Abstract
Purpose
To collect existing evidence on the relationship between sleep duration and health outcomes.
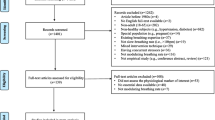
Methods
A thorough search was conducted in PubMed, Web of Science, Embase, and the Cochrane Database of Systematic Reviews from inception to January, 2021. Meta-analyses of observational and interventional studies were eligible if they examined the associations between sleep duration and human health.
Results
In total, this umbrella review identified 69 meta-analyses with 11 outcomes for cancers and 30 outcomes for non-cancer conditions. Inappropriate sleep durations may significantly elevate the risk for cardiovascular disease (CVD), cognitive decline, coronary heart disease (CHD), depression, falls, frailty, lung cancer, metabolic syndrome (MS), and stroke. Dose–response analysis revealed that a 1-h reduction per 24 hours is associated with an increased risk by 3–11% of all-cause mortality, CHD, osteoporosis, stroke, and T2DM among short sleepers. Conversely, a 1-h increment in long sleepers is associated with a 7–17% higher risk of stroke mortality, CHD, stroke, and T2DM in adults.
Conclusion
Inappropriate sleep duration is a risk factor for developing non-cancer conditions. Decreasing and increasing sleep hours towards extreme sleep durations are associated with poor health outcomes.



Similar content being viewed by others
Data availability
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability.
Not applicable.
Ethics approval and consent to participate.
Not applicable.
Consent for publication.
Not applicable.
Abbreviations
- AD:
-
Alzheimer’s disease
- ADHD:
-
Attention deficit hyperactivity disorder
- CHD:
-
Coronary heart disease
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CVD:
-
Cardiovascular disease
- FLD:
-
Fatty liver disease
- GDM:
-
Gestational diabetes mellitus
- HDL:
-
High density lipoprotein
- HR:
-
Hazard ratio
- LDL:
-
Low density lipoprotein
- LGA:
-
Large for gestational age
- MCI:
-
Mild cognitive impairment
- MS:
-
Metabolic syndrome
- NA:
-
Not available
- NFLD:
-
Nonalcoholic fatty liver disease
- OR:
-
Odds ratio
- RCTs:
-
Random control trials
- RR:
-
Relative risk
- SGA:
-
Small for gestational age
- T2DM:
-
Type 2 diabetes mellitus
References
Hirshkowitz M, Whito K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Katz ES, Kheirandish-Gozal L, Neubauer DN, O’Donnell AE, Ohayon M, Peever J, Rawding R, Sachdeva RC, Setters B, Vitiello MV, Ware JC, Adams Hillard PJ (2015) National Sleep Foundation’s sleep time duration recommendations methodology and results summary. Sleep Health 1:40–43. https://doi.org/10.1016/j.sleh.2014.12.01
Warland J, Dorrian J, Morrison JL, O’Brien LM (2018) Maternal sleep during pregnancy and poor fetal outcomes: a scoping review of the literature with meta-analysis. Sleep Med Rev 41:197–219. https://doi.org/10.1016/j.smrv.2018.03.004
Akerstedt T, Nilsson PM (2003) Sleep as restitution: an introduction. J Intern Med 254:6–12. https://doi.org/10.1046/j.1365-2796.2003.01195.x
Bin YS, Marshall NS, Glozier N (2013) Sleeping at the limits: the changing prevalence of short and long sleep durations in 10 countries. Am J Epidemiol 177:826–833. https://doi.org/10.1093/aje/kws308
Itani O, Jike M, Watanabe N, Kaneita Y (2017) Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med 32:246–256. https://doi.org/10.1016/j.sleep.2016.08.006
Lee SWH, Ng KY, Chin WK (2017) The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: a systematic review and meta-analysis. Sleep Med Rev 31:91–101. https://doi.org/10.1016/j.smrv.2016.02.001
Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA (2011) Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 32:1484–1492. https://doi.org/10.1093/eurheartj/ehr007
Jike M, Itani O, Watanabe N, Buysse DJ, Kaneita Y (2018) Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep Med Rev 39:25–36. https://doi.org/10.1016/j.smrv.2017.06.011
Krittanawong C, Tunhasiriwet A, Wang Z, Zhang H, Farrell AM, Chirapongsathorn S, Sun T, Kitai T, Argulian E (2019) Association between short and long sleep durations and cardiovascular outcomes: a systematic review and meta-analysis. European Heart Journal-Acute Cardiovascular Care 8:762–770. https://doi.org/10.1177/2048872617741733
Guo X, Zheng L, Wang J, Zhang X, Zhang X, Li J, Sun Y (2013) Epidemiological evidence for the link between sleep duration and high blood pressure: a systematic review and meta-analysis. Sleep Med 14:324–332. https://doi.org/10.1016/j.sleep.2012.12.001
Gallicchio L, Kalesan B (2009) Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 18:148–158. https://doi.org/10.1111/j.1365-2869.2008.00732.x
Li Y, Cai S, Ling Y, Mi S, Fan C, Zhong Y, Shen Q (2019) Association between total sleep time and all cancer mortality: non-linear dose-response meta-analysis of cohort studies. Sleep Med 60:211–218. https://doi.org/10.1016/j.sleep.2019.03.026
A. Pan, D.A. De Silva, J.M. Yuan, W.P. Koh, Sleep duration and risk of stroke mortality among Chinese adults Singapore Chinese Health Study, Stroke 45 (2014) 1620-+. https://doi.org/10.1161/Strokeaha.114.005181.
J. Yin, X. Jin, Z. Shan, S. Li, H. Huang, P. Li, X. Peng, Z. Peng, K. Yu, W. Bao, W. Yang, X. Chen, L. Liu, Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response Meta-analysis of prospective cohort studies, J Am Heart Assoc 6 (2017). https://doi.org/10.1161/jaha.117.005947.
Liu W, Zhang R, Tan A, Ye B, Zhang X, Wang Y, Zou Y, Ma L, Chen G, Li R, Moore JB (2019) Long sleep duration predicts a higher risk of obesity in adults: a meta-analysis of prospective cohort studies. J Public Health 41:E158–E168. https://doi.org/10.1093/pubmed/fdy135
Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W, Rong Y, Jackson CL, Hu FB, Liu L (2015) Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 38:529–537. https://doi.org/10.2337/dc14-2073
He Q, Sun H, Wu X, Zhang P, Dai H, Ai C, Shi J (2017) Sleep duration and risk of stroke: a dose-response meta-analysis of prospective cohort studies. Sleep Med 32:66–74. https://doi.org/10.1016/j.sleep.2016.12.012
Jiao L, Duan Z, Sangi-Haghpeykar H, Hale L, White DL, El-Serag HB (2013) Sleep duration and incidence of colorectal cancer in postmenopausal women. Br J Cancer 108:213–221. https://doi.org/10.1038/bjc.2012.561
Liu R, Wu S, Zhang B, Guo M, Zhang Y (2020) The association between sleep duration and prostate cancer A systematic review and meta-analysis. Medicine 99:21180. https://doi.org/10.1097/md.0000000000021180
Fatima Y, Doi SA, Mamun AA (2015) Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev 16:137–149. https://doi.org/10.1111/obr.12245
Y. Wang, H. Mei, Y.-R. Jiang, W.-Q. Sun, Y.-J. Song, S.-J. Liu, F. Jiang, Relationship between duration of sleep and hypertension in adults: a meta-analysis, Journal of Clinical Sleep Medicine 11 (2015) 1047-+ PII jc-00343–14. https://doi.org/10.5664/jcsm.5024.
Shen X, Wu Y, Zhang D (2016) Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Sci Rep 6:21480. https://doi.org/10.1038/srep21480
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P (2015) Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc 13:132–140. https://doi.org/10.1097/XEB.0000000000000055
Papatheodorou S (2019) Umbrella reviews: what they are and why we need them. Eur J Epidemiol 34:543–546. https://doi.org/10.1007/s10654-019-00505-6
SIGN. Scottish Intercollegiate Guidelines Network Search Filters. 2015. http://www.sign.ac.uk/search-filters.html.
Fang HF, Miao NF, Chen CD, Sithole T, Chung MH (2015) Risk of cancer in patients with insomnia, parasomnia, and obstructive sleep apnea: a nationwide nested case-control study. J Cancer 6:1140–1147. https://doi.org/10.7150/jca.12490
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. https://doi.org/10.1136/bmj.j4008
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schunemann HJ (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables, J Clin Epidemiol 64:383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026
Stone CR, Haig TR, Fiest KM, McNeil J, Brenner DR, Friedenreich CM (2019) The association between sleep duration and cancer-specific mortality: a systematic review and meta-analysis. Cancer Causes Control 30:501–525. https://doi.org/10.1007/s10552-019-01156-4
Wong ATY, Heath AK, Tong TYN, Reeves GK, Floud S, Beral V, Travis RC (2020) Sleep duration and breast cancer incidence: results from the Million Women Study and meta-analysis of published prospective studies. Sleep. https://doi.org/10.1093/sleep/zsaa166
Chen Y, Tan F, Wei L, Li X, Lyu Z, Feng X, Wen Y, Guo L, He J, Dai M, Li N (2018) Sleep duration and the risk of cancer: a systematic review and meta-analysis including dose-response relationship. BMC Cancer 18:1149. https://doi.org/10.1186/s12885-018-5025-y
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA (2010) Sleep Duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33:585–592. https://doi.org/10.1093/sleep/33.5.585
Li W, Wang D, Cao S, Yin X, Gong Y, Gan Y, Zhou Y, Lu Z (2016) Sleep duration and risk of stroke events and stroke mortality: a systematic review and meta-analysis of prospective cohort studies. Int J Cardiol 223:870–876. https://doi.org/10.1016/j.ijcard.2016.08.302
Yang X, Chen H, Li S, Pan L, Jia C (2015) Association of sleep duration with the morbidity and mortality of coronary artery disease: a meta-analysis of prospective studies. Heart Lung Circ 24:1180–1190. https://doi.org/10.1016/j.hlc.2015.08.005
Lo JC, Groeger JA, Cheng GH, Dijk D-J, Chee MWL (2016) Self-reported sleep duration and cognitive performance in older adults: a systematic review and meta-analysis. Sleep Med 17:87–98. https://doi.org/10.1016/j.sleep.2015.08.021
L. Fan, W. Xu, Y. Cai, Y. Hu, C. Wu, Sleep duration and the risk of dementia: a systematic review and meta-analysis of prospective cohort studies, Journal of the American Medical Directors Association 20 (2019) 1480-+. https://doi.org/10.1016/j.jamda.2019.06.009.
Wu L, Sun D, Tan Y (2018) A systematic review and dose-response meta-analysis of sleep duration and the occurrence of cognitive disorders. Sleep Breath 22:805–814. https://doi.org/10.1007/s11325-017-1527-0
Lee S-H, Kim H-B, Lee K-W (2019) Association between sleep duration and attention-deficit hyperactivity disorder: a systematic review and meta-analysis of observational studies. J Affect Disord 256:62–69. https://doi.org/10.1016/j.jad.2019.05.071
Kruisbrink M, Robertson W, Ji C, Miller MA, Geleijnse JM, Cappuccio FP (2017) Association of sleep duration and quality with blood lipids: a systematic review and meta-analysis of prospective studies. BMJ Open 7:e018585. https://doi.org/10.1136/bmjopen-2017-018585
Shen N, Wang P, Yan W (2016) Sleep duration and the risk of fatty liver disease: a systematic review and meta-analysis. Sci Rep 6:31956. https://doi.org/10.1038/srep31956
Moradi S, Shab-bidar S, Alizadeh S, Djafarian K (2017) Association between sleep duration and osteoporosis risk in middle-aged and elderly women: a systematic review and meta-analysis of observational studies. Metabolism-Clinical and Experimental 69:199–206. https://doi.org/10.1016/j.metabol.2017.01.027
Bacaro V, Ballesio A, Cerolini S, Vacca M, Poggiogalle E, Donini LM, Lucidi F, Lombardo C (2020) Sleep duration and obesity in adulthood: an updated systematic review and meta-analysis. Obes Res Clin Pract 14:301–309. https://doi.org/10.1016/j.orcp.2020.03.004
Wijarnpreecha K, Thongprayoon C, Panjawatanan P, Ungprasert P (2016) Short sleep duration and risk of nonalcoholic fatty liver disease: a systematic review and meta-analysis. J Gastroenterol Hepatol 31:1802–1807. https://doi.org/10.1111/jgh.13391
M.A. Miller, M. Kruisbrink, J. Wallace, C. Ji, F.P. Cappuccio, Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies, Sleep 41 (2018) zsy018. https://doi.org/10.1093/sleep/zsy018.
Wang D, Ruan W, Peng Y, Li W (2018) Sleep duration and the risk of osteoporosis among middle-aged and elderly adults: a dose-response meta-analysis. Osteoporos Int 29:1689–1695. https://doi.org/10.1007/s00198-018-4487-8
Wang L, Hu Y, Wang X, Yang S, Chen W, Zeng Z (2020) The association between sleep duration and hypertension: a meta and study sequential analysis. J Hum Hypertens. https://doi.org/10.1038/s41371-020-0372-y
Wang D, Li W, Cui X, Meng Y, Zhou M, Xiao L, Ma J, Yi G, Chen W (2016) Sleep duration and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Int J Cardiol 219:231–239. https://doi.org/10.1016/j.ijcard.2016.06.027
Zhai L, Zhang H, Zhang D (2015) Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety 32:664–670. https://doi.org/10.1002/da.22386
The relationship between sleep duration and mood in adolescents: a systematic review and meta-analysis, Sleep Medicine Reviews 52 (2020).
Zhang X, Zhang R, Cheng L, Wang Y, Ding X, Fu J, Dang J, Moore J, Li R (2020) The effect of sleep impairment on gestational diabetes mellitus: a systematic review and meta-analysis of cohort studies. Sleep Med 74:267–277. https://doi.org/10.1016/j.sleep.2020.05.014
Wu L, Sun D (2017) Sleep duration and falls: a systemic review and meta-analysis of observational studies. J Sleep Res 26:293–301. https://doi.org/10.1111/jsr.12505
Sleep and frailty risk: a systematic review and meta-analysis, Sleep and Breathing 24 (1187) 1187–1197. https://doi.org/10.1007/s11325-020-02061-w.
Cheungpasitporn W, Thongprayoon C, Gonzalez-Suarez ML, Srivali N, Ungprasert P, Kittanamongkolchai W, Caples SM, Erickson SB (2017) The effects of short sleep duration on proteinuria and chronic kidney disease: a systematic review and meta-analysis. Nephrol Dial Transplant 32:991–996. https://doi.org/10.1093/ndt/gfw072
Liang Y, Qu LB, Liu H (2019) Non-linear associations between sleep duration and the risks of mild cognitive impairment/dementia and cognitive decline: a dose-response meta-analysis of observational studies. Aging Clin Exp Res 31:309–320. https://doi.org/10.1007/s40520-018-1005-y
J.J. Virta, K. Heikkila, M. Perola, M. Koskenvuo, I. Raiha, J.O. Rinne, J. Kaprio, Midlife sleep characteristics associated with late life cognitive function, Sleep 36 (2013) 1533–1541, 1541A. https://doi.org/10.5665/sleep.3052.
Ohayon MM, Vecchierini MF (2002) Daytime sleepiness and cognitive impairment in the elderly population. Arch Intern Med 162:201–208. https://doi.org/10.1001/archinte.162.2.201
Chen JC, Espeland MA, Brunner RL, Lovato LC, Wallace RB, Leng X, Phillips LS, Robinson JG, Kotchen JM, Johnson KC, Manson JE, Stefanick ML, Sarto GE, Mysiw WJ (2016) Sleep duration, cognitive decline, and dementia risk in older women. Alzheimers Dement 12:21–33. https://doi.org/10.1016/j.jalz.2015.03.004
L. Xu, J. C, L. T, L. B, J. Y, Z. T, Z. W, C. K, T. G, T. Email Lam, h. hkucc, hku, hk, Short or long sleep duration is associated with memory impairment in older chinese: the Guangzhou Biobank Cohort Study, Sleep 34 (2011) 575–580. https://doi.org/10.1093/sleep/34.5.575.
Kanda A, Matsui T, Ebihara S, Arai H, Sasaki H (2003) Periventricular white matter lesions and sleep alteration in older people. J Am Geriatr Soc 51:432–433. https://doi.org/10.1046/j.1532-5415.2003.51125.x
Sexton CE, Storsve AB, Walhovd KB, Johansen-Berg H, Fjell AM (2014) Poor sleep quality is associated with increased cortical atrophy in community-dwelling adults. Neurology 83:967–973. https://doi.org/10.1212/Wnl.0000000000000774
Patel SR, Zhu X, Storfer-Isser A, Mehra R, Jenny NS, Tracy R, Redline S (2009) Sleep duration and biomarkers of inflammation. Sleep 32:200–204. https://doi.org/10.1093/sleep/32.2.200
Prather AA, Vogelzangs N, Penninx BW (2015) Sleep duration, insomnia, and markers of systemic inflammation: results from the Netherlands Study of Depression and Anxiety (NESDA). J Psychiatr Res 60:95–102. https://doi.org/10.1016/j.jpsychires.2014.09.018
Grandner MA, Buxton OM, Jackson N, Sands-Lincoln M, Pandey A, Jean-Louis G (2013) Extreme sleep durations and increased C-reactive protein: effects of sex and ethnoracial group. Sleep 36:769–779. https://doi.org/10.5665/sleep.2646
Satizabal CL, Zhu YC, Mazoyer B, Dufouil C, Tzourio C (2012) Circulating IL-6 and CRP are associated with MRI findings in the elderly: the 3C-Dijon Study. Neurology 78:720–727. https://doi.org/10.1212/WNL.0b013e318248e50f
D. Anand, C. G, Z. G, Z. C, T. A, G. Email Colpo, g. gmail, A. com Teixeira, antonio, teixeira@uth, tmc, edu, Attention-deficit/hyperactivity disorder and inflammation: what does current knowledge tell US? A systematic review, Front. Psychiatry Journal Translated Name Frontiers in Psychiatry 8 (2017) no pagination. https://doi.org/10.3389/fpsyt.2017.00228.
Ju YES, Lucey BP, Holtzman DM (2014) Sleep and Alzheimer disease pathology-a bidirectional relationship. Nat Rev Neurol 10:115–119. https://doi.org/10.1038/nrneurol.2013.269
Aziz G, Navabi SS, Al-Shukaili A, Seyedzadeh MH, Yazdani R, Mirshafiey A (2015) The role of inflammatory mediators in the pathogenesis of Alzheimer’s disease. Sultan Qaboos Univ Med J 15:e305-316. https://doi.org/10.18295/squmj.2015.15.03.002
Akiyama H, Barger S, Barnum S, Bradt B, Bauer J, Cole GM, Cooper NR, Eikelenboom P, Emmerling M, Fiebich BL, Finch CE, Frautschy S, Griffin WS, Hampel H, Hull M, Landreth G, Lue L, Mrak R, Mackenzie IR, McGeer PL, O’Banion MK, Pachter J, Pasinetti G, Plata-Salaman C, Rogers J, Rydel R, Shen Y, Streit W, Strohmeyer R, Tooyoma I, Van Muiswinkel FL, Veerhuis R, Walker D, Webster S, Wegrzyniak B, Wenk G, Wyss-Coray T (2000) Inflammation and Alzheimer’s disease. Neurobiol Aging 21:383–421. https://doi.org/10.1016/s0197-4580(00)00124-x
Carter JR, Durocher JJ, Larson RA, DellaValla JP, Yang H (2012) Sympathetic neural responses to 24-hour sleep deprivation in humans: sex differences. Am J Physiol Heart Circ Physiol 302:H1991-1997. https://doi.org/10.1152/ajpheart.01132.2011
Castro-Diehl C, Roux AVD, Redline S, Seeman T, McKinley P, Sloan R, Shea S (2016) Sleep duration and quality in relation to autonomic nervous system measures: the multi-ethnic study of atherosclerosis (MESA). Sleep 39:1927–1940. https://doi.org/10.5665/sleep.6218
Takase B, Akima T, Uehata A, Ohsuzu F, Kurita A (2004) Effect of chronic stress and sleep deprivation on both flow-mediated dilation in the brachial artery and the intracellular magnesium level in humans. Clin Cardiol 27:223–227. https://doi.org/10.1002/clc.4960270411
Paciencia I, Barros H, Araujo J, Ramos E (2013) Association between sleep duration and blood pressure in adolescents. Hypertens Res 36:747–752. https://doi.org/10.1038/hr.2013.36
Y. Wang, H. Mei, Y.R. Jiang, W.Q. Sun, Y.J. Song, S.J. Liu, F. Jiang, Relationship between duration of sleep and hypertension in adults: a meta-analysis, Journal of Clinical Sleep Medicine 11 (2015) 1047-+. PII jc-00343–14 https://doi.org/10.5664/jcsm.5024.
Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB (2006) Correlates of long sleep duration. Sleep 29:A332–A332
Suzuki E, Yorifuji T, Ueshima K, Takao S, Sugiyama M, Ohta T, Ishikawa-Takata K, Doi H (2009) Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population-based cohort study. Prev Med 49:135–141. https://doi.org/10.1016/j.ypmed.2009.06.016
Reinhard W, Plappert N, Zeman F, Hengstenberg C, Riegger G, Novack V, Maimon N, Pfeifer M, Arzt M (2013) Prognostic impact of sleep duration and sleep efficiency on mortality in patients with chronic heart failure. Sleep Med 14:502–509. https://doi.org/10.1016/j.sleep.2012.12.014
Cappuccio FP, D’Elia L, Strazzlillo P, Miller MA (2010) Quantity and quality of sleep and incidence of type 2 diabetes - a systematic review and meta-analysis. Diabetes Care 33:414–420. https://doi.org/10.2337/dc09-1124
Spiegel K, Tasali E, Leproult R, Van Cauter E (2009) Effects of poor and short sleep on glucose metabolism and obesity risk. Nat Rev Endocrinol 5:253–261. https://doi.org/10.1038/nrendo.2009.23
Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E (2005) Sleep loss: a novel risk factor for insulin resistance and type 2 diabetes. J Appl Physiol 99:2008–2019. https://doi.org/10.1152/japplphysiol.00660.2005
S. Taheri, L. Lin, D. Austin, T. Young, E. Mignot, Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index, Plos Med 1 (2004) 210–217. ARTN e62 https://doi.org/10.1371/journal.pmed.0010062.
Erren TC, Morfeld P, Foster RG, Reiter RJ, Gross JV, Westermann IK (2016) Sleep and cancer: synthesis of experimental data and meta-analyses of cancer incidence among some 1,500,000 study individuals in 13 countries. Chronobiol Int 33:325–350. https://doi.org/10.3109/07420528.2016.1149486
Wu AH, Wang RW, Koh WP, Stanczyk FZ, Lee HP, Yu MC (2008) Sleep duration, melatonin and breast cancer among Chinese women in Singapore. Carcinogenesis 29:1244–1248. https://doi.org/10.1093/carcin/bgn100
R.J. Reiter, S.A. Rosales-Corral, D.X. Tan, D. Acuna-Castroviejo, L.L. Qin, S.F. Yang, K.X. Xu, Melatonin, a full service anti-cancer agent: inhibition of initiation, progression and metastasis, Int J Mol Sci 18 (2017). ARTN 843 https://doi.org/10.3390/ijms18040843.
Blask DE (2009) Melatonin, sleep disturbance and cancer risk. Sleep Med Rev 13:257–264. https://doi.org/10.1016/j.smrv.2008.07.007
Sanchez-Barcelo EJ, Cos S, Mediavilla D, Martinez-Campa C, Gonzalez A, Alonso-Gonzalez C (2005) Melatonin-estrogen interactions in breast cancer. J Pineal Res 38:217–222. https://doi.org/10.1111/j.1600-079X.2004.00207.x
Xu L, Liu H, Zhang H, Wang RX, Song J, Zhou RX (2013) Growth-inhibitory activity of melatonin on murine foregastric carcinoma cells in vitro and the underlying molecular mechanism. Anat Rec (Hoboken) 296:914–920. https://doi.org/10.1002/ar.22689
Wang J, Guo W, Chen W, Yu W, Tian Y, Fu L, Shi D, Tong B, Xiao X, Huang W, Deng W (2013) Melatonin potentiates the antiproliferative and pro-apoptotic effects of ursolic acid in colon cancer cells by modulating multiple signaling pathways. J Pineal Res 54:406–416. https://doi.org/10.1111/jpi.12035
Yang WS, Shi YF, Ke XM, Sun HN, Guo JC, Wang X (2019) Long-term sleep habits and the risk of breast cancer among Chinese women: a case-control study. Eur J Cancer Prev 28:323–329. https://doi.org/10.1097/Cej.0000000000000458
Folkerd EJ, Dowsett M (2010) Influence of sex hormones on cancer progression. J Clin Oncol 28:4038–4044. https://doi.org/10.1200/Jco.2009.27.4290
Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI (2010) Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Med Rev 14:239–247. https://doi.org/10.1016/j.smrv.2009.08.001
Kasprzak A, Kwasniewski W, Adamek A, Gozdzicka-Jozefiak A (2017) Insulin-like growth factor (IGF) axis in cancerogenesis. Mutat Res Rev Mutat Res 772:78–104. https://doi.org/10.1016/j.mrrev.2016.08.007
Larsson SC, Carter P, Vithayathil M, Kar S, Mason AM, Burgess S (2020) Insulin-like growth factor-1 and site-specific cancers: a Mendelian randomization study. Cancer Med 9:6836–6842. https://doi.org/10.1002/cam4.3345
Abbott SM, Reid KJ, Zee PC (2015) Circadian rhythm sleep-wake disorders. Psychiatr Clin North Am 38:805–823. https://doi.org/10.1016/j.psc.2015.07.012
Savvidis C, Koutsilieris M (2012) Circadian rhythm disruption in cancer biology. Mol Med 18:1249–1260. https://doi.org/10.2119/molmed.2012.00077
Wennberg AMV, Wu MN, Rosenberg PB, Spira AP (2017) Sleep disturbance, cognitive decline, and dementia: a review. Semin Neurol 37:395–406. https://doi.org/10.1055/s-0037-1604351
N.A.S.M. Azmi, N. Juliana, S. Azmani, N.M. Effendy, I.F. Abu, N.I.M.F. Teng, S. Das, Cortisol on circadian rhythm and its effect on cardiovascular system, Int J Env Res Pub He 18 (2021). ARTN 676 https://doi.org/10.3390/ijerph18020676.
N.A.S.M. Azmi, N. Juliana, N.I.M.F. Teng, S. Azmani, S. Das, N. Effendy, Consequences of circadian disruption in shift workers on chrononutrition and their psychosocial well-being, Int J Env Res Pub He 17 (2020). ARTN 2043 https://doi.org/10.3390/ijerph17062043.
Ingelsson E, Bjorklund-Bodegard K, Lind L, Arnlov J, Sundstrom J (2006) Diurnal blood pressure pattern and risk of congestive heart failure. Jama-J Am Med Assoc 295:2859–2866. https://doi.org/10.1001/jama.295.24.2859
Gourine A, Gourine AV (2014) Neural mechanisms of cardioprotection. Physiology 29:133–140. https://doi.org/10.1152/physiol.00037.2013
Wood PA, Yang XM, Hrushesky WJM (2009) Clock genes and cancer. Integr Cancer Ther 8:303–308. https://doi.org/10.1177/1534735409355292
Funding
This study was funded by the National Natural Science Foundation of China (Grant Numbers 81974098, 81770756) and Program from Department of Science and Technology of Sichuan Province (Grant Number 2020YJ0054), Post-Doctor Research Project, West China Hospital, Sichuan University (Grant Number 2019HXBH089), and Health Commission of Sichuan province (20PJ036).
Author information
Authors and Affiliations
Contributions
JL and DHC searched, collected, analyzed the data, and wrote the manuscript. LRL and QW designed the study, supervised the project, and revised the manuscript. BC and YH assisted with detailed statistical analysis. ZYC, RYW, and QD helped with data extraction. All authors read and approved the final draft.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jin Li and Dehong Cao are Equal study contribution.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, J., Cao, D., Huang, Y. et al. Sleep duration and health outcomes: an umbrella review. Sleep Breath 26, 1479–1501 (2022). https://doi.org/10.1007/s11325-021-02458-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02458-1