Low-density lipoprotein cholesterol
- MET-h:
-
Metabolic equivalent hours
- MRI:
-
Magnetic resonance imaging
References
Babisch W et al (2005) Traffic noise and risk of myocardial infarction. Epidemiology 16:33–40
Casale M et al (2016) Idiopathic sensorineural hearing loss is associated with endothelial dysfunction. Int J Cardiol Heart Vasc 12:32–33
Causes of Death Collaborators (2018) Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1736–1788
Cho BH et al (2020) Association between body mass index and stroke severity in acute ischaemic stroke with non-valvular atrial fibrillation. Eur J Neurol 27:1672–1679
Curhan SG et al (2013) Body mass index, waist circumference, physical activity, and risk of hearing loss in women. Am J Med 126(1142):e1–e8
Doehner W et al (2013) Overweight and obesity are associated with improved survival, functional outcome, and stroke recurrence after acute stroke or transient ischaemic attack: observations from the TEMPiS trial. Eur Heart J 34:268–277
Dratva J et al (2012) Transportation noise and blood pressure in a population-based sample of adults. Environ Health Perspect 120:50–55
Erickson LC, Newman RS (2017) Influences of background noise on infants and children. Curr Dir Psychol Sci 26:451–457
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A (2001) executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 285:2486–2497
Fang Q et al (2018) Hearing loss is associated with increased CHD risk and unfavorable CHD-related biomarkers in the Dongfeng-Tongji cohort. Atherosclerosis 271:70–76
Fang Q et al (2019) Hearing loss is associated with increased stroke risk in the Dongfeng-Tongji Cohort. Atherosclerosis 285:10–16
Friedland DR et al (2009) Audiometric pattern as a predictor of cardiovascular status: development of a model for assessment of risk. Laryngoscope 119:473–486
Gan WQ et al (2016) Exposure to loud noise, bilateral high-frequency hearing loss and coronary heart disease. Occup Environ Med 73:34–41
Gates GA et al (1993) The relation of hearing in the elderly to the presence of cardiovascular disease and cardiovascular risk factors. Arch Otolaryngol Head Neck Surg 119:156–161
Han X et al (2018) Metabolic syndrome is associated with hearing loss among a middle-aged and older Chinese population: a cross-sectional study. Ann Med 50:587–595
International Labour Organization (2012) International standard classification of occupations. Switzerland, Geneva
Jayakody DMP et al (2018) Association between speech and high-frequency hearing loss and depression, anxiety and stress in older adults. Maturitas 110:86–91
Karpa MJ et al (2010) Associations between hearing impairment and mortality risk in older persons: the Blue Mountains Hearing Study. Ann Epidemiol 20:452–459
Kim MB et al (2017) Diabetes mellitus and the incidence of hearing loss: a cohort study. Int J Epidemiol 46:717–726
Kim JY et al (2018a) Association of Sudden Sensorineural Hearing Loss With Risk of Cardiocerebrovascular Disease: a study using data from the Korea National Health Insurance Service. JAMA Otolaryngol Head Neck Surg 144:129–135
Kim SY et al (2018b) Sudden sensorineural hearing loss predicts ischemic stroke: a longitudinal follow-up study. Otol Neurotol 39:964–969
Lammers MJW et al (2021) Risk of stroke and myocardial infarction after sudden sensorineural hearing loss: a meta-analysis. Laryngoscope 131:1369–1377
Lee H (2014) Recent advances in acute hearing loss due to posterior circulation ischemic stroke. J Neurol Sci 338:23–29
Lee JS et al (2015) Lipid profiles and obesity as potential risk factors of sudden sensorineural hearing loss. PLoS One 10:e0122496
Lee HY et al (2016) Metabolic syndrome is not an independent risk factor for hearing impairment. J Nutr Health Aging 20:816–824
Lee W et al (2020) Hearing loss and risk of overall, injury-related, and cardiovascular mortality: the Kangbuk Samsung Health Study. J Clin Med 9:1415
Li CM et al (2014) Hearing impairment associated with depression in US adults, National Health and Nutrition Examination Survey 2005–2010. Jama Otolaryngol 140:293–302
Li W et al (2020) Association of occupational noise exposure, bilateral hearing loss with hypertension among Chinese workers. J Hypertens 39:643–650
Licitra G et al (2016) Annoyance evaluation due to overall railway noise and vibration in Pisa urban areas. Sci Total Environ 568:1315–1325
Liljas AE et al (2016) Socio-demographic characteristics, lifestyle factors and burden of morbidity associated with self-reported hearing and vision impairments in older British community-dwelling men: a cross-sectional study. J Public Health (oxf) 38:e21–e28
Lin HC et al (2008) Sudden sensorineural hearing loss increases the risk of stroke: a 5-year follow-up study. Stroke 39:2744–2748
Luepker RV et al (2003) Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation 108:2543–2549
Miedema HM, Oudshoorn CG (2001) Annoyance from transportation noise: relationships with exposure metrics DNL and DENL and their confidence intervals. Environ Health Perspect 109:409–416
Minichilli F et al (2018) Annoyance judgment and measurements of environmental noise: a focus on italian secondary schools. Int J Environ Res Public Health 15:208
Muzet A (2007) Environmental noise, sleep and health. Sleep Med Rev 11:135–142
Petri D et al (2021) Effects of exposure to road, railway, airport and recreational noise on blood pressure and hypertension. Int J Environ Res Public Health 18:9145
Rossi L et al (2018) Effects of low-frequency noise on human cognitive performances in laboratory. Build Acoust 25:17–33
Saxelby C (2006) Cardiovascular disease: diet, nutrition and emerging risk factors, 63:189–191 pp
Susmano A, Rosenbush SW (1988) Hearing loss and ischemic heart disease. Am J Otol 9:403–408
Tan HE et al (2018) Associations between cardiovascular disease and its risk factors with hearing loss-A cross-sectional analysis. Clin Otolaryngol 43:172–181
Vukic L et al (2021) Seafarers’ perception and attitudes towards noise emission on board ships. Int J Environ Res Public Health 18:6671
Wang F et al (2013) Cohort Profile: the Dongfeng-Tongji cohort study of retired workers. Int J Epidemiol 42:731–740
Weng T et al (2013) A clinical study of serum lipid disturbance in Chinese patients with sudden deafness. Lipids Health Dis 12:95
World Health Organization (2016) International statistical classification of diseases and related health problems 10th revision (ICD-10)-WHO version for 2016
World Health Organization (2017) Prevention of deafness and hearing impaired grades of hearing impairment
World Health Organization (2021) Deafness and hearing loss. http://www.who.int/en/news-room/fact-sheets/detail/deafness-and-hearing-loss
Xu D, Francis AL (2019) Relationships among self-reported hearing problems, psychological distress, and cardiovascular disease in U.S. adults, National Health Interview Survey 1997–2017. J Speech Lang Hear Res 62:2872–2881
Zacarias FF et al (2013) Noise exposure in preterm infants treated with respiratory support using neonatal helmets. Acta Acust United Ac 99:590–597
Zhou BF, Cooperative Meta-Analysis Group of the Working Group on Obesity in C (2002) Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 15:83–96
Zhou L et al (2020) Sleep duration, midday napping, and sleep quality and incident stroke: the Dongfeng-Tongji cohort. Neurology 94:e345–e356
Acknowledgements
We thank the participants and staff of the Department of Otorhinolaryngology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Dongfeng Central Hospital, and the Medical Insurance Center of DMC for their valuable contributions to scientific research.
Funding
This work was supported by the National Natural Science Foundation of China (81973128) and Fundamental Research Funds for the Central Universities, HUST (2020kfyXJJS058). The funders had no roles in the study design, implementation, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Prof. Zhang and Prof. Kong had full access to all data and took responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Xiaomin Zhang and Weijia Kong.
Acquisition, analysis, or interpretation of the data: All authors.
Drafting of the manuscript: Liangle Yang and Qin Fang.
Critical revision of the manuscript for important intellectual contents: All authors.
Statistical analysis: Liangle Yang and Qin Fang.
Obtained Funding: Xiaomin Zhang and Liangle Yang.
Administrative, technical, or material support: Lue Zhou, Hao Wang, Handong Yang, and Zhichao Wang.
Supervision: Meian He.
Corresponding authors
Ethics declarations
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yang, L., Fang, Q., Zhou, L. et al. Hearing loss is associated with increased risk of incident stroke but not coronary heart disease among middle-aged and older Chinese adults: the Dongfeng-Tongji cohort study. Environ Sci Pollut Res 29, 21198–21209 (2022). https://doi.org/10.1007/s11356-021-17324-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-17324-6