Abstract
Background
After treatment, high residual platelet reactivity (HRPR) is considered as an essential risk factor for recurrent ischemic events.
Aim
To evaluate the impact of fibrinogen on HRPR after implantation of emergency drug-eluting stents (DES) in patients treated with aspirin and clopidogrel or ticagrelor due to ST-elevation myocardial infarction (STEMI) and to explore the predictive values of HRPR and fibrinogen for adverse ischemic events at 12 months.
Method
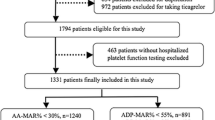
This single-center prospective observational study analyzed patients with STEMI who underwent primary percutaneous coronary intervention (PCI) with second-generation DES implantation from January 2017 to December 2018. Platelet reactivity was measured by thromboelastography (TEG) at 60–72 h after primary PCI. HRPR was defined as the adenosine diphosphate-induced maximum amplitude (MAADP) > 47 mm.
Results
A total of 919 patients were analyzed, of which 512 (55.8%) received aspirin and clopidogrel and 406 (44.2%) received aspirin and ticagrelor. Elevated fibrinogen levels were associated with an increased prevalence of HRPR (P < 0.001). High fibrinogen (quartile IV, ≥ 410 mg/dL) was an independent risk factor for HRPR after multivariate regression (odds ratio 6.556, 95% confidence interval [CI]: 3.200–13.431, P < 0.001). When analyzed by Kaplan–Meier survival curves, the combination of high fibrinogen and HRPR was strongly predictive for ischemic major adverse cardiac events at 12 months compared to the group without HRPR and with low fibrinogen (hazard ratio 9.681, 95% CI: 4.467–20.98, log-rank P < 0.001). Similar results were confirmed in subgroups according to different dual antiplatelet therapies.
Conclusion
A combination of high fibrinogen and HRPR may identify recurrent adverse ischemic events over 12 months. Ticagrelor exhibited more potent platelet inhibition and a better prognosis than clopidogrel.



Similar content being viewed by others
References
Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet Therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients with Non-ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation. 2016;134:e123–55. https://doi.org/10.1161/cir.0000000000000404.
Bonello L, Tantry US, Marcucci R, et al. Consensus and future directions on the definition of high on-treatment platelet reactivity to adenosine diphosphate. J Am Coll Cardiol. 2010;56:919–33. https://doi.org/10.1016/j.jacc.2010.04.047.
Tantry US, Bonello L, Aradi D, et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol. 2013;62:2261–73. https://doi.org/10.1016/j.jacc.2013.07.101.
Tang YD, Wang W, Yang M, et al. Randomized comparisons of double-dose clopidogrel or adjunctive cilostazol versus standard dual antiplatelet in patients with high posttreatment platelet reactivity: results of the CREATIVE trial. Circulation. 2018;137:2231–45. https://doi.org/10.1161/circulationaha.117.030190.
Breddin HK. Can platelet aggregometry be standardized? Platelets. 2005;16:151–8. https://doi.org/10.1080/09537100400020161.
Dunning J, Versteegh M, Fabbri A, et al. Guideline on antiplatelet and anticoagulation management in cardiac surgery. Eur J Cardiothorac Surg. 2008;34:73–92. https://doi.org/10.1016/j.ejcts.2008.02.024.
Gurbel PA, Bliden KP, Navickas IA, et al. Adenosine diphosphate-induced platelet-fibrin clot strength: a new thrombelastographic indicator of long-term poststenting ischemic events. Am Heart J. 2010;160:346–54. https://doi.org/10.1016/j.ahj.2010.05.034.
Rechner AR. Platelet function testing in clinical diagnostics. Hamostaseologie. 2011;31:79–87. https://doi.org/10.5482/ha-1133.
Rali AS, Salem AM, Gebre M, et al. Viscoelastic haemostatic assays in cardiovascular critical care. Card Fail Rev. 2020;7:e01. https://doi.org/10.15420/cfr.2020.22.
Nguyen TA, Diodati JG, Pharand C. Resistance to clopidogrel: a review of the evidence. J Am Coll Cardiol. 2005;45:1157–64. https://doi.org/10.1016/j.jacc.2005.01.034.
Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045–57. https://doi.org/10.1056/NEJMoa0904327.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–77. https://doi.org/10.1093/eurheartj/ehx393.
Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289–367. https://doi.org/10.1093/eurheartj/ehaa575.
Bliden KP, Tantry US, Storey RF, et al. The effect of ticagrelor versus clopidogrel on high on-treatment platelet reactivity: combined analysis of the ONSET/OFFSET and RESPOND studies. Am Heart J. 2011;162:160–5. https://doi.org/10.1016/j.ahj.2010.11.025.
Verdoia M, Sartori C, Pergolini P, et al. Prevalence and predictors of high-on treatment platelet reactivity with ticagrelor in ACS patients undergoing stent implantation. Vasc Pharmacol. 2016;77:48–53. https://doi.org/10.1016/j.vph.2015.04.014.
Cavallari I, Nusca A, Ricottini E, et al. Prognostic role of platelet reactivity in patients with acute coronary syndromes. Cardiol Rev. 2014;22:313–8. https://doi.org/10.1097/crd.0000000000000034.
Krintus M, Kozinski M, Kubica J, et al. Critical appraisal of inflammatory markers in cardiovascular risk stratification. Crit Rev Clin Lab Sci. 2014;51:263–79. https://doi.org/10.3109/10408363.2014.913549.
Kaski JC, Fernández-Bergés DJ, Consuegra-Sánchez L, et al. A comparative study of biomarkers for risk prediction in acute coronary syndrome-results of the SIESTA (Systemic Inflammation Evaluation in non-ST-elevation Acute coronary syndrome) study. Atherosclerosis. 2010;212:636–43. https://doi.org/10.1016/j.atherosclerosis.2010.06.026.
Kamath S, Lip GY. Fibrinogen: biochemistry, epidemiology and determinants. QJM. 2003;96:711–29. https://doi.org/10.1093/qjmed/hcg129.
Corrado E, Rizzo M, Coppola G, et al. An update on the role of markers of inflammation in atherosclerosis. J Atheroscler Thromb. 2010;17:1–11. https://doi.org/10.5551/jat.2600.
Ang L, Palakodeti V, Khalid A, et al. Elevated plasma fibrinogen and diabetes mellitus are associated with lower inhibition of platelet reactivity with clopidogrel. J Am Coll Cardiol. 2008;52:1052–9. https://doi.org/10.1016/j.jacc.2008.05.054.
Bennett JS. Platelet-fibrinogen interactions. Ann N Y Acad Sci. 2001;936:340–54. https://doi.org/10.1111/j.1749-6632.2001.tb03521.x.
Althoff TF, Fischer M, Langer E, et al. Sustained enhancement of residual platelet reactivity after coronary stenting in patients with myocardial infarction compared to elective patients. Thromb Res. 2010;125:e190–6. https://doi.org/10.1016/j.thromres.2010.01.003.
Ang L, Thani KB, Ilapakurti M, et al. Elevated plasma fibrinogen rather than residual platelet reactivity after clopidogrel pre-treatment is associated with an increased ischemic risk during elective percutaneous coronary intervention. J Am Coll Cardiol. 2013;61:23–34. https://doi.org/10.1016/j.jacc.2012.09.037.
Schoenfeld DA. Sample-size formula for the proportional-hazards regression model. Biometrics. 1983;39:499–503.
Tobbia P, Brodie BR, Witzenbichler B, et al. Adverse event rates following primary PCI for STEMI at US and non-US hospitals: three-year analysis from the HORIZONS-AMI trial. EuroIntervention. 2013;8:1134–42. https://doi.org/10.4244/eijv8i10a176.
Poudel I, Tejpal C, Rashid H, et al. Major adverse cardiovascular events: an inevitable outcome of ST-elevation myocardial infarction? A literature review. Cureus. 2019;11:e5280. https://doi.org/10.7759/cureus.5280.
Sawano M, Kohsaka S, Ishii H, et al. One-year outcome after percutaneous coronary intervention for acute coronary syndrome—An analysis of 20,042 patients from a Japanese nationwide registry. Circ J. 2021;85:1756–67. https://doi.org/10.1253/circj.CJ-21-0098.
Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011;306:1215–23. https://doi.org/10.1001/jama.2011.1332.
Parodi G, Bellandi B, Tarantini G, et al. Clinical events beyond one year after an acute coronary syndrome: insights from the RECLOSE 2-ACS study. EuroIntervention. 2017;12:2018–24. https://doi.org/10.4244/eij-d-16-00255.
Tang N, Yin S, Sun Z, et al. The relationship between on-clopidogrel platelet reactivity, genotype, and post-percutaneous coronary intervention outcomes in Chinese patients. Scand J Clin Lab Invest. 2015;75:223–9. https://doi.org/10.3109/00365513.2014.993696.
Zhao X, Wu H, Xu H, et al. Association between residual platelet reactivity on clopidogrel treatment and severity of coronary atherosclerosis: intrinsic hypercoagulability as a mediator. Adv Ther. 2019;36:2296–309. https://doi.org/10.1007/s12325-019-01032-2.
Li J, Yuan D, Jiang L, et al. Similar inflammatory biomarkers reflect different platelet reactivity in percutaneous coronary intervention patients treated with clopidogrel: a large-sample study from China. Front Cardiovasc Med. 2021;8:736466. https://doi.org/10.3389/fcvm.2021.736466.
Alfonso F, Byrne RA, Rivero F, et al. Current treatment of in-stent restenosis. J Am Coll Cardiol. 2014;63:2659–73. https://doi.org/10.1016/j.jacc.2014.02.545.
Cassese S, Byrne RA, Tada T, et al. Incidence and predictors of restenosis after coronary stenting in 10 004 patients with surveillance angiography. Heart. 2014;100:153–9. https://doi.org/10.1136/heartjnl-2013-304933.
Haybar H, Pezeshki SMS, Saki N. Platelets in in-stent restenosis: from fundamental role to possible prognostic application. Curr Cardiol Rev. 2020;16:285–91. https://doi.org/10.2174/1573403x15666190620141129.
Jiang Z, Zhang R, Sun M, et al. Effect of clopidogrel vs ticagrelor on platelet aggregation and inflammation markers after percutaneous coronary intervention for ST-elevation myocardial infarction. Can J Cardiol. 2018;34:1606–12. https://doi.org/10.1016/j.cjca.2018.08.024.
Guimarães PO, Tricoci P. Ticagrelor, prasugrel, or clopidogrel in ST-segment elevation myocardial infarction: which one to choose? Expert Opin Pharmacother. 2015;16:1983–95. https://doi.org/10.1517/14656566.2015.1074180.
Dong Z, Zhai H, Pan L, et al. Stronger inhibitory effects of Ticagrelor plus aspirin compared with Clopidogrel plus aspirin on arachidonic acid-induced platelet aggregation in patients with acute coronary syndrome with PCI. J Pak Med Assoc. 2021;71:540–2. https://doi.org/10.47391/jpma.029.
Adamski P, Buszko K, Sikora J, et al. Determinants of high platelet reactivity in patients with acute coronary syndromes treated with ticagrelor. Sci Rep. 2019;9:3924. https://doi.org/10.1038/s41598-019-40628-0.
Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–596. https://doi.org/10.1161/cir.0000000000000757.
Kreutz RP, Schmeisser G, Maatman B, et al. Fibrin clot strength measured by thrombelastography and outcomes after percutaneous coronary intervention. Thromb Haemost. 2017;117:426–8. https://doi.org/10.1160/th16-10-0496.
Biolik G, Gajniak D, Kubicz M, et al. The influence of inflammation on fibrinogen turnover and redistribution of the hemostatic balance to a prothrombotic state in high on-treatment platelet reactivity-dual poor responder (HTPR-DPR) patients. Mediat Inflamm. 2019;2019:3767128. https://doi.org/10.1155/2019/3767128.
Luyendyk JP, Schoenecker JG, Flick MJ. The multifaceted role of fibrinogen in tissue injury and inflammation. Blood. 2019;133:511–20. https://doi.org/10.1182/blood-2018-07-818211.
Kannel WB, Wolf PA, Castelli WP, et al. Fibrinogen and risk of cardiovascular disease. The Framingham study. JAMA. 1987;258:1183–6.
Nieuwdorp M, Stroes ES, Meijers JC, et al. Hypercoagulability in the metabolic syndrome. Curr Opin Pharmacol. 2005;5:155–9. https://doi.org/10.1016/j.coph.2004.10.003.
Surma S, Banach M. Fibrinogen and atherosclerotic cardiovascular diseases-review of the literature and clinical studies. Int J Mol Sci. 2021;23:193. https://doi.org/10.3390/ijms23010193.
Yang H, Lang S, Zhai Z, et al. Fibrinogen is required for maintenance of platelet intracellular and cell-surface P-selectin expression. Blood. 2009;114:425–36. https://doi.org/10.1182/blood-2008-03-145821.
Jaster M, Horstkotte D, Willich T, et al. The amount of fibrinogen-positive platelets predicts the occurrence of in-stent restenosis. Atherosclerosis. 2008;197:190–6. https://doi.org/10.1016/j.atherosclerosis.2007.03.020.
Tabakcı MM, Gerin F, Sunbul M, et al. Relation of plasma fibrinogen level with the presence, severity, and complexity of coronary artery disease. Clin Appl Thromb Hemost. 2017;23:638–44. https://doi.org/10.1177/1076029616629210.
Woo JS, Kim W, Jang HH, et al. Effect of platelet reactivity, endothelial function, and inflammatory status on outcomes in patients with stable angina pectoris on clopidogrel therapy. Am J Cardiol. 2014;113:786–92. https://doi.org/10.1016/j.amjcard.2013.11.025.
Campo G, Parrinello G, Ferraresi P, et al. Prospective evaluation of on-clopidogrel platelet reactivity over time in patients treated with percutaneous coronary intervention relationship with gene polymorphisms and clinical outcome. J Am Coll Cardiol. 2011;57:2474–83. https://doi.org/10.1016/j.jacc.2010.12.047.
Chatterjee M, Geisler T. Inflammatory contribution of platelets revisited: new players in the arena of inflammation. Semin Thromb Hemost. 2016;42:205–14. https://doi.org/10.1055/s-0035-1570081.
Gupta T, Kolte D, Khera S, et al. Smoker’s paradox in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. J Am Heart Assoc. 2016;5:e003370. https://doi.org/10.1161/jaha.116.003370.
Gurbel PA, Bliden KP, Logan DK, et al. The influence of smoking status on the pharmacokinetics and pharmacodynamics of clopidogrel and prasugrel: the PARADOX study. J Am Coll Cardiol. 2013;62:505–12. https://doi.org/10.1016/j.jacc.2013.03.037.
Gupta R, Kirtane AJ, Liu Y, et al. Impact of smoking on platelet reactivity and clinical outcomes after percutaneous coronary intervention: findings from the ADAPT-DES study. Circ Cardiovasc Interv. 2019;12:e007982. https://doi.org/10.1161/circinterventions.119.007982.
Bliden KP, Dichiara J, Lawal L, et al. The association of cigarette smoking with enhanced platelet inhibition by clopidogrel. J Am Coll Cardiol. 2008;52:531–3. https://doi.org/10.1016/j.jacc.2008.04.045.
Zhang L, Chen Y, Jin Y, et al. Genetic determinants of high on-treatment platelet reactivity in clopidogrel treated Chinese patients. Thromb Res. 2013;132:81–7. https://doi.org/10.1016/j.thromres.2013.05.006.
Marcucci R, Grifoni E, Giusti B. On-treatment platelet reactivity: state of the art and perspectives. Vascul Pharmacol. 2016;77:8–18. https://doi.org/10.1016/j.vph.2015.10.005.
Marcucci R, Giusti B, Paniccia R, et al. High on-treatment platelet reactivity by ADP and increased risk of MACE in good clopidogrel metabolizers. Platelets. 2012;23:586–93. https://doi.org/10.3109/09537104.2012.658106.
Acknowledgements
Shikun Xu and Qianzhou Lv contributed equally to this article as co-corresponding authors. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The author reports no conflicts of interest in this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yao, Y., Li, X., Wang, Z. et al. The impact of high on-treatment platelet reactivity and fibrinogen levels on ischemic events in patients with ST elevation myocardial infarction: a prospective observational study. Int J Clin Pharm 45, 461–472 (2023). https://doi.org/10.1007/s11096-022-01525-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-022-01525-1