Abstract
Background
Tinea capitis (TC) is one of the most common public health concerns due to its high incidence in preadolescent children. The epidemiological and clinical characteristics of TC vary depending on geographical regions and have changed over the past decades.
Objectives
This study aimed to identify epidemiological changes in recent decades, including the prevalence and clinical and mycological characteristics of TC in southern China.
Methods
We conducted a retrospective study at the Department of Dermatology of Sun Yat-sen Memorial Hospital, Sun Yat-sen University from June 1997 to August 2020.
Results
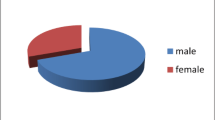
We retrospectively evaluated 401 TC patients. Of these, 157 patients (39.2%) were preschool children aged 3–7 years and the majority were males. However, the prevalence in children under 3 years old is on the rise (from 19.67% during 1997–2010 to 32.49% during 2011–2020). Grey patches were the most common clinical pattern and mostly occurred in children (71.3%), while the proportion of grey patches and black dots was almost the same in adults. Although Microsporum canis (76%) was the most common causative organism, the number of the T. mentagrophytes complex, as a zoophilic fungus, has increased more than that of the anthropophilic fungi T. violaceum in the recent decade. There was a significant difference in the portion of sex among different age groups, and the gender difference was more notable in the adult group, which showed that the TC prevalence in females was 9 times that in males. In males, M. canis and the T. mentagrophytes complex were the two most common causative fungi, while M. canis and T. violaceum were the two most common causative fungi in females. Additionally, approximately 61.7% of black dot TCs occurred in females. For treatment, oral antifungal therapeutics were widely used in most patients with different treatment durations, although without a significant difference in efficacy (P = 0.106).
Conclusions
In the last decade, the prevalence of TC in children under 3 years old increased, and boys dramatically outnumbered girls. In adults, the TC prevalence in females is nine times that in males, and most TCs occurring in females are presented as black dots. Moreover, the zoophilic T. mentagrophytes complex has replaced T. violaceum and is now the second most prevalent organism, followed by M. canis of TC.

Similar content being viewed by others
Data Availability
All relevant data are cited in the manuscript.
Materials Availability
All relevant methods and materials used are cited in the manuscript.
Code Availability
Not applicable.
References
Ferguson L, Fuller LC. Spectrum and burden of dermatophytes in children. J Infect. 2017;74(Suppl 1):S54–60. Epub 2017/06/26. https://doi.org/10.1016/S0163-4453(17)30192-5.
Rodriguez-Cerdeira C, Martinez-Herrera E, Szepietowski JC, Pinto-Almazan R, Frias-De-Leon MG, Espinosa-Hernandez VM, et al. A systematic review of worldwide data on tinea capitis: analysis of the last 20 years. J Eur Acad Dermatol Venereol. 2021;35(4):844–83. Epub 2020/09/26. https://doi.org/10.1111/jdv.16951.
Grigoryan KV, Tollefson MM, Olson MA, Newman CC. Pediatric tinea capitis caused by Trichophyton violaceum and Trichophyton soudanense in Rochester, Minnesota. United States Int J Dermatol. 2019;58(8):912–5. Epub 2018/12/15. https://doi.org/10.1111/ijd.14352.
Zhan P, Li D, Wang C, Sun J, Geng C, Xiong Z, et al. Epidemiological changes in tinea capitis over the sixty years of economic growth in China. Med Mycol. 2015;53(7):691–8. Epub 2015/08/12. https://doi.org/10.1093/mmy/myv057.
Cai WY, Lu CM, Hu YX, Lu S, Xi LY. Clinical and mycological analysis of 241 cases of tinea capitis in Guangzhou region. Chin J Dermatol. 2011;44(8):585–6.
Getso MI, Hashemi SJ, Ghazvini RD, Yusuf SM, Khodavaisy S, Gerami-Shoar M, Kibiya FS, Aliyu UT, Sarvestani HK, Aliyu M. Determination of dermatophytes isolated from tinea capitis using conventional and ITS-based sequencing methods in Kano, Nigeria. J Mycol Med. 2021;31(3):101157. Epub 2021 May 26. https://doi.org/10.1016/j.mycmed.2021.101157.
Leung AKC, Hon KL, Leong KF, Barankin B, Lam JM. Tinea capitis: an updated review. Recent Pat Inflamm Allergy Drug Discov. 2020;14(1):58–68. Epub 2020/01/08. https://doi.org/10.2174/1872213X14666200106145624.
Chen XQ, Zheng DY, Xiao YY, Dong BL, Cao CW, Ma L, et al. Aetiology of tinea capitis in China: a multicentre prospective study. Br J Dermatol. 2022;186(4):705–12. Epub 2021/11/07. https://doi.org/10.1111/bjd.20875.
Liang G, Zheng X, Song G, Zhang M, Liu J, Zang X, et al. Adult tinea capitis in China: A retrospective analysis from 2000 to 2019. Mycoses. 2020;63(8):876–88. Epub 2020/05/13. https://doi.org/10.1111/myc.13102.
Park SK, Park SW, Yun SK, Kim HU, Park J. Tinea capitis in adults: A 18-year retrospective, single-centre study in Korea. Mycoses. 2019;62(7):609–16. Epub 2019/04/14. https://doi.org/10.1111/myc.12916.
Marcoux D, Dang J, Auguste H, McCuaig C, Powell J, Hatami A, et al. Emergence of African species of dermatophytes in tinea capitis: A 17-year experience in a Montreal pediatric hospital. Pediatr Dermatol. 2018;35(3):323–8. Epub 2018/03/25. https://doi.org/10.1111/pde.13446.
Aharaz A, Jemec GBE, Hay RJ, Saunte DML. Tinea capitis asymptomatic carriers: what is the evidence behind treatment? J Eur Acad Dermatol Venereol. 2021;35(11):2199–207. Epub 2021/06/20. https://doi.org/10.1111/jdv.17462.
Chen X, Jiang X, Yang M, Gonzalez U, Lin X, Hua X, et al. Systemic antifungal therapy for tinea capitis in children. Cochrane Database Syst Rev. 2016. Epub 2016/05/14. https://doi.org/10.1002/14651858.CD004685.pub3.
Le TK, Cohen BA. Tinea capitis: advances and a needed paradigm shift. Curr Opin Pediatr. 2021;33(4):387–91. Epub 2021/07/07. https://doi.org/10.1097/MOP.0000000000001034.
Funding
This work was funded by National Natural Science Foundation of China (NSFC, Grant Number: 82172289).
Author information
Authors and Affiliations
Contributions
SL and JZ contributed to the study conception and design. Material preparation, data collection and analysis were performed by WC, JH, JL, LL, LX, JZ, XL, ZZ, YT, HL, SL and JZ. The first draft of the manuscript was written by WC and JH, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interests
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical Approval
The study has been proved by the institution's ethics committee (Approval No. SYSEC-KY- KS-2019–098).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
The participants have consented to the submission of the original article to the journal.
Additional information
Handling Editor: Ruoyu Li.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cai, W., Huang, J., Li, J. et al. Epidemiology and Clinical Findings of Tinea Capitis: A 23-Year Retrospective, Single-Center Study in Guangzhou, China. Mycopathologia 188, 507–514 (2023). https://doi.org/10.1007/s11046-023-00730-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-023-00730-4