Abstract
Objectives
The NoSAS score has been shown to be a reliable screening tool for obstructive sleep apnea (OSA) in overall populations. This study aimed to explore the effects of age and sex on the predicting performance of this score.
Methods
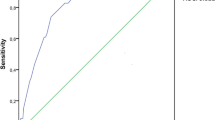
A retrospective analysis was conducted on 1119 subjects aged ≥ 18 years and with a total sleep time of ≥ 4 h during overnight polysomnography. Discrimination was assessed by using areas under receiver operating characteristic curve (AUCs), while predictive parameters were calculated by using contingency tables.
Results
Overall, a NoSAS score of 8 points or higher resulted in sensitivity, specificity, and AUC for predicting an apnea−hypopnea index (AHI) of ≥ 20 events/h of 74%, 36%, and 0.63 (in non-elderly 73%, 46%, and 0.65; in elderly 91%, 17%, and 0.59; in men 85%, 18%, and 0.56; in women 52%, 76%, and 0.71, respectively). The AUCs at all AHI cutoffs were significantly lower in men than in women (all with p < 0.01), while the AUCs at AHI cutoff of 5, 15, and 30 events/h were significantly lower in elderly than in non-elderly (p < 0.01, 0.05, and 0.05, respectively). In non-elderly, a conventional NoSAS with cutoff of 7 or a modified NoSAS with age cutoff of 50 years provided sensitivity and specificity for predicting an AHI of ≥ 20 events/h of 87%, 37% and 80%, 36%, respectively, with comparable AUCs. In women, a conventional NoSAS with cutoff of 6 or a modified NoSAS with neck circumference cutoff of 35 cm provided sensitivity and specificity for predicting an AHI of ≥ 20 events/h of 85%, 39% and 79%, 52%, respectively, with comparable AUCs.
Conclusions
NoSAS score has better discrimination but lower sensitivity for predicting OSA in non-elderly and women than in their counterparts. Age- and sex-specific cutoff values reverse this imbalance. Our results underline the preference of age- and sex-specific cutoff values and the need for better age- and sex-specific screening algorithms.



Similar content being viewed by others
Data availability
Not applicable.
References
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014. https://doi.org/10.1093/aje/kws342
McNicholas WT, Bonsignore MR (2007) Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J 29:156–178. https://doi.org/10.1183/09031936.00027406
Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, Nieto FJ, Stubbs R, Hla KM (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31:1071–1078
Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G (2013) Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol 62:569–576. https://doi.org/10.1016/j.jacc.2013.05.045
Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR (2008) Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 31:1079–1085
Young T, Evans L, Finn L, Palta M (1997) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 20:705–706. https://doi.org/10.1093/sleep/20.9.705
Marti-Soler H, Hirotsu C, Marques-Vidal P, Vollenweider P, Waeber G, Preisig M, Tafti M, Tufik SB, Bittencourt L, Tufik S, Haba-Rubio J, Heinzer R (2016) The NoSAS score for screening of sleep-disordered breathing: a derivation and validation study. Lancet Respir Med 4:742–748. https://doi.org/10.1016/S2213-2600(16)30075-3
Tan A, Hong Y, Tan LWL, van Dam RM, Cheung YY, Lee CH (2017) Validation of NoSAS score for screening of sleep-disordered breathing in a multiethnic Asian population. Sleep Breath 21:1033–1038. https://doi.org/10.1007/s11325-016-1455-4
Hong C, Chen R, Qing S, Kuang A, Yang H, Su X, Zhao D, Wu K, Zhang N (2018) Validation of the NoSAS score for the screening of sleep-disordered breathing: a hospital-based retrospective study in China. J Clin Sleep Med 14:191–197. https://doi.org/10.5664/jcsm.6930
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:597–619. https://doi.org/10.5664/jcsm.2172
Lee RW, Vasudavan S, Hui DS, Prvan T, Petocz P, Darendeliler MA, Cistulli PA (2010) Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep 33:1075–1080. https://doi.org/10.1093/sleep/33.8.1075
Li KK, Kushida C, Powell NB, Riley RW, Guilleminault C (2000) Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope 110:1689–1693. https://doi.org/10.1097/00005537-200010000-00022
Topirceanu A, Udrescu M, Udrescu L, Ardelean C, Dan R, Reisz D, Mihaicuta S (2018) SAS score: targeting high-specificity for efficient population-wide monitoring of obstructive sleep apnea. PLoS One 13:e0202042. https://doi.org/10.1371/journal.pone.0202042
Horvath CM, Jossen J, Kröll D, Nett PC, Baty F, Brill AK, Ott SR (2018) Prevalence and prediction of obstructive sleep apnea prior to bariatric surgery—gender-specific performance of four sleep questionnaires. Obes Surg 28:2720–2726. https://doi.org/10.1007/s11695-018-3222-z
Duarte RLM, Mello FC, Magalhaes-da-Silveira FJ, Oliveira-E-Sa TS, Rabahi MF, Gozal D (2019) Comparative performance of screening instruments for obstructive sleep apnea in morbidly obese patients referred to a sleep laboratory: a prospective cross-sectional study. Sleep Breath 23:1123–1132. https://doi.org/10.1007/s11325-019-01791-w
Bauters FA, Loof S, Hertegonne KB, Chirinos HA, De Buyzere ML, Rietzschel ER (2020) Sex-specific sleep apnea screening questionnaires: closing the performance gap in women. Sleep Med 67:91–98. https://doi.org/10.1016/j.sleep.2019.10.023
Mohsenin V (2003) Effects of gender on upper airway collapsibility and severity of obstructive sleep apnea. Sleep Med 4:523–529. https://doi.org/10.1016/s1389-9457(03)00168-0
Subramanian S, Jayaraman G, Majid H, Aguilar R, Surani S (2012) Influence of gender and anthropometric measures on severity of obstructive sleep apnea. Sleep Breath 16:1091–1095. https://doi.org/10.1007/s11325-011-0607-9
Gabbay IE, Lavie P (2012) Age- and gender-related characteristics of obstructive sleep apnea. Sleep Breath 16:453–460. https://doi.org/10.1007/s11325-011-0523-z
Basoglu OK, Tasbakan MS (2018) Gender differences in clinical and polysomnographic features of obstructive sleep apnea: a clinical study of 2827 patients. Sleep Breath 22:241–249. https://doi.org/10.1007/s11325-017-1482-9
Shah N, Hanna DB, Teng Y, Sotres-Alvarez D, Hall M, Loredo JS, Zee P, Kim M, Yaggi HK, Redline S, Kaplan RC (2016) Sex-specific prediction models for sleep apnea from the Hispanic Community Health Study/Study of Latinos. Chest 149:1409–1418. https://doi.org/10.1016/j.chest.2016.01.013
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, Kales A (2001) Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med 163:608–613. https://doi.org/10.1164/ajrccm.163.3.9911064
Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A (1998) Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med 157:144–148. https://doi.org/10.1164/ajrccm.157.1.9706079
Rutjes AW, Reitsma JB, Vandenbroucke JP, Glas AS, Bossuyt PM (2005) Case-control and two-gate designs in diagnostic accuracy studies. Clin Chem 51:1335–1341. https://doi.org/10.1373/clinchem.2005.048595
Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP (2001) The continuing epidemics of obesity and diabetes in the United States. JAMA 286:1195–1200. https://doi.org/10.1001/jama.286.10.1195
Malhotra A, Huang Y, Fogel R, Lazic S, Pillar G, Jakab M, Kikinis R, White DP (2006) Aging influences on pharyngeal anatomy and physiology: the predisposition to pharyngeal collapse. Am J Med 119:72e9–7e14. https://doi.org/10.1016/j.amjmed.2005.01.077
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Zhigang Zhang, Dan Yang, and Haiying Wang. The first draft of the manuscript was written by Zhigang Zhang. The draft was reviewed and edited by Zhigang Zhang and Xinmin Liu. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study protocol was approved by the Ethics Committee of Peking University First Hospital and waived the patient consent requirement.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, Z., Yang, D., Wang, H. et al. Effects of age and sex on the performance of the NoSAS score as a screening tool for obstructive sleep apnea: a hospital-based retrospective study in China. Sleep Breath 25, 1407–1417 (2021). https://doi.org/10.1007/s11325-020-02254-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02254-3