Abstract
Background
The increasing cases of bloodstream infections among children at neonatal intensive care units (NICUs) led this work to investigate biofilm production, antibiotics and the presence of ESβL genes in Serratia marcescens (S. marcescens) strains isolated from blood.
Methods
Twenty S. marcescens strains were isolated and identified by the VITEK-2 system over 7 months from late 2022 to mid-2023 from Ibn Al-Balady Hospital in Baghdad. Kirby-Bauer test was used to measure antibiotic susceptibility.
Results
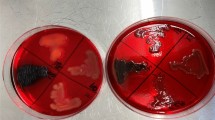
The results revealed that 95% of twenty S. marcescens isolates were non-susceptible to Ampicillin and Amoxicillin-clavulanic. Furthermore, S. marcescens isolates showed a high sensitivity rate 70% toward Imipenem. All S. marcescens strains 100% were produced biofilm. This work clarifies that, out of 20 S. marcescens strains, 80% were harbored ESβL genes. The coexistence of blaTEM, blaCTX and blaSHV genes was shown in 43.75% of strains, while 56.25% of S. marcescens strains harbored single ES\(\upbeta\)L genes. The biofilm values increase with the accuracy of EsβL genes. Phylogenetic analyses based on the sequence of blaCTX-M and blaTEM were done with closely related genes in the GenBank using MEGA6 software.
Conclusions
The distribution of blaTEM, blaCTX and blaSHV genes among local S. marcescens strains may be attributed to the indiscriminate use of antibiotics. The results confirmed the spread of ESβL genes in S. marcescens from blood infections among newborn infants.

Similar content being viewed by others
Data availability
No data is associated with the manuscript.
References
Coggins SA, Edwards EM, Flannery DD, Gerber JS, Horbar JD, Puopolo KM (2023) Serratia infection epidemiology among very preterm infants in the neonatal intensive care unit. Pediatr Infect Dis J 42(2):152–158. https://doi.org/10.1097/INF.0000000000003736
Weakland DR, Smith SN, Bell B, Tripathi A, Mobley HLT (2020) The Serratia marcescens Siderophore Serratiochelin is necessary for full virulence during bloodstream infection. Infect Immun 88(8):e00117-e120. https://doi.org/10.1128/IAI.00117-20
Bdulwahhab AM, Khalaf KJ (2022) Effect of cultivation conditions on hemolysin production from clinical isolates of Serratia marcescens. Al-Mustansiriyah J Sci 33:6–14. https://doi.org/10.23851/mjs.v33i1.1080
Greco-Stewart VS, Brown EE, Parr C, Kalab M, Jacobs MR, Yomtovian RA, Ramírez-Arcos SM (2012) Serratia marcescens strains implicated in adverse transfusion reactions form biofilms in platelet concentrates and demonstrate reduced detection by automated culture. Vox Sang 102(3):212–220. https://doi.org/10.1111/j.1423-0410.2011.01550.x
Phadke VK, Jacob JT (2016) Marvelous but morbid: infective endocarditis due to Serratia marcescens. Infect Dis Clin Pract 24(3):143–150. https://doi.org/10.1097/IPC.0000000000000360
Slain D, Howard C, Cooper G (2022) An antimicrobial treatment assessment of Serratia marcescens bacteremia and endocarditis. Front Antibiot 1:942721–942725. https://doi.org/10.3389/frabi.2022.942721
Tavares-Carreon F, De Anda-Mora K, Rojas-Barrera IC, Andrade A (2023) Serratia marcescens antibiotic resistance mechanisms of an opportunistic pathogen: a literature review. PeerJ 11:e14399. https://doi.org/10.7717/peerj.14399
Bradford PA (2001) Extended-spectrum beta-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev 14(4):933–951. https://doi.org/10.1128/CMR.14.4.933-951.2001
Smail SB, Al-Otrachi KI (2020) Phenotypic characterization of extended-spectrum beta-lactamases and metallo-beta-lactamase of multi drug resistant Acinetobacter baumannii causing nosocomial infections in Erbil city. Al-Mustansiriyah J Sci 30:51–56. https://doi.org/10.23851/mjs.v30i4.671
Sadeghi M, Sedigh ESH, Mojtahedi A (2021) Prevalence of ESBL and AmpC genes in E. coli isolates from urinary tract infections in the north of Iran. New Microbes New Infect 45:100947. https://doi.org/10.1016/j.nmni.2021.100947
Ray C, Anukul TS, Carlos JO, Norberto G (2017) Killing of Serratia marcescens biofilms with chloramphenicol. Ann Clin Microbiol Antimicrob 16:19. https://doi.org/10.1186/s12941-017-0192-2
Abdu-Allah SN, Hussein NH, Taha BM (2017) Study of bio film formation by Sphingomonas Paucimobilis isolates and in-vitro inhibition of bio film by Iraqi probiotics. J Global Pharm Technol 12(9):241–247
WHO (World Health Organization) (2003) Basic laboratory procedures in clinical bacteriology, 2nd edn. WHO, Geneva, pp 103–121
CLSI (Clinical and Laboratory Standards Institute) (2011) Performance standard for antimicrobial susceptibility testing; Twenty-first informational supplement, M100–S21. Clinical and Laboratory Standards Institute, Berwyn
Musafer HK, Kuchma SL, Naimie AA, Schwartzman JD, Al-Mathkhury HJ, O’Toole GA (2014) Investigating the link between imipenem resistance and biofilm formation by Pseudomonas aeruginosa. Microb Ecol 68(1):111–120. https://doi.org/10.1007/s00248-013-0361-6
Musafer HK, Nabeeh JF, Ahmed M (2022) Association of biofilm inducer with blaVIM, blaIMP and blaNDM in Pseudomonas aeruginosa isolates. Arch Razi Inst 77(5):1723–1728. https://doi.org/10.22092/ARI.2022.358104.2153
Al-Kadmy MS, Musafer HK, Abd Ali MH, Sajid S (2015) Detection of 16S ribosomal RNA methylation in extended-spectrum β-lactamase-producing Klebsiella pneumoniae clinical isolates from Baghdad hospitals. Iraqi J Biotechnol 14:53–62
Sambrook J, Fritsch EF, Maniatis T (1989) Molecular cloning: a laboratory manual, 2nd edn. Cold Spring Harbor Laboratory Press, New York, p 68
Bhatta DR, Hosuru Subramanya S, Hamal D, Shrestha R, Gauchan E et al (2021) Bacterial contamination of neonatal intensive care units: how safe are the neonates? Antimicrob Resist Infect Control 10:26. https://doi.org/10.1186/s13756-021-00901-2
Denton M (2007) Enterobacteriaceae. Int J Antimicrob Agents 29(3):S9–S22. https://doi.org/10.1016/S0924-8579(07)72174-X
Hussein NH (2023) Molecular detection of blaTEM, blaCTX-M and blaSHV genes in ESβL harboring uropthogenic Escherichia coli (UPEC) isolated from UTIs in Baghdad/Iraq. Rev Res Med Microbiol. https://doi.org/10.1097/MRM.000000000000036320
Musafer H, Majid A, Sawsan K (2023) Epidemiology and genetic diversity of CTX-M gene in Klebsiella Pneumoniaein Baghdad city. J Med Chem Sci 6:1419–1425. https://doi.org/10.26655/JMCHEMSCI.2023.6.21
Talab MD, Mehrabi MR, Mirzaee M (2017) Detection of AmpC beta-lactamase genes in clinical isolates of Escherichia coli in Kermanshah city. New Cell Mol Biotechnol J 7:69–76
Ali MG, Almoneim ZA, Kareem SM (2023) Evaluated gene expressions of Metallo beta lactamase genes GIM and VIM, SPM in Pseudomonas aeruginosa clinical isolates. Mol Biol Rep 50:10111–10120. https://doi.org/10.1007/s11033-023-08883-7
Khdair SR (2017) Detection of blaCTX-M gene among Pseudomonas aeruginosa isolated from water samples in Baghdad. Al-Mustansiriyah J Sci 28:35–40. https://doi.org/10.23851/mjs.v28i1.309
Shipitsyna IV, Osipova EV (2017) The biofilm formation ability of strains serratia spp., separated from wounds of patients with chronic osteomyelitis in mono-cultures and in composition of association of microorganisms harvested in vitro. Klin Lab Diagn 62(3):188–192
Mostatabi N, Farshad S, Ranjbar R (2013) Molecular evaluations of extended spectrum β-lactamase producing strains of Serratia isolated from blood samples of the patients in Namazi Hospital, Shiraz, Southern Iran. Iran J Microbiol 5(4):328–333
Legese MH, Asrat D, Aseffa A, Hasan B, Mihret A, Swedberg G (2022) Molecular epidemiology of extended-spectrum beta-lactamase and AmpC producing enterobacteriaceae among Sepsis patients in Ethiopia: a prospective multicenter study. Antibiotics 11:131. https://doi.org/10.3390/antibiotics11020131
Acknowledgements
This work was sponsored by the Biology department/ College of science/ Mustansiriyah University (www.Mustansiriyah.com).
Funding
There is No funding received.
Author information
Authors and Affiliations
Contributions
H.K.M. Proposal writing, revising, reading, approving, and submitting the final manuscript. N.H.H: study design, acquisition of data, proposal writing, and drafting of the manuscript. S.M.K.: study design, aquation and analysis of data, proposal writing, and drafting the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declared that there are no competing financial interests that could appear to influence the study reported in the manuscript.
Ethical approval
Clinical samples were taken with the approval and recommendation of the Iraqi Ministry of Health Research Ethics Commission. The ethical committee approval number for this study is CSEC/1020/0088.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Musafer, H.K., Hussein, N.H. & Kareem, S.M. Neonatal intensive care units: extended spectrum β-lactamase genes and biofilm formation by Serratia marcescens. Mol Biol Rep 51, 167 (2024). https://doi.org/10.1007/s11033-023-09124-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-023-09124-7