Abstract
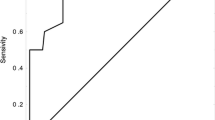
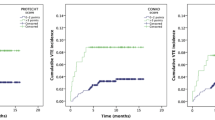
Cancer patients are at higher risk for venous thromboembolism (VTE). Several risk assessment models (RAM), including the Khorana and COMPASS-CAT, were developed to help predict the occurrence of VTE in cancer patients on active anti-cancer therapy. We aim to study the prevalence and predictors of VTE among patients with non-small cell lung cancer (NSCLC) and compare both RAMs in predicting VTE in patients with NSCLC were retrospectively reviewed. Variables known to increase the risk of VTE were collected and risk of VTE was assessed using both Khorana and COMPASS-CAT RAM. A total of 508 patients (mean age ± SD, 58.4 ± 12.2 years) were enrolled. Most (n = 357, 70.3%) patients had adenocarcinoma, and 333 (65.6%) patients had metastatic disease. VTE were confirmed in 76 (15.0%) patients. Rates were higher among patients with metastatic disease (19.8%, p < 0.001), adenocarcinoma (17.4%, p = 0.01) and those treated with immunotherapy (23.5%, p = 0.014). VTE rates were 21.2%, 14.1% and 13.9% among those with high (n = 66), intermediate (n = 341) and low (n = 101) Khorana risk scores, respectively (p = 0.126). On the other hand, 190 (37.4%) were classified as high risk by the COMPASS-CAT RAM; 52 (27.4%) of them had VTE compared to 24 (7.5%) of the remaining 318 (62.6%) classified as Low/Intermediate risk level, p < 0.001. In conclusion, patients with NSCLC are at high risk for VTE, especially those with adenocarcinoma, metastatic disease and when treated with immunotherapy. Compared to Khorana RAM, COMPASS-CAT RAM was better in identifying more patients in high-risk group, with higher VTE rate.
Key points
-
VTE rates in patients with lung cancer is relatively high; more so with metastatic disease and in patients with adenocarcinoma.
-
Molecular alterations have no effect on VTE rates; however, use of immunotherapy is associated with higher rates.
-
COMPASS-CAT RAM is better than Khorana RAM in segregating patients into different risk levels.


Similar content being viewed by others
Data Availability
All data and materials are available from the corresponding authors upon written request.
References
Prandoni P, Falanga A, Piccioli A (2005) Cancer and venous thromboembolism. Lancet Oncol 6:401–410. https://doi.org/10.1016/S1470-2045(05)70207-2
Horsted F, West J, Grainge MJ (2012) Risk of venous thromboembolism in patients with cancer: a systematic review and meta-analysis. PLoS Med 9. https://doi.org/10.1371/journal.pmed.1001275
Ay C, Pabinger I, Cohen AT (2017) Cancer-associated venous thromboembolism: Burden, mechanisms, and management. Thromb Haemost 117:219–230. https://doi.org/10.1160/TH16-08-0615
Khorana AA, Mackman N, Falanga A (2022) Cancer-associated venous thromboembolism. Nat Rev Dis Primers 8:11. https://doi.org/10.1038/s41572-022-00336-y
Gade IL, Braekkan SK, Naess IA (2017) The impact of initial cancer stage on the incidence of venous thromboembolism: the scandinavian thrombosis and Cancer (STAC) cohort. J Thromb Haemost 15:1567–1575. https://doi.org/10.1111/jth.13752
Khorana AA, Francis CW, Culakova E, Lyman GH (2005) Risk factors for chemotherapy-associated venous thromboembolism in a prospective observational study. Cancer 104:2822–2829. https://doi.org/10.1002/cncr.21496
Abdel-Razeq H, Mansour A, Abdulelah H (2018) Thromboembolic events in cancer patients on active treatment with cisplatin-based chemotherapy: another look! Thromb J. https://doi.org/10.1186/s12959-018-0161-9. 16, 2:
Falanga A, Brenner B, Khorana AA, Francis CW (2022) Thrombotic complications in patients with cancer: advances in pathogenesis, prevention, and treatment-A report from ICTHIC 2021. https://doi.org/10.1002/rth2.12744. Res Pract Thromb Haemost 6:
Moik F, Chan WE, Wiedemann S (2021) Incidence, risk factors, and outcomes of venous and arterial thromboembolism in immune checkpoint inhibitor therapy. Blood 137:1669–1678. https://doi.org/10.1182/blood.2020007878
Sussman TA, Li H, Hobbs B et al (2021) Incidence of thromboembolism in patients with melanoma on immune checkpoint inhibitor therapy and its adverse association with survival. J Immunother Cancer 9. https://doi.org/10.1136/jitc-2020-001719
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72:7–33. https://doi.org/10.3322/caac.21708
Lung Cancer Fact Sheet (2023) American lung association. Available at: https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/resource-library/lung-cancer-fact-sheet. Accessed 29
Numico G, Garrone O, Dongiovanni V (2005) Prospective evaluation of major vascular events in patients with nonsmall cell lung carcinoma treated with cisplatin and gemcitabine. Cancer 103:994–999. https://doi.org/10.1002/cncr.20893
Song C, Shargall Y, Li H (2019) Prevalence of venous thromboembolism after lung surgery in China: a single-centre, prospective cohort study involving patients undergoing lung resections without perioperative venous thromboembolism prophylaxis†. Eur J Cardiothorac Surg 55:455–460. https://doi.org/10.1093/ejcts/ezy323
Dong H, Liang X, Gao Y (2022) Postoperative venous thromboembolism after surgery for stage IA non-small-cell lung cancer: a single-center, prospective cohort study. Thorac Cancer 13:1258–1266. https://doi.org/10.1111/1759-7714.14373
Hicks LK, Cheung MC, Ding K (2009) Venous thromboembolism and nonsmall cell lung cancer: a pooled analysis of National Cancer Institute of Canada clinical trials Group trials. Cancer 115:5516–5525. https://doi.org/10.1002/cncr.24596
Abdel-Razeq H, Mansour A, Saadeh SS (2018) The application of current proposed venous thromboembolism risk assessment model for ambulatory patients with cancer. Clin Appl Thromb Hemost 24:429–433. https://doi.org/10.1177/1076029617692880
Khorana AA, Dalal M, Lin J, Connolly GC (2013) Incidence and predictors of venous thromboembolism (VTE) among ambulatory high-risk cancer patients undergoing chemotherapy in the United States. Cancer 119:648–655. https://doi.org/10.1002/cncr.27772
Falanga A, Gal GL, Carrier M (2021) Management of Cancer-Associated thrombosis: unmet needs and future perspectives. TH Open 5. https://doi.org/10.1055/s-0041-1736037
Rutjes AW, Porreca E, Candeloro M et al (2020) Primary prophylaxis for venous thromboembolism in ambulatory cancer patients receiving chemotherapy. Cochrane Database Syst Rev 12:008500. https://doi.org/10.1002/14651858
Gerotziafas GT, Mahé I, Lefkou E (2020) Overview of risk assessment models for venous thromboembolism in ambulatory patients with cancer. Thromb Res 191 Suppl 150–57. https://doi.org/10.1016/S0049-3848(20)30397-2
Abdel-Razeq H, Ma’koseh M, Abdel-Razeq R et al (2021) The application of the lymphoma international prognostic index to predict venous thromboembolic events in diffuse large B-cell lymphoma patients. Front Oncol 11:677776
Khorana AA, Kuderer NM, Culakova E et al (2008) Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111:4902–4907. https://doi.org/10.1182/blood-2007-10-116327
Mulder FI, Candeloro M, Kamphuisen PW (2019) The Khorana score for prediction of venous thromboembolism in cancer patients: a systematic review and meta-analysis. Haematologica 104:1277–1287. https://doi.org/10.3324/haematol.2018.209114
Gerotziafas GT, Taher A, Abdel-Razeq H (2017) A predictive score for thrombosis Associated with breast, colorectal, lung, or ovarian Cancer: the prospective COMPASS-Cancer-Associated thrombosis study. Oncologist 22:1222–1231. https://doi.org/10.1634/theoncologist.2016-0414
Sung H, Ferlay J, Siegel RL, Global Cancer Statistics et al (2020) GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Fuentes HE, Tafur AJ, Caprini JA (2016) Cancer-associated thrombosis. Dis Mon 62:121–158. https://doi.org/10.1016/j.disamonth.2016.03.003
Kourelis TV, Wysokinska EM, Wang Y et al (2014) Early venous thromboembolic events are associated with worse prognosis in patients with lung cancer. Lung Cancer 86:358–362. https://doi.org/10.1016/j.lungcan.2014.10.003
Jin YF, Ye YQ, Jin YJ (2022) Risk factors and impact on outcomes of Lung Cancer Patients concurrent with deep vein thrombosis. Cancer Control 29:10732748221145074. https://doi.org/10.1177/10732748221145074
Howlett J, Benzenine E, Cottenet J et al (2020) Could venous thromboembolism and major bleeding be indicators of lung cancer mortality? A nationwide database study. BMC Cancer 20:461. https://doi.org/10.1186/s12885-020-06930-1
Sun L, Aggarwal C (2020) Immunotherapy for lung Cancer-improving outcomes in patients with locally Advanced Non-Small Cell Lung Cancer with Immunotherapy. Cancer J 26:548–554. https://doi.org/10.1097/PPO.0000000000000485
Luciani A, Ghidini A, Borgonovo K et al (2022) Outcome of non-small-cell lung cancer with driven mutations treated with anti-PD-(L)1 agents: a systematic review. Tumori 3008916221122601. https://doi.org/10.1177/03008916221122601
Reck M, Garassino MC, Imbimbo M (2018) Antiangiogenic therapy for patients with aggressive or refractory advanced non-small cell lung cancer in the second-line setting. Lung Cancer 120:62–69. https://doi.org/10.1016/j.lungcan.2018.03.025
Guo Q, Liu L, Chen Z (2022) Current treatments for non-small cell lung cancer. Front Oncol 12:945102. https://doi.org/10.3389/fonc.2022.945102
Mansfield AS, Tafur AJ, Wang CE et al (2016) Predictors of active cancer thromboembolic outcomes: validation of the Khorana score among patients with lung cancer. J Thromb Haemost 14:1773–1778. https://doi.org/10.1111/jth.13378
Nishimura A, Ikeda Y (2021) Yakugaku Zasshi 141:611–622. https://doi.org/10.1248/yakushi.20-00228
Wang Y, Attar BM, Fuentes HE et al (2018) Performance of Khorana risk score for prediction of venous thromboembolism in patients with hepatocellular carcinoma. Clin Appl Thromb Hemost 24:471–476. https://doi.org/10.1177/1076029617699088
VF NE F, S M, et al (2017) The Khorana score for the prediction of venous thromboembolism in patients with pancreatic cancer. Thromb Res 150:30–32. https://doi.org/10.1016/j.thromres.2016.12.013
Alma S, Eloi D, Léa V (2022) Incidence of venous thromboembolism and discriminating capacity of Khorana score in lung cancer patients treated with immune checkpoint inhibitors. J Thromb Thrombolysis 54:287–294. https://doi.org/10.1007/s11239-022-02649-x
Thawani R, Kartika T, Elstrott B (2022) Association of PD-L1 expression, tumor mutational burden and immunotherapy with venous thrombosis in patients with solid organ malignancies. Thromb Res 217:12–14. https://doi.org/10.1016/j.thromres.2022.06.012
Malka D, Girard N, Smadja DM (2022) Prévention et prise en charge des thromboses associées au cancer: questions pratiques à propos de l’anticoagulation [Prophylaxis and management of cancer-associated thrombosis: Practical issues about anticoagulant use. Bull Cancer 0007-4551 22 00424–6. https://doi.org/10.1016/j.bulcan.2022.10.008
Acknowledgements
The authors would like to acknowledge and thanks Mrs. Ayat Taqash for her help in preparing the statistical analysis.
Funding
This work was not funded.
Author information
Authors and Affiliations
Contributions
HAR and MJA conceived and designed the study. BS,HAF,RB,MAS,HAJ,DAL,OS,FT, KA,TS,RZ,YH collected the data. HAR, MJA, BS, HAF,RB analyzed and interpreted the data. HAF, RB performed the statistical analysis. HAR, BS, MJA drafted the manuscript. HAR, BS, RB supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics approval and consent to participate
This study was presented in-part as an oral presentation during the 30th Congress of the International Society on Thrombosis and Hemostasis (ISTH). London, UK. 9–13 July, 2022.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abdel-Razeq, H., Sharaf, B., Al-Jaghbeer, M.J. et al. COMPASS-CAT versus Khorana risk assessment model for predicting venous thromboembolic events in patients with non-small cell lung cancer on active treatment with chemotherapy and/or immunotherapy, the CK-RAM study. J Thromb Thrombolysis 56, 447–453 (2023). https://doi.org/10.1007/s11239-023-02860-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-023-02860-4