Abstract
Purpose
To evaluate the effects of nocturnal asthma on sleep parameters and inflammatory markers according to the severity of the condition in participants in the São Paulo Epidemiologic Sleep Study (EPISONO).
Methods
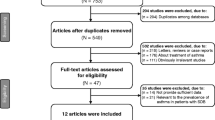
Data from the 2007 and 2018 editions of the EPISONO study were utilized. Subjects completed validated sleep and respiratory questionnaires, underwent nocturnal polysomnography and spirometry tests, and provided blood samples for the assessment of inflammatory parameters.
Results
Of 72 participants (67% women), 53% (n = 38) had intermittent nocturnal asthma symptoms and 47% (n = 34) had persistent asthma (mild, moderate, and severe). Individuals with persistent nocturnal symptoms had a higher body mass index (BMI), were more likely to have respiratory symptoms, and had worse lung function, a higher apnea-hypopnea index (AHI), and higher desaturation index than individuals with intermittent nocturnal symptoms. Positive associations were identified between nocturnal asthma and obstructive sleep apnea (OSA). A higher frequency of OSA was observed in participants with persistent asthma and participants with OSA were more likely to have persistent than intermittent asthma. However, there were no significant differences between the immunological parameters of those with intermittent or persistent asthma.
Conclusions
This study highlights the relevance of nocturnal symptoms as a valuable indicator of asthma severity. The findings also add to the existing body of evidence linking nocturnal asthma and OSA.
Similar content being viewed by others
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Global Initiative for Asthma (2022) Global Strategy for Asthma Management and Prevention. Retrieved from https://www.ginasthma.org/
Global Asthma Network (2018) The Global Asthma Report. Auckland, New Zealand. Retrieved from https://globalasthmanetwork.org/
Skloot GS (2002) Nocturnal asthma: mechanisms and management. Mt Sinai J Med 69:140–147
Turner-Warwick M (1988) Epidemiology of nocturnal asthma. Am J Med 85:6–8. https://doi.org/10.1016/0002-9343(88)90231-8
Raherison C, Abouelfath A, Le Gros V et al (2006) Underdiagnosis of nocturnal symptoms in asthma in general practice. J Asthma 43:199–202. https://doi.org/10.1080/02770900600566744
Pinyochotiwong C, Chirakalwasan N, Collop N (2021) Nocturnal asthma. Asian Pac J Allergy Immunol 39:78–88. https://doi.org/10.12932/AP-231020-0986
Greenberg H, Cohen RI (2012) Nocturnal asthma. Curr Opin Pulm Med 18:57–62
National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma (2007) Expert panel report 3: guidelines for the diagnosis and management of asthma. National Heart, Lung, and Blood Institute (US), Bethesda, MD. Available from: https://www.ncbi.nlm.nih.gov/books/NBK7232/
Cloutier MM, Baptist AP, Blake KV et al (2020) 2020 Focused updates to the asthma management guidelines: a report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol 146:1217–1270. https://doi.org/10.1016/j.jaci.2020.10.003
Kavanagh J, Jackson DJ, Kent BD (2018) Sleep and asthma. Curr Opin Pulm Med 24:569–573. https://doi.org/10.1097/MCP.0000000000000526
Fagnano M, Bayer AL, Isensee CA et al (2011) Nocturnal asthma symptoms and poor sleep quality among urban school children with asthma. Acad Pediatr 11:493–499. https://doi.org/10.1016/j.acap.2011.05.006
Krouse HJ, Yarandi H, McIntosh J et al (2008) Assessing sleep quality and daytime wakefulness in asthma using wrist actigraphy. J Asthma 45:389–395. https://doi.org/10.1080/02770900801971800
Jensen ME, Gibson PG, Collins CE et al (2013) Increased sleep latency and reduced sleep duration in children with asthma. Sleep Breath 17:281–287. https://doi.org/10.1007/s11325-012-0687-1
Khassawneh B, Tsai SC, Meltzer LJ (2019) Polysomnographic characteristics of adolescents with asthma and low risk for sleep-disordered breathing. Sleep Breath 23:943–951. https://doi.org/10.1007/s11325-018-01774-3
Luyster FS, Shi X, Baniak LM et al (2020) Associations of sleep duration with patient-reported outcomes and health care use in US adults with asthma. Ann Allergy Asthma Immunol 125:319–324. https://doi.org/10.1016/j.anai.2020.04.035
Althoff MD, Ghincea A, Wood LG et al (2021) Asthma and three colinear comorbidities: obesity, OSA, and GERD. J Allergy Clin Immunol Pract 9:3877–3884. https://doi.org/10.1016/j.jaip.2021.09.003
Bryant PA, Trinder J, Curtis N (2004) Sick and tired: does sleep have a vital role in the immune system? Nat Rev Immunol 4:457–467. https://doi.org/10.1038/nri1369
Späth-Schwalbe E, Hansen K, Schmidt F et al (1998) Acute effects of recombinant human interleukin-6 on endocrine and central nervous sleep functions in healthy men 1. J Clin Endocrinol Metab 83:1573–1579. https://doi.org/10.1210/jcem.83.5.4795
Lange T, Dimitrov S, Born J (2010) Effects of sleep and circadian rhythm on the human immune system. Ann N Y Acad Sci 1193:48–59. https://doi.org/10.1111/j.1749-6632.2009.05300.x
Irwin MR, Olmstead R, Carroll JE (2016) Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 80:40–52. https://doi.org/10.1016/j.biopsych.2015.05.014
Mullington JM, Simpson NS, Meier-Ewert HK, Haack M (2010) Sleep loss and inflammation. Best Pract Res Clin Endocrinol Metab 24:775–784
Santos-Silva R, Tufik S, Conway SG et al (2009) Sao Paulo Epidemiologic Sleep Study: rationale, design, sampling, and procedures. Sleep Med 10:679–685. https://doi.org/10.1016/j.sleep.2008.11.001
Pires MLN, Benedito-Silva AA, Mello MT, et al (2007) Sleep habits and complaints of adults in the city of São Paulo, Brazil, in 1987 and 1995. Braz J Med Biol Res 40:1505–1515. https://doi.org/10.1590/S0100-879X2006005000170
Expert Panel Working Group of the National Heart, Lung, and Blood Institute (NHLBI) administered and coordinated National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC); Cloutier MM, Baptist AP, Blake KV et al (2020) 2020 Focused updates to the asthma management guidelines: a report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol 146:1217–1270. https://doi.org/10.1016/j.jaci.2020.10.003
Teodorescu M, Polomis DA, Teodorescu MC et al (2012) Association of obstructive sleep apnea risk or diagnosis with daytime asthma in adults. J Asthma 49:620–628. https://doi.org/10.3109/02770903.2012.689408
Ferris BG (1978) Epidemiology standardization project (American Thoracic Society). Am Rev Respir Dis 118:1–120
Miller MR, Hankinson J, Brusasco V et al (2005) Standardisation of spirometry. Eur Respir J 26:319–338
Cooper BG, Stocks J, Hall GL et al (2017) The global lung function initiative (GLI) network: bringing the world’s respiratory reference values together. Breathe 13:e56–e64. https://doi.org/10.1183/20734735.012717
Pereira CA, Sato T, Rodrigues SC (2007) Novos valores de referência para espirometria forçada em brasileiros adultos de raça branca. J Bras Pneumol 33:397–406. https://doi.org/10.1590/S1806-37132007000400008
Bertolazi AN, Fagondes SC, Hoff LS et al (2011) Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med 12:70–75. https://doi.org/10.1016/j.sleep.2010.04.020
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545. https://doi.org/10.1093/sleep/14.6.540
Berry RB, Gamaldo CE, Harding SM et al (2015) AASM Scoring Manual Version 2.2 Updates: New chapters for scoring infant sleep staging and home sleep apnea testing. J Clin Sleep Med 11:1253–1254. https://doi.org/10.5664/jcsm.5176
Tempaku PF, Oliveira Silva L, Guimarães TM et al (2022) The reproducibility of clinical OSA subtypes: a population-based longitudinal study. Sleep Breath 26:1253–1263. https://doi.org/10.1007/s11325-021-02470-5
Jamovi (2022) The jamovi project (version 2.3) [Computer Software]. Retrieved from https://www.jamovi.org/
Sutherland E (2005) Nocturnal asthma. J Allergy Clin Immunol 116:1179–1186. https://doi.org/10.1016/j.jaci.2005.09.028
Martin RJ, Cicutto LC, Smith HR et al (1991) Airways inflammation in nocturnal asthma. Am Rev Respir Dis 143:351–357. https://doi.org/10.1164/ajrccm/143.2.351
Janson C, Gislason T, Boman G et al (1990) Sleep disturbances in patients with asthma. Respir Med 84:37–42. https://doi.org/10.1016/S0954-6111(08)80092-3
Fiori NS, Gonçalves H, Dumith SC et al (2012) Ten-year trends in prevalence of asthma in adults in southern Brazil: comparison of two population-based studies. Cad Saude Publica 28:135–144. https://doi.org/10.1590/S0102-311X2012000100014
Qin X, Pate CA, Zahran HS (2023) Adult asthma prevalence and trend analysis by urban–rural status across sociodemographic characteristics—United States, 2012-20. J Allergy Clin Immunol 2:100085. https://doi.org/10.1016/j.jacig.2023.100085
Kourlaba G, Bakakos P, Loukides S et al (2019) The self-reported prevalence and disease burden of asthma in Greece. J Asthma 56:478–497. https://doi.org/10.1080/02770903.2018.1471704
Eisner MD, Katz PP, Yelin EH et al (2000) Risk factors for hospitalization among adults with asthma: the influence of sociodemographic factors and asthma severity. Respir Res 2:4. https://doi.org/10.1186/rr37
Hirano T, Matsunaga K (2018) Late-onset asthma: current perspectives. J Asthma Allergy 11:19–27. https://doi.org/10.2147/JAA.S125948
Boulos MI, Jairam T, Kendzerska T et al (2019) Normal polysomnography parameters in healthy adults: a systematic review and meta-analysis. Lancet Respir Med 7:533–543. https://doi.org/10.1016/S2213-2600(19)30057-8
Nehring SM, Goyal A, Patel BC (2023) C Reactive Protein. In StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL). Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK441843/
Laurent J, Noirot C, Ansquer JC et al (1985) Comment définir le taux normal des IgE sériques chez l’adulte? [How to define the normal level of serum IgE in adults?]. Ann Med Interne (Paris) 136:419–422
Luyster FS, Teodorescu M, Bleecker E et al (2012) Sleep quality and asthma control and quality of life in non-severe and severe asthma. Sleep Breath 16:1129–1137. https://doi.org/10.1007/s11325-011-0616-8
Alanazi TM, Alghamdi HS, Alberreet MS et al (2021) The prevalence of sleep disturbance among asthmatic patients in a tertiary care center. Sci Rep 11. https://doi.org/10.1038/s41598-020-79697-x
Stores G, Ellis AJ, Wiggs L et al (1998) Sleep and psychological disturbance in nocturnal asthma. Arch Dis Child 78:413–419. https://doi.org/10.1136/adc.78.5.413
Kilic H, Karalezli A, Hasanoglu HC et al (2012) The relationship between hs-CRP and asthma control test in asthmatic patients. Allergol Immunopathol (Madr) 40:362–367. https://doi.org/10.1016/j.aller.2011.10.002
Lou HM (2007) Immunoglobulin E-mediated airway inflammation is active in most patients with asthma. J Am Acad Nurse Pract 19:439–449. https://doi.org/10.1111/j.1745-7599.2007.00251.x
Rand Sutherland E, Martin RJ, Ellison MC, Kraft M (2002) Immunomodulatory effects of melatonin in asthma. Am J Respir Crit Care Med 166:1055–1061. https://doi.org/10.1164/rccm.200204-356OC
Demarco R, Marcon A, Jarvis D et al (2006) Prognostic factors of asthma severity: a 9-year international prospective cohort study. J Allergy Clin Immunol 117:1249–1256. https://doi.org/10.1016/j.jaci.2006.03.019
Ulrik CS, Lange P (1994) Decline of lung function in adults with bronchial asthma. Am J Respir Crit Care Med 150:629–634. https://doi.org/10.1164/ajrccm.150.3.8087330
Klepaker G, Henneberger PK, Hertel JK et al (2021) Influence of asthma and obesity on respiratory symptoms, work ability and lung function: findings from a cross-sectional Norwegian population study. BMJ Open Respir Res 8:e000932. https://doi.org/10.1136/bmjresp-2021-000932
Wang D, Zhou Y, Chen R et al (2023) The relationship between obstructive sleep apnea and asthma severity and vice versa: a systematic review and meta-analysis. Eur J Med Res 28:139. https://doi.org/10.1186/s40001-023-01097-4
Kong D-L, Qin Z, Shen H et al (2017) Association of obstructive sleep apnea with asthma: a meta-analysis. Sci Rep 7:4088. https://doi.org/10.1038/s41598-017-04446-6
Damianaki A, Vagiakis E, Sigala I et al (2019) Τhe co-existence of obstructive sleep apnea and bronchial asthma: revelation of a new asthma phenotype? J Clin Med 8:1476. https://doi.org/10.3390/jcm8091476
Araujo AMS, Duarte RLM, Gozal D et al (2023) Predictive factors for obstructive sleep apnea in adults with severe asthma receiving biologics: a single-center cross-sectional study. Sleep Breath 27:1091–1098. https://doi.org/10.1007/s11325-022-02710-2
Teodorescu M, Broytman O, Curran-Everett D et al (2015) Obstructive sleep apnea risk, asthma burden, and lower airway inflammation in adults in the Severe Asthma Research Program (SARP) II. J Allergy Clin Immunol Pract 3:566–575.e1. https://doi.org/10.1016/j.jaip.2015.04.002
Al-Lawati F, Al-Mubaihsi SM, Jayakrishnan B et al (2022) Obstructive sleep apnea in patients with severe asthma: prevalence and association between severity and asthma control. Ann Thorac Med 17:118–123. https://doi.org/10.4103/atm.atm_375_21
Julien JY, Martin JG, Ernst P et al (2009) Prevalence of obstructive sleep apnea–hypopnea in severe versus moderate asthma. J Allergy Clin Immunol 124:371–376. https://doi.org/10.1016/j.jaci.2009.05.016
Prasad B, Nyenhuis SM, Imayama I et al (2020) Asthma and obstructive sleep apnea overlap: what has the evidence taught us? Am J Respir Crit Care Med 201:1345–1357. https://doi.org/10.1164/rccm.201810-1838TR
Sundbom F, Janson C, Malinovschi A, Lindberg E (2018) Effects of coexisting asthma and obstructive sleep apnea on sleep architecture, oxygen saturation, and systemic inflammation in women. J Clin Sleep Med 14:253–259. https://doi.org/10.5664/jcsm.6946
Alharbi M, Almutairi A, Alotaibi D et al (2009) The prevalence of asthma in patients with obstructive sleep apnoea. Prim Care Respir J 18:328–330. https://doi.org/10.4104/pcrj.2009.00020
Yigla M, Tov N, Solomonov A et al (2003) Difficult-to-control asthma and obstructive sleep apnea. J Asthma 40:865–871. https://doi.org/10.1081/JAS-120023577
Pepito DL, Mohammed JM, Hardin KA (2021) Obstructive sleep apnea and asthma: more than chance? Curr Pulmonol Rep 10:84–91. https://doi.org/10.1007/s13665-021-00271-5
Lafond C, Series F, Lemiere C (2006) Impact of CPAP on asthmatic patients with obstructive sleep apnoea. Eur Respir J 29:307–311. https://doi.org/10.1183/09031936.00059706
Ciftci TU, Ciftci B, Firat Guven S et al (2005) Effect of nasal continuous positive airway pressure in uncontrolled nocturnal asthmatic patients with obstructive sleep apnea syndrome. Respir Med 99:529–534. https://doi.org/10.1016/j.rmed.2004.10.011
Gleeson M, McNicholas WT (2022) Bidirectional relationships of comorbidity with obstructive sleep apnoea. Eur Respir Rev 31:210256. https://doi.org/10.1183/16000617.0256-2021
Kline CE (2020) Polysomnography. In: Encyclopedia of behavioral medicine. Springer International Publishing, Cham, pp 1700–1704
Funding
Our studies are supported by grants from the Associacão Fundo de Incentivo à Pesquisa (AFIP) and Sao Paulo Research Foundation (FAPESP #2020/13467-8 to MLA and #2021/13004-0 to DSR). M.L.A. and D.S.R. are Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) fellowship recipients.
Author information
Authors and Affiliations
Contributions
The study was designed by M.R.S., M.L.A., D.S.R., T.A.A., and S.T. P.K.M. assisted with the statistical analysis. The preparation of the manuscript, including revising the text format, references, terminology, and overall structure, was a collaborative effort involving M.R.S., M.L.A., D.S.R., T.A.A., S.T., and P.K.M.
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Ethics Committee of Universidade Federal de São Paulo (CEP: 593/2006; 0985/2017).
Consent to participate
Written informed consent forms were completed and signed by all participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Souza, M.R., Rosa, D.S., Alvarenga, T.A. et al. Do nocturnal asthma attacks influence sleep parameters and inflammatory markers? A cross-sectional population-based study. Sleep Breath 28, 619–627 (2024). https://doi.org/10.1007/s11325-023-02935-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02935-9