Abstract
Purpose
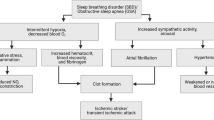
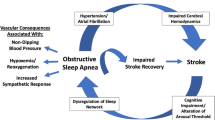
Obstructive sleep apnea (OSA) and stroke affect each other. In this review, we summarized the effect of OSA on the onset and recurrence of stroke, the prognosis, and the treatment of poststroke patients with OSA.
Methods
Pubmed/MEDLINE were searched through May 2023 to explore the relationship between OSA and stroke. The relevant papers included OSA and stroke, OSA and recurrent stroke, and the prognosis and treatment of poststroke patients with OSA.
Results
The results showed that OSA can promote the onset and recurrence of stroke and that OSA may adversely affect the prognosis of poststroke patients. The application of continuous positive airway pressure (CPAP) and other treatments may benefit poststroke patients with OSA, though the long term effects of treatment are not well documented.
Conclusion
Both the onset and recurrence of stroke closely correlated with OSA, but the specific mechanisms remain unclear. Further studies should be carried out to explore effective treatments in patients with stroke and OSA.

Similar content being viewed by others
Data availability
My manuscript has no associated data.
References
Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, Abbasifard M, Abbasi-Kangevari M, Abd-Allah F, Abedi V, Abualhasan A (2021) Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 20:795–820. https://doi.org/10.1016/S1474-4422(21)00252-0
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50:e344–e418. https://doi.org/10.1161/STR.0000000000000211
Caprio FZ, Sorond FA (2019) Cerebrovascular disease: primary and secondary stroke prevention. Med Clin North Am 103:295–308. https://doi.org/10.1016/j.mcna.2018.10.001
Patel SR (2019) Obstructive sleep apnea. Ann Intern Med 171:C81–C96. https://doi.org/10.7326/AITC201912030
Gleeson M, McNicholas WT (2022) Bidirectional relationships of comorbidity with obstructive sleep apnoea. Eur Respir Rev 31. https://doi.org/10.1183/16000617.0256-2021
Mochol J, Gawrys J, Gajecki D, Szahidewicz-Krupska E, Martynowicz H, Doroszko A (2021) Cardiovascular disorders triggered by obstructive sleep apnea-A focus on endothelium and clood components. Int J Mol Sci 22. https://doi.org/10.3390/ijms22105139
Johnson KG, Johnson DC (2010) Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin Sleep Med 6:131–137
Hale E, Gottlieb E, Usseglio J, Shechter A (2023) Post-stroke sleep disturbance and recurrent cardiovascular and cerebrovascular events: a systematic review and meta-analysis. Sleep Med 104:29–41. https://doi.org/10.1016/j.sleep.2023.02.019
Swartz RH, Cayley ML, Lanctôt KL, Murray BJ, Cohen A, Thorpe KE et al (2017) The "DOC" screen: Feasible and valid screening for depression, Obstructive sleep apnea (OSA) and cognitive impairment in stroke prevention clinics. Plos One 12:e174451. https://doi.org/10.1371/journal.pone.0174451
Gaines J, Vgontzas AN, Fernandez-Mendoza J, Bixler EO (2018) Obstructive sleep apnea and the metabolic syndrome: the road to clinically-meaningful phenotyping, improved prognosis, and personalized treatment. Sleep Med Rev 42:211–219. https://doi.org/10.1016/j.smrv.2018.08.009
Boulos MI, Dharmakulaseelan L, Brown DL, Swartz RH (2021) Trials in sleep apnea and stroke: learning from the past to direct future approaches. Stroke 52:366–372. https://doi.org/10.1161/STROKEAHA.120.031709
Nilius G, Schroeder M, Domanski U, Tietze A, Schäfer T, Franke KJ (2019) Telemedicine improves continuous positive airway pressure adherence in stroke patients with obstructive sleep apnea in a randomized trial. Respiration. https://doi.org/10.1159/000501656
Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y (2013) Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol 169:207–214. https://doi.org/10.1016/j.ijcard.2013.08.088
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353:2034–2041. https://doi.org/10.1056/NEJMoa043104
Stone KL, Blackwell TL, Ancoli-Israel S, Barrett-Connor E, Bauer DC, Cauley JA et al (2016) Sleep disordered breathing and risk of stroke in older community-dwelling men. Sleep 39:531–540. https://doi.org/10.5665/sleep.5520
Rola R, Jarosz H, Wierzbicka A, Wichniak A, Richter P, Ryglewicz D et al (2008) Sleep disorderd breathing and recurrence of cerebrovascular events, case-fatality, and functional outcome in patients with ischemic stroke or transient ischemic attack. J Physiol Pharmacol 59(Suppl 6):615–621
Brown DL, Shafie-Khorassani F, Kim S, Chervin RD, Case E, Morgenstern LB et al (2019) Sleep-disordered breathing is associated with recurrent ischemic stroke. Stroke 50:571–576. https://doi.org/10.1161/STROKEAHA.118.023807
Lisabeth LD, Sánchez BN, Lim D, Chervin RD, Case E, Morgenstern LB et al (2019) Sleep-disordered breathing and poststroke outcomes. Ann Neurol 86:241–250. https://doi.org/10.1002/ana.25515
Festic N, Alejos D, Bansal V, Mooney L, Fredrickson PA, Castillo PR et al (2018) Sleep apnea in patients hospitalized with acute ischemic stroke: underrecognition and associated clinical outcomes. J Clin Sleep Med 14:75–80. https://doi.org/10.5664/jcsm.6884
Kumar R, Suri JC, Manocha R (2017) Study of association of severity of sleep disordered breathing and functional outcome in stroke patients. Sleep Med 34:50–56. https://doi.org/10.1016/j.sleep.2017.02.025
Tsivgoulis G, Alexandrov AV, Katsanos AH, Barlinn K, Mikulik R, Lambadiari V et al (2017) Noninvasive ventilatory correction in patients with acute ischemic stroke: a systematic review and meta-analysis. Stroke 48:2285–2288. https://doi.org/10.1161/STROKEAHA.117.017661
Gupta A, Shukla G, Afsar M, Poornima S, Pandey RM, Goyal V et al (2018) Role of positive airway pressure therapy for obstructive sleep apnea in patients with stroke: a randomized controlled trial. J Clin Sleep Med. https://doi.org/10.5664/jcsm.7034
Parra O, Sánchez-Armengol Á, Capote F, Bonnin M, Arboix A, Campos-Rodríguez F et al (2015) Efficacy of continuous positive airway pressure treatment on 5-year survival in patients with ischaemic stroke and obstructive sleep apnea: a randomized controlled trial. J Sleep Res 24:47–53. https://doi.org/10.1111/jsr.12181
Haba-Rubio J, Vujica J, Franc Y, Michel P, Heinzer R (2019) Effect of CPAP treatment of sleep apnea on clinical prognosis after ischemic stroke: an observational study. J Clin Sleep Med 15:839–847. https://doi.org/10.5664/jcsm.7832
Bassetti C, Randerath W, Vignatelli L, Ferini-Strambi L, Brill AK, Bonsignore MR et al (2020) EAN/ERS/ESO/ESRS statement on the impact of sleep disorders on risk and outcome of stroke. Eur J Neurol 27:1117–1136. https://doi.org/10.1111/ene.14201
Young T (2009) Rationale, design and findings from the Wisconsin Sleep Cohort Study: toward understanding the total societal burden of sleep disordered breathing. Sleep Med Clin 4:37–46. https://doi.org/10.1016/j.jsmc.2008.11.003
Roaldsen MB, Lindekleiv H, Eltoft A, Jusufovic M, Søyland MH, Petersson J et al (2021) Tenecteplase in wake-up ischemic stroke trial: protocol for a randomized-controlled trial. Int J Stroke 16:990–994. https://doi.org/10.1177/1747493020984073
Xiao Z, Xie M, You Y, Wu H, Zhou G, Li M (2018) Wake-up stroke and sleep-disordered breathing: a meta-analysis of current studies. J Neurol 265:1288–1294. https://doi.org/10.1007/s00415-018-8810-2
Aurora RN, Crainiceanu C, Gottlieb DJ, Kim JS, Punjabi NM (2018) Obstructive sleep apnea during REM sleep and cardiovascular disease. Am J Respir Crit Care Med 197:653–660. https://doi.org/10.1164/rccm.201706-1112OC
Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S et al (2016) Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol 15:913–924. https://doi.org/10.1016/S1474-4422(16)30073-4
Harańczyk M, Konieczyńska M, Płazak W (2022) Endothelial dysfunction in obstructive sleep apnea patients. Sleep Breath 26:231–242. https://doi.org/10.1007/s11325-021-02382-4
Chen J, Lin S, Zeng Y (2021) An update on obstructive sleep apnea for atherosclerosis: mechanism, diagnosis, and treatment. Front Cardiovasc Med 8:647071. https://doi.org/10.3389/fcvm.2021.647071
Bradley TD, Floras JS (2009) Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373:82–93. https://doi.org/10.1016/S0140-6736(08)61622-0
Huang B, Liu H, Scherlag BJ, Sun L, Xing S, Xu J et al (2021) Atrial fibrillation in obstructive sleep apnea: neural mechanisms and emerging therapies. Trends Cardiovasc Med 31:127–132. https://doi.org/10.1016/j.tcm.2020.01.006
Yan L, Park HR, Kezirian EJ, Yook S, Kim JH, Joo EY et al (2021) Altered regional cerebral blood flow in obstructive sleep apnea is associated with sleep fragmentation and oxygen desaturation. J Cereb Blood Flow Metab 41:2712–2724. https://doi.org/10.1177/0271678X211012109
Shirasaki O, Kuwabara M, Saito M, Tagami K, Washiya S, Kario K (2011) Development and clinical application of a new technique for detecting 'sleep blood pressure surges' in sleep apnea patients based on a variable desaturation threshold. Hypertens Res 34:922–928. https://doi.org/10.1038/hr.2011.52
Xu J, Ding N, Chen L, Zhang Y, Huang M, Wang Y et al (2019) Inducers of post-apneic blood pressure fluctuation monitored by pulse transfer time measurement in obstructive sleep apnea varied with syndrome severity. Sleep Breath 23:769–776. https://doi.org/10.1007/s11325-018-1770-z
Urbano F, Roux F, Schindler J, Mohsenin V (1985) Impaired cerebral autoregulation in obstructive sleep apnea. J Appl Physiol 2008(105):1852–1857. https://doi.org/10.1152/japplphysiol.90900.2008
Lavie L, Dyugovskaya L, Lavie P (2005) Sleep-apnea-related intermittent hypoxia and atherogenesis: adhesion molecules and monocytes/endothelial cells interactions. Atherosclerosis 183:183–184. https://doi.org/10.1016/j.atherosclerosis.2005.06.024
Mohan KM, Wolfe CD, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP (2011) Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke 42:1489–1494. https://doi.org/10.1161/STROKEAHA.110.602615
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD et al (2014) Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45:2160–2236. https://doi.org/10.1161/STR.0000000000000024
McDermott M, Brown DL, Li C, Garcia NM, Case E, Chervin RD et al (2018) Sex differences in sleep-disordered breathing after stroke: results from the BASIC project. Sleep Med 43:54–59. https://doi.org/10.1016/j.sleep.2017.11.1129
Brown DL, Shafie-Khorassani F, Kim S, Chervin RD, Case E, Yadollahi A et al (2019) Do apneas and hypopneas best reflect risk for poor outcomes after stroke? Sleep Med 63:14–17. https://doi.org/10.1016/j.sleep.2019.05.006
Yoshida T, Kuwabara M, Hoshide S, Kario K (2016) Recurrence of stroke caused by nocturnal hypoxia-induced blood pressure surge in a young adult male with severe obstructive sleep apnea syndrome. J Am Soc Hypertens 10:201–204. https://doi.org/10.1016/j.jash.2016.01.013
Gottlieb E, Khlif MS, Bird L, Werden E, Churchward T, Pase MP et al (2021) Sleep architectural dysfunction and undiagnosed obstructive sleep apnea after chronic ischemic stroke. Sleep Med 83:45–53. https://doi.org/10.1016/j.sleep.2021.04.011
Flach C, Muruet W, Wolfe C, Bhalla A, Douiri A (2020) Risk and secondary prevention of stroke recurrence: a Population-Base Cohort Study. Stroke 51:2435–2444. https://doi.org/10.1161/STROKEAHA.120.028992
Brown DL, Jiang X, Li C, Case E, Sozener CB, Chervin RD et al (2019) Sleep apnea screening is uncommon after stroke. Sleep Med 59:90–93. https://doi.org/10.1016/j.sleep.2018.09.009
Li C, Liu Y, Xu P, Fan Q, Gong P, Ding C et al (2020) Association between obstructive sleep apnea and risk of post-stroke depression: a hospital-based study in ischemic stroke patients. J Stroke Cerebrovasc Dis 29:104876. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104876
Klingman KJ, Skufca JD, Duncan PW, Wang D, Fulk GD (2022) Study protocol: Sleep Effects on Poststroke Rehabilitation Study. Nurs Res 71:483–490. https://doi.org/10.1097/NNR.0000000000000611
Muir RT, Kapoor A, Cayley ML, Sicard MN, Lien K, Southwell A et al (2023) Language discordance as a marker of disparities in cerebrovascular risk and stroke outcomes: a multi-center Canadian study. Cereb Circ Cogn Behav 4:100163. https://doi.org/10.1016/j.cccb.2023.100163
Kasner SE (2006) Clinical interpretation and use of stroke scales. Lancet Neurol 5:603–612. https://doi.org/10.1016/S1474-4422(06)70495-1
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 15:335–343. https://doi.org/10.5664/jcsm.7640
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med 15:301–334. https://doi.org/10.5664/jcsm.7638
Duss SB, Seiler A, Schmidt MH, Pace M, Adamantidis A, Müri RM et al (2017) The role of sleep in recovery following ischemic stroke: a review of human and animal data. Neurobiol Sleep Circadian Rhythms 2:94–105. https://doi.org/10.1016/j.nbscr.2016.11.003
Li J, RD ME, Zheng D, Loffler KA, Wang X, Redline S et al (2020) Self-reported snoring patterns predict stroke events in high-risk patients with OSA: post hoc analyses of the SAVE Study. Chest. https://doi.org/10.1016/j.chest.2020.05.615
Sleeper G, Rashidi M, Strohl KP, Najimi N, Chen PL, El GR et al (2022) Comparison of expiratory pressures generated by four different EPAP devices in a laboratory bench setting. Sleep Med 96:87–92. https://doi.org/10.1016/j.sleep.2022.05.004
Chen CY, Chen CL, Yu CC (2021) Trazodone improves obstructive sleep apnea after ischemic stroke: a randomized, double-blind, placebo-controlled, crossover pilot study. J Neurol. https://doi.org/10.1007/s00415-021-10480-2
Svatikova A, Chervin RD, Wing JJ, Sanchez BN, Migda EM, Brown DL (2011) Positional therapy in ischemic stroke patients with obstructive sleep apnea. Sleep Med. https://doi.org/10.1016/j.sleep.2010.12.008
Qian S, Zhang X, Wang T, Zhang L, Hu C, Jia R et al (2022) Effects of comprehensive swallowing intervention on obstructive sleep apnea and dysphagia after stroke: a randomized controlled trial. J Stroke Cerebrovasc Dis 31:106521. https://doi.org/10.1016/j.jstrokecerebrovasdis.2022.106521
Funding
The study was supported by National Natural Science Foundation of China (81900084).
Author information
Authors and Affiliations
Contributions
Bo Sun: screening literature, data analysis, manuscript editing; Qiyun Ma: screening literature, data analysis, manuscript modifying, and polishing; Jiani Shen: screening literature, data analysis; Zili Meng: critical analysis, final approval; Jing Xu: critical analysis, manuscript editing, and final approval
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants performed by any of the authors; therefore, no consent was needed.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, B., Ma, Q., Shen, J. et al. Up-to-date advance in the relationship between OSA and stroke: a narrative review. Sleep Breath 28, 53–60 (2024). https://doi.org/10.1007/s11325-023-02904-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02904-2