Abstract
Background
Limited data suggest that health literacy (HL) is associated with kidney functions and clinical outcomes in patients with non-dialysis chronic kidney disease (CKD). We aimed to identify factors associated with the level of HL in a CKD population that has not been studied previously.
Methods
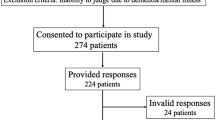
Patients with stage I–V (non-dialysis) CKD according to the Kidney Disease Outcomes Quality Initiative classification were enrolled in the study from two tertiary healthcare centers. Data were collected cross-sectionally using the European Health Literacy Survey (HLS-EU).
Results
Data of 208 participants were analyzed. HLS-EU scores had the highest correlations with age (r = − 0.494, p = 0.0001) and education (r = 0.476, p = 0.0001). Estimated glomerular filtration rate (e-GFR) was significantly correlated with HLS-EU score (r = 0.186, p = 0.01). Presence of a self-reported acquaintance with any kind of kidney disease was associated with higher HL. On the other hand, participants with multiple comorbidities, and therefore with more frequent contact with the health system, had lower HL than those without such frequent contact. Similarly, those with a high disease burden had lower HL than those without. HLS-EU scores were also significantly associated with gender, marital status, occupational status, self-perception of health, restriction of daily activities, participation in social activities, place of residence, blood pressure, body mass index, and serum parathyroid hormone and albumin levels.
Conclusion
Low HL is prevalent among CKD patients and is associated with e-GFR. Presence of an acquaintance with any kind of kidney disease is positively associated with HL. Presence of multiple comorbidities might be a limiting factor for the improvement of HL, which might also be expected to improve as a result of frequent contact with healthcare providers.

Similar content being viewed by others
Data availability
The data of this article are available within the article itself and in its online supplementary material.
References
Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H (2012) (HLS-EU) Consortium Health Literacy Project European. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 12:80. https://doi.org/10.1186/1471-2458-12-80. PMID: 22276600; PMCID: PMC3292515
Nutbeam D, McGill B, Premkumar P (2018) Improving health literacy in community populations: a review of progress. Health Promot Int 33(5):901–911. https://doi.org/10.1093/heapro/dax015
Elisabeth Stømer U, Klopstad Wahl A, Gunnar Gøransson L, Hjorthaug UK (2020) Health literacy in kidney disease: associations with quality of life and adherence. J Ren Care 46(2):85–94. https://doi.org/10.1111/jorc.12314
Green JA, Mor MK, Shields AM et al (2013) Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. Am J Kidney Dis 62(1):73–80. https://doi.org/10.1053/j.ajkd.2012.12.014
Taylor DM, Fraser S, Dudley C et al (2018) Health literacy and patient outcomes in chronic kidney disease: a systematic review. Nephrol Dial Transplant 33(9):1545–1558. https://doi.org/10.1093/ndt/gfx293
Cavanaugh KL, Wingard RL, Hakim RM et al (2010) Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol 21(11):1979–1985. https://doi.org/10.1681/ASN.2009111163
Jain D, Green JA (2016) Health literacy in kidney disease: Review of the literature and implications for clinical practice. World J Nephrol 5(2):147. https://doi.org/10.5527/wjn.v5.i2.147
Ricardo AC, Yang W, Lora CM et al (2014) Limited health literacy is associated with low glomerular filtration in the chronic renal insufficiency cohort (cric) study. Clin Nephrol 81(1):30–37. https://doi.org/10.5414/CN108062
Devraj R, Borrego M, Vilay AM, Gordon EJ, Pailden J, Horowitz B (2015) Relationship between health literacy and kidney function. Nephrology 20(5):360–367. https://doi.org/10.1111/nep.12425
Schrauben SJ, Cavanaugh KL, Fagerlin A et al (2020) The relationship of disease-specific knowledge and health literacy with the uptake of self-care behaviors in CKD. Kidney Int Reports 5(1):48–57. https://doi.org/10.1016/j.ekir.2019.10.004
Taylor DM, Bradley JA, Bradley C et al (2016) Limited health literacy in advanced kidney disease. Kidney Int 90(3):685–695. https://doi.org/10.1016/j.kint.2016.05.033
K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification-PubMed. https://pubmed.ncbi.nlm.nih.gov/11904577/. Accessed 17 June 2020
Ozdemir H, Alper Z, Uncu Y, Bilgel N (2010) Health literacy among adults: A study from Turkey. Health Educ Res 25(3):464–477. https://doi.org/10.1093/her/cyp068
Durusu-Tanrıöver M, Yildirim HH, Demiray-Ready FN, Çakir B ve Akalin HE (2014). Türkiye Sağlık Okuryazarlığı Araştırması (Turkey Health Literacy Survey), Birinci Baskı, Sağlık-Sen Yayınları (Saglik-Sen Union Publication), Ankara. Acc-Google’da Ara. https://www.google.com/search?source=hp&ei=YtjpXqT5DY243AP15bCwDw&q=Durusu-Tanrıöver+M%2C+Yildirim+HH%2C+Demiray-Ready+FN%2C+Çakir+B+ve+Akalin+HE+%282014%29.+Türkiye+Sağlık+Okuryazarlığı+Araştırması+%28Turkey+Health+Literacy+Survey%29%2C+Birinci+Baskı%2C+Sağlık-Sen+Yayınları+%28Saglik-Sen+Union+Publication%29%2C+Ankara.+Acc&oq=Durusu-Tanrıöver+M%2C+Yildirim+HH%2C+Demiray-Ready+FN%2C+Çakir+B+ve+Akalin+HE+%282014%29.+Türkiye+Sağlık+Okuryazarlığı+Araştırması+%28Turkey+Health+Literacy+Survey%29%2C+Birinci+Baskı%2C+Sağlık-Sen+Yayınları+%28Saglik-Sen+Union+Publication%29%2C+Ankara.+Acc&gs_lcp=CgZwc3ktYWIQA1CkBlikBmCZFWgAcAB4AIABAIgBAJIBAJgBAaABAqABAaoBB2d3cy13aXo&sclient=psy-ab&ved=0ahUKEwiksoOQu4jqAhUNHHcKHfUyDPYQ4dUDCAc&uact=5. Accessed 17 June 2020
Sørensen K, Pelikan JM, Röthlin F et al (2015) Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health 25(6):1053–1058. https://doi.org/10.1093/eurpub/ckv043
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 130(6):461–470. https://doi.org/10.7326/0003-4819-130-6-199903160-00002
Taylor DM, Fraser SDS, Bradley JA et al (2017) A systematic review of the prevalence and associations of limited health literacy in CKD. Clin J Am Soc Nephrol 12(7):1070–1084. https://doi.org/10.2215/CJN.12921216
Stømer UE, Gøransson LG, Wahl AK, Urstad KH (2019) A cross-sectional study of health literacy in patients with chronic kidney disease: Associations with demographic and clinical variables. Nurs Open 6(4):1481–1490. https://doi.org/10.1002/nop2.350
Liu YB, Hou P, Xue HP, Mao XE, Li YN (2019) Social support, health literacy, and health care utilization among older adults. Asia-Pac J Public Health 31(4):359–366. https://doi.org/10.1177/1010539519851674
Friis K, Lasgaard M, Osborne RH, Maindal HT (2016) Gaps in understanding health and engagement with healthcare providers across common long-term conditions: a population survey of health literacy in 29 473 Danish citizens. BMJ Open. https://doi.org/10.1136/bmjopen-2015-009627
Palmer S, Vecchio M, Craig JC et al (2013) Prevalence of depression in chronic kidney disease: Systematic review and meta-analysis of observational studies. Kidney Int 84(1):179–191. https://doi.org/10.1038/ki.2013.77
Bautovich A, Katz I, Smith M, Loo CK, Harvey SB (2014) Depression and chronic kidney disease: A review for clinicians. Aust N Z J Psychiatry 48(6):530–541. https://doi.org/10.1177/0004867414528589
Yaffe K, Kurella-Tamura M, Ackerson L et al (2014) Higher levels of cystatin C are associated with worse cognitive function in older adults with chronic kidney disease: the chronic renal insufficiency cohort cognitive study. J Am Geriatr Soc 62(9):1623–1629. https://doi.org/10.1111/jgs.12986
Hailpern SM, Melamed ML, Cohen HW, Hostetter TH (2007) Moderate chronic kidney disease and cognitive function in adults 20 to 59 years of age: Third National Health and Nutrition Examination Survey (NHANES III). J Am Soc Nephrol 18(7):2205–2213. https://doi.org/10.1681/ASN.2006101165
Kurella M, Chertow GM, Fried LF et al (2005) Chronic kidney disease and cognitive impairment in the elderly: the Health, Aging, and Body Composition study. J Am Soc Nephrol 16(7):2127–2133. https://doi.org/10.1681/ASN.2005010005
Wong KK, Velasquez A, Powe NR, Tuot DS (2018) Association between health literacy and self-care behaviors among patients with chronic kidney disease. BMC Nephrol 19(1):1–8. https://doi.org/10.1186/s12882-018-0988-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have a conflict of interest. Results presented in this paper have not been published previously in whole or in part, except in abstract form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Demir, N., Koz, S. & Ugurlu, C.T. Health literacy in chronic kidney disease patients: association with self-reported presence of acquaintance with kidney disease, disease burden and frequent contact with health care provider. Int Urol Nephrol 54, 2295–2304 (2022). https://doi.org/10.1007/s11255-022-03124-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03124-5