Abstract
Introduction
Though interest is growing for trials comparing planned delivery mode (vaginal delivery [VD]; cesarean section [CS]) in low-risk nulliparous women, appropriate study design is unclear. Our objective was to assess feasibility of three designs (preference trial [PCT], randomized controlled trial [RCT], partially randomized patient preference trial [PRPPT]) for a trial comparing planned delivery mode in low-risk women.
Methods
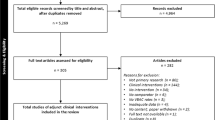
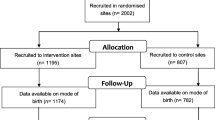
A cross-sectional survey of low-risk, nulliparous pregnant women (N = 416) and healthcare providers (N = 168) providing prenatal care and/or labor/delivery services was conducted in Argentina (2 public, 2 private hospitals). Proportion of pregnant women and providers willing to participate in each design and reasons for not participating were determined.
Results
Few women (< 15%) or professionals (33.3%) would participate in an RCT, though more would participate in PCTs (88% women; 65.9% professionals) or PRPPTs (44.4% public, 63.4% private sector women; 44.0% professionals). However, most women would choose vaginal delivery in the PCT and PRPPT (> 85%). Believing randomization unacceptable (RCT, PRPPT) and desiring choice of delivery mode (RCT) were women’s reasons for not participating. For providers, commonly cited reasons for not participating included unacceptability of performing CS without medical indication, difficulty obtaining informed consent, discomfort enrolling patients (all designs), and violating women’s right to choose (RCT).
Conclusions for Practice
Important limitations were found for each trial design evaluated. The necessity of stronger evidence regarding delivery mode in low-risk women suggests consideration of additional designs, such as a rigorously designed cohort study or an RCT within an obstetric population with equivocal CS indications.

Similar content being viewed by others
References
Alsayegh, E., Bos, H., Campbell, K., & Barrett, J. (2018). No. 361-caesarean delivery on maternal request. Journal of Obstetrics and Gynaecology Canada, 40(7), 967–971.
Aref-Adib, M., Vlachodimitropoulou, E., Khasriya, R., Lamb, B. W., & Selo-Ojeme, D. (2018). UK O&G trainees’ attitudes to caesarean delivery for maternal request. Journal of Obstetrics and Gynaecology, 38(3), 367–371.
Barrett, J. F., Hannah, M. E., Hutton, E. K., Willan, A. R., Allen, A. C., Armson, B. A.,… Ohlsson, A. (2013). A randomized trial of planned cesarean or vaginal delivery for twin pregnancy. New England Journal of Medicine, 369(14), 1295–1305.
Belizán, J. M., Minckas, N., McClure, E. M., Saleem, S., Moore, J. L., Goudar, S. S., et al. (2018). An approach to identify a minimum and rational proportion of caesarean sections in resource-poor settings: A global network study. Lancet Global Health, 6(8), e894–e901.
Betran, A. P., Torloni, M. R., Zhang, J., Ye, J., Mikolajczyk, R., Deneux-Tharaux, C., Oladapo, O. T., et al. (2015). What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reproductive Health, 12(1), 57.
Betrán, A. P., Ye, J., Moller, A. B., Zhang, J., Gulmezoglu, A. M., & Torloni, M. R. (2016). The increasing trend in caesarean section rates: Global, regional and national estimates: 1990–2014. PLoS ONE, 11(2), e0148343.
Brennan, D. J., Robson, M. S., Murphy, M., & O’Herlihy, C. (2009). Comparative analysis of international cesarean delivery rates using 10-group classification identifies significant variation in spontaneous labor. American Journal of Obstetrics and Gynecology, 201(3), 308.e1-308.e8.
Brewin, C. R., & Bradley, C. (1989). Patient preferences and randomised clinical trials. British Medical Journal (Clinical Research Edition), 299(6694), 313–315.
Cooper, K. G., Grant, A. M., & Garratt, A. M. (1997). The impact of using a partially randomised patient preference design when evaluating alternative managements for heavy menstrual bleeding. British Journal of Obstetrics and Gynaecology, 104(12), 1367–1373.
Crowther, C. A., Dodd, J. M., Hiller, J. E., Haslam, R. R., Robinson, J. S., & Birth After Caesarean Study Group. (2012). Planned vaginal birth or elective repeat caesarean: Patient preference restricted cohort with nested randomised trial. PLoS Medicine, 9(3), e1001192.
Dodd, J., Pearce, E., & Crowther, C. (2004). Women’s experiences and preferences following caesarean birth. Australian & New Zealand Journal of Obstetrics & Gynaecology, 44(6), 521–524.
Ecker, J. (2013). Elective cesarean delivery on maternal request. Journal of the American Medical Association, 309(18), 1930–1936.
FIGO Committee for the Study of Ethical Aspects of Human Reproduction and Women’s Health. (2012). Ethical issues in obstetrics and gynecology. International Federation of Gynecology and Obstetrics (FIGO). Retrieved January 15, 2019, from http://www.figo.org/about/guidelines.
Fowler, F. J., Jr. (2008). Survey research methods. Thousand Oaks, CA: Sage.
Grant, A., & Glazener, C. M. (2001). Elective caesarean section versus expectant management for delivery of the small baby. The Cochrane Database of Systematic Reviews, 2, CD000078.
Hannah, M. E., & Hannah, W. J. (1996). Feasibility of a randomized controlled trial of planned cesarean section versus planned vaginal delivery for breech presentation at term. American Journal of Obstetrics and Gynecology, 174(4), 1393–1394.
Hannah, M. E., Hannah, W. J., Hewson, S. A., Hodnett, E. D., Saigal, S., & Willan, A. R. (2000). Planned caesarean section versus planned vaginal birth for breech presentation at term: A randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet, 356(9239), 1375–1383.
Hyde, M. J., & Modi, N. (2012). The long-term effects of birth by caesarean section: The case for a randomised controlled trial. Early Human Development, 88(12), 943–949.
Kowalski, C. J., & Mrdjenovich, A. J. (2013). Patient preference clinical trials: Why and when they will sometimes be preferred. Perspectives in Biology and Medicine, 56(1), 18–35.
Lambert, M. F., & Wood, J. (2000). Incorporating patient preferences into randomized trials. Journal of Clinical Epidemiology, 53(2), 163–166.
Lavender, T., Hofmeyr, G. J., Neilson, J. P., Kingdon, C., & Gyte, G. M. (2012). Caesarean section for non-medical reasons at term. The Cochrane Database of Systematic Reviews, 3, CD004660.
Lavender, T., & Kingdon, C. (2009). Primigravid women’s views of being approached to participate in a hypothetical term cephalic trial of planned vaginal birth versus planned cesarean birth. Birth, 36(3), 213–219.
Lavender, T., Kingdon, C., Hart, A., Gyte, G., Gabbay, M., & Neilson, J. P. (2005). Could a randomised trial answer the controversy relating to elective caesarean section? National survey of consultant obstetricians and heads of midwifery. British Medical Journal, 331(7515), 490.
Liu, N. H., Mazzoni, A., Zamberlin, N., Colomar, M., Chang, O. H., Arnaud, L., et al. (2013). Preferences for mode of delivery in nulliparous Argentinean women: A qualitative study. Reproductive Health, 10(1), 2. https://doi.org/10.1186/1742-4755-10-2.
Lumley, J., Lester, A., Renou, P., & Wood, C. (1985). A failed RCT to determine the best method of delivery for very low birth weight infants. Controlled Clinical Trials, 6(2), 120–127.
Mazzoni, A., Althabe, F., Gutierrez, L., Gibbons, L., Liu, N. H., Bonotti, A. M., et al. (2016). Women’s preferences and mode of delivery in public and private hospitals: A prospective cohort study. BMC Pregnancy and Childbirth, 16(1), 34. https://doi.org/10.1186/s12884-016-0824-0.
McLeod, L., Barrett, J., Hewson, S., & Hannah, M. E. (2004). Women’s views regarding participation in a proposed randomized controlled trial of twin delivery. Journal of Obstetrics and Gynaecology Canada, 26(6), 575–579.
Murray-Davis, B., McVittie, J., Barrett, J. F., Hutton, E. K., & Twin Birth Study Collaborative Group. (2016). Exploring women’s preferences for the mode of delivery in twin gestations: Results of the Twin Birth Study. Birth, 43(4), 285–292.
National Institute for Health and Clinical Excellence. (2011). NICE CG132 Caesarean Section. Retrieved from http://guidance.nice.org.uk/CG132.
National Program of Statistics in Health. (2011). 2010 Vital Statistics. http://www.deis.msal.gov.ar/wp-content/uploads/2015/12/Serie5Nro54.pdf.
Paleari, L., Gibbons, L., Chacón, S., Ramil, V., & Belizán, J. M. (2012). Rates of caesarean sections in two types of private hospitals: Restricted-access and open-access [Tasa de cesáreas en dos hospitales privados con normativas diferentes: abierto y cerrado]. Ginecología y Obstetricia De México, 80(4), 263–269.
Penn, Z. J., Steer, P. J., & Grant, A. (2014). A multicentre randomised controlled trial comparing elective and selective caesarean section for the delivery of the preterm breech infant. British Journal of Obstetrics and Gynaecology, 121(Suppl 7), 48–53.
Rivo, J. C., Amyx, M., Pingray, V., Casale, R. A., Fiorillo, A. E., Krupitzki, H. B., et al. (2018). Obstetrical providers’ preferred mode of delivery and attitude towards non-medically indicated caesarean sections: A cross-sectional study. British Journal of Obstetrics and Gynaecology, 125(10), 1294–1302.
Turner, C. E., Young, J. M., Solomon, M. J., Ludlow, J., Benness, C., & Phipps, H. (2008). Willingness of pregnant women and clinicians to participate in a hypothetical randomised controlled trial comparing vaginal delivery and elective caesarean section. Australian & New Zealand Journal of Obstetrics & Gynaecology, 48(6), 542–546.
Wallace, R. L., Schifrin, B. S., & Paul, R. H. (1984). The delivery route for very-low-birth-weight infants. A preliminary report of a randomized, prospective study. Journal of Reproductive Medicine, 29(10), 736–740.
Acknowledgements
We are grateful to the women and healthcare professionals who participated in this study. We thank Dr. Agustina Mazzoni (IECS) for sharing survey instruments and other materials used in her study, the “Women’s preferences and mode of delivery in public and private hospitals: a prospective cohort study.” Dr. Amyx thanks her dissertation committee members for their guidance (Xu Xiong, MD, DrPH [chair], Gretchen Clum, PhD, and Pierre Buekens, MD, PhD [Tulane University]). We could not have done this study without the collaboration and dedication of the Feasibility of ‘Mode of Delivery Trial’ Study Group. This study was funded by the National Institutes of Health Training in Global Reproductive Epidemiology grant (5T32HD057780); National Institutes of Health Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Heart, Blood, and Lung Institute, and the National Institutes of Health Office of Research for Women’s Health through the Fogarty Global Health Fellows Program Consortium comprised of the University of North Carolina, John Hopkins, Morehouse and Tulane (R25TW009340); Health Resources & Services Administration/Maternal & Child Health Bureau Maternal and Child Health Epidemiology Doctoral Training Program (#T03MC07649).
Collaborators for the Feasibility of ‘Mode of Delivery Trial’ Study Group
Study coordinating group: Dr. Melissa Amyx (PI); Dr. José M. Belizán (Co-Investigator); Julie Rivo (Sub-Investigator); Dr. Fernando Althabe, Verónica Pingray, Gabriela Cormick, Nicole Minckas Qualitative/pilot phase coordination group: María Belizán, Ana Becu. Data management/coordination: Dr. Mabel Berrueta (coordination); Luz Gibbons (survey development and data analysis); Alvaro Ciganda (technical support); Candela Stella, Paula Rubinstein (data management). Participating hospitals and staff: Centro de Educación Médica e Investigaciones Clínicas “Norberto Quirno” (CEMIC), Autonomous City of Buenos Aires, Argentina: Dr. Angél E. Fiorillo (Hospital-based PI); Dr. Hugo B. Krupitzki, Dr. Javier A. Schvartzman (Hospital-based Co-investigators); Dr. Karen Tapper (Coordinator qualitative phase); Nora Viergue, Mariana Piola Sanatorio de la Mujer, Rosario, Santa Fe, Argentina: Dr. Julio D. Malamud (Hospital-based PI); Dr. Mauricio Belizán (Co-Investigator); Alicia Beatriz del Pino (Co-Investigator, Coordinator); Pablo Quaranta; Julieta Malamud; Marianela Oriti; Gonzalo Molina; Patricia Ahumada; Leandro Biancofiore. Instituto de la Maternidad y Ginecología Nuestra Señora de las Mercedes, San Miguel de Tucumán, Tucumán, Argentina: Dr. Gerardo Murga Tartalo (Hospital-based PI); Dr. María Lucía Medina, Dr. María Mendilaharzu (Co-investigators, Coordinators); Dr. Elena Hurtado, Susana Gil, Dr. Lucía Inés Barcatt Mirande, Dr. Laissa Antonella Avellaneda, Dr. María Eugenia Moyano, Dr. Evelyn Geanette Llano P., Dr. Carla Díaz Martín, Dr. Viviana Goldina Jaitt, Dr. M. Valentina Giraldez, Dr. Melina Julian, Dr. Antonella Gisel Quintana, Dr. Lourdes Alicia Bravo, Dr. Gabriela Alejandra Olavarría Mendez, Dr. Diego Martín Rongetti, Dr. Lourdes Solange Venegas Tarancón, Dr. Luciana Andrea Carrizo, Dr. Federico Coria, Dr. Analía Soledad Carrizo. Hospital Nacional A. Posadas, El Palomar, Buenos Aires, Argentina: Dr. Roberto A. Casale (Hospital-based PI); Silvana Varela, Mónica Trasmonte (Hospital-based Co-investigator, Coordinator); Dr. Lucio Ribola (Coordinator), Analia Mereles, Gabriela Violano, Milena Losardo, Vanina Lauphan, Yesica Lombardo.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical Approval
The study research protocol was approved by the appropriate ethics committees, including the Institutional Review Boards of Tulane University and Duke University and by local hospital ethics committees (CEMIC; Posadas Hospital). The study was conducted in accordance with the ethical standards of the Declaration of Helsinki.
Informed Consent
All participants gave written informed consent prior to participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members for the Feasibility of “Mode of Delivery Trial” Study Group are listed in “Acknowledgements”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Amyx, M.M., Althabe, F., Rivo, J. et al. Feasibility of Conducting a Trial Assessing Benefits and Risks of Planned Caesarean Section Versus Planned Vaginal Birth: A Cross-Sectional Study. Matern Child Health J 25, 136–150 (2021). https://doi.org/10.1007/s10995-020-03073-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-020-03073-4