Abstract
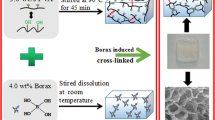
Gelatin has many superior biological properties and can absorb a large volume of water to form hydrogels, making it a promising material for skin wound care. In this study, gel membranes were prepared based on gelatin and added with different amounts of the synthesized carboxymethyl chitosan (CMCS) and poly(N-isopropylacrylamide-co-acrylic acid) (P(NI-co-AA)) copolymer for providing antibacterial and thermo-responsive properties, respectively. The synthesized CMCS had a degree of carboxymethyl substitution at 0.77 and the P(NI-co-AA) had an AA content of 5.7 mol %. Both CMCS and P(NI-co-AA) had carboxylate groups that could further provide ionic-crosslinking sites for the membranes. Though the P(NI-co-AA) copolymer had a higher phase transition temperature than poly(N-isopropylacrylamide) (PNIPAAm) owing to its hydrophilic carboxylate groups, the prepared gelatin/CMCS/P(NI-co-AA) membranes had similar phase transition temperatures to the PNIPAAm at around 30.5 − 32.4 °C because of ionic crosslinking. Moreover, the equilibrium swelling ratio and water vapor transmission rate of the gel membranes were in the range of 769 − 1226% and 1678 − 2496 g/m2- day, respectively. These membranes could promote cell proliferation of human keratinocytes (HaCaT) and mouse fibroblasts (L-929), indicating they were non-toxic to the cells. They also had antimicrobial properties against S. aureus and E. coli, where the antibacterial efficacy increased with increasing the CMCS content. These hydrogel membranes had good biocompatibility, suitable swelling ratio and water vapor transmission rate, antibacterial and thermo-responsive properties. Therefore, they have potential to be applied as functional wound dressing material.







Similar content being viewed by others
References
Rahman MM, Pervez S, Nesa B, Khan MA (2013) Preparation and characterization of porous scaffold composite films by blending chitosan and gelatin solutions for skin tissue engineering. Polym Int 62:79–86
Chen K, Wang F, Liu S, Wu X, Xu L, Zhang D (2020) In situ reduction of silver nanoparticles by sodium alginate to obtain silver-loaded composite wound dressing with enhanced mechanical and antimicrobial property. Int J Biol Macromol 148:501–509
Park SN, Kim JK, Suh H (2004) Evaluation of antibiotic-loaded collagen-hyaluronic acid matrix as a skin substitute. Biomaterials 25:3689–3698
Ward AG, Courts A (1977) The science and technology of gelatin. Academic press, New York
Ponticiello MS, Schinagl RM, Kadiyala S, Barry FP (2000) Gelatin-based resorbable sponge as a carrier matrix for human mesenchymal stem cells in cartilage regeneration therapy. J Biomed Mater 52:246–255
Djagny KB, Wang Z, Xu S (2010) Gelatin: a valuable protein for food and pharmaceutical industries.vReview. Crit Rev Food Sci Nutr 41:481–492
Postlethwaite AE, Seyer JM, Kang AH (1978) Chemotactic attraction of human fibroblasts to type I, II, and III collagens and collagen-derived peptides. Proc Natl Acad Sci 75:871–875
Pankongadisak P, Ruktanonchai UR, Supaphol P, Suwantong O (2015) Development of silver nanoparticles-loaded calcium alginate beads embedded in gelatin scaffolds for use as wound dressings. Polym Int 64:275–283
Muzzarelli RA, El Mehtedi M, Bottegoni C, Gigante A (2016) Physical properties imparted by genipin to chitosan for tissue regeneration with human stem cells: A review. Int J Biol Macromol 93:1366–1381
Deepthi S, Venkatesan J, Kim S-K, Bumgardner JD, Jayakumar R (2016) An overview of chitin or chitosan/nano ceramic composite scaffolds for bone tissue engineering. Int J Biol Macromol 93:1338–1353
Anitha A, Sowmya S, Kumar PS, Deepthi S, Chennazhi K, Ehrlich H et al (2014) Chitin and chitosan in selected biomedical applications. Prog Polym Sci 39:1644–1667
Wu SJ, Don TM, Lin CW, Mi FL (2014) Delivery of berberine using chitosan/fucoidan-taurine conjugate nanoparticles for treatment of defective intestinal epithelial tight junction barrier. Mar Drugs 12:5677–5697
Jayakumar R, Prabaharan M, Nair S, Tokura S, Tamura H, Selvamurugan N (2010) Novel carboxymethyl derivatives of chitin and chitosan materials and their biomedical applications. Prog in Mater Sci 5:675–709
Shariatinia Z (2018) Carboxymethyl chitosan: Properties and biomedical applications. Int J Biol Macromol 120:1406–1419
Zhang C, Yang X, Hu W, Han X, Fan L, Tao S (2020) Preparation and characterization of carboxymethyl chitosan/collagen peptide/oxidized konjac composite hydrogel. Int J Biol Macromol 149:31–40
Huang X, Zhang Y, Zhang X, Xu L, Chen X, Wei S et al (2013) Influence of radiation crosslinked carboxymethyl-chitosan/gelatin hydrogel on cutaneous wound healing. Mater Sci Eng 33:4816–4824
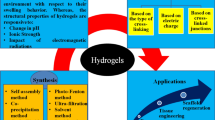
Ratner BD, Hoffman AS (1976) Synthetic hydrogels for biomedical applications, hydrogels for medical and related applications, in ACS Symposium Series, Vol 31, Chapter 1, ACS Publications, 1–36
Lee KY, Mooney DJ (2001) Hydrogels for tissue engeneering. Chem Rev 101:1869–1880
Qiu Y, Park K (2001) Environment-sensitive hydrogels for drug delivery. Adv Drug Deliv Rev 53:321–339
Kamoun EA, Kenawy ES, Chen X (2017) A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J Adv Res 8:217–233
Zha L, Banik B, Alexis F (2011) Stimulus responsive nanogels for drug delivery. Soft Matter 7:5908–5916
Che Y, Li D, Liu Y, Yue Z, Zhao J, Ma Q et al (2018) Design and fabrication of a triple-responsive chitosan-based hydrogel with excellent mechanical properties for controlled drug delivery. J Polym Res 25:169
Don TM, Lu KY, Lin LJ, Hsu CH, Wu JY, Mi FL (2017) Temperature/pH/Enzyme triple-responsive cationic protein/PAA-b-PNIPAAm nanogels for controlled anticancer drug and photosensitizer delivery against multidrug resistant breast cancer cells. Mol Pharm 14:4648–4660
Chee C, Rimmer S, Soutar I, Swanson L (2001) Fluorescence investigations of the thermally induced conformational transition of poly (N-isopropylacrylamide). Polymer 42:5079–5087
Li H, Williams GR, Wu J, Wang H, Sun X, Zhu LM et al (2017) Poly(N-isopropylacrylamide)/poly(l-lactic acid-co-ɛ-caprolactone) fibers loaded with ciprofloxacin as wound dressing materials. Mater Sci Eng 79:245–254
Zubik K, Singhsa P, Wang Y, Manuspiya H, Narain R (2017) Thermo-responsive poly(N-isopropylacrylamide)-cellulose nanocrystals hybrid hydrogels for wound dressing. Polymers 9:119
Jiang B, Larson JC, Drapala PW, Pérez-Luna VH, Kang-Mieler JJ, Brey EM (2012) Investigation of lysine acrylate containing poly (N-isopropylacrylamide) hydrogels as wound dressings in normal and infected wounds. J Biomed Mater Res B Appl Biomater 100:668–676
Reddy TT, Kano A, Maruyama A, Hadano M, Takahara A (2009) Synthesis and characterization of semi-interpenetrating polymer networks based on polyurethane and N-isopropylacrylamide for wound dressing. J Biomed Mater Res B Appl Biomater 88:32–40
Reddy TT, Kano A, Maruyama A, Hadano M, Takahara A (2008) Thermosensitive transparent semi-interpenetrating polymer networks for wound dressing and cell adhesion control. Biomacromol 9:1313–1321
Lin SY, Chen KS, Liang RC (2001) Design and evaluation of drug-loaded wound dressing having thermoresponsive, adhesive, absorptive and easy peeling properties. Biomaterials 22:2999–3004
Kuo CY, Don TM, Hsu SC, Lee CF, Chiu WY, Huang CY (2016) Thermo- and pH-induced self-assembly of P (AA-b-NIPAAm-b-AA) triblock copolymers synthesized via RAFT polymerization. J Polym Sci Polym Chem 54:1109–1118
Park JS, Yang HN, Woo DG, Jeon SY, Park KH (2013) Poly(N-isopropylacrylamide-co-acrylic acid) nanogels for tracing and delivering genes to human mesenchymal stem cells. Biomaterials 34:8819–8834
Gao Y, Ahiabu A, Serpe MJ (2014) Controlled drug release from the aggregation–disaggregation behavior of pH-responsive microgels. ACS Appl Mater Interfaces 6:13749–13756
Lin YJ, Lee GH, Chou CW, Chen YP, Wu TH, Lin HR (2015) Stimulation of wound healing by PU/hydrogel composites containing fibroblast growth factor-2. J Mater Chem 3:1931–1941
Choudhary M, Chhabra P, Tyagi A, Singh H (2021) Scar free healing of full thickness diabetic wounds: A unique combination of silver nanoparticles as antimicrobial agent, calcium alginate nanoparticles as hemostatic agent, fresh blood as nutrient/growth factor supplier and chitosan as base matrix. Inter J Biol Macromol 178:41–52
Tao G, Cai R, Wang Y, Zuo H, He H (2021) Fabrication of antibacterial sericin based hydrogel as an injectable and mouldable wound dressing. Mater Sci Eng C 119:111597
Sadeghi D, Solouk A, Samadikuchaksaraei A, Seifalian AM (2021) Preparation of internally-crosslinked alginate microspheres: Optimization of process parameters and study of pH-responsive behaviors. Carbohydr Polym 255:117336
Masood R, Anam Khubaib M, Hussain T, Raza ZA (2021) Silver-containing polysaccharide-based tricomponent antibacterial fibres for wound care applications. J Wound Care 30(1):81–88
Nokhodchi A, Tailor A (2004) In situ cross-linking of sodium alginate with calcium and aluminum ions to sustain the release of theophylline from polymeric matrices. Il Farmaco 59:999–1004
Tarighi P, Khoroushi M (2014) A review on common chemical hemostatic agents in restorative dentistry. Dent Res J 11(4):423–428
Palm MD, Altman JS (2008) Topical hemostatic agents: a review. Dermatol Surg 34(4):431–445
Henley J, Brewer JD (2013) Newer hemostatic agents used in the practice of dermatologic surgery. Dermatol Res Pract 2013:279289
Shen YH, Dempsey BA (1998) Synthesis and speciation of polyaluminum chloride for water treatment. Environ Int 24(8):899–910
Nouri S, Sharif MR, Panahi Y, Ghanei M, Jamali B (2015) Efficacy and safety of aluminum chloride in controlling external hemorrhage: an animal model study. Iran Red Crescent Med J 17:e19714
Tai HY, Chou SH, Cheng LP, Yu HT, Don TM (2012) Asymmetric composite membranes from chitosan and tricalcium phosphate useful for guided bone regeneration. J Biomater Sci Polym Ed 23:1153–1170
Trombotto S, Ladavière C, Delolme F, Domard A (2008) Chemical preparation and structural characterization of a homogeneous series of chitin/chitosan oligomers. Biomacromol 9:1731–1738
Rinaudo M, Le Dung P, Gey C, Milas M (1992) Substituent distribution on O, N-carboxymethylchitosans by 1H and 13C NMR. Int J Biol Macromol 14:122–128
Philippova OE, Hourdet D, Audebert R, Khokhlov AR (1997) pH-responsive gels of hydrophobically modified poly (acrylic acid). Macromolecules 30:8278–8285
Nagahama H, Maeda H, Kashiki T, Jayakuma R, Furuike T, Tamura H (2009) Preparation and characterization of novel chitosan/gelatin membranes using chitosan hydrogel. Carbohydr Polym 76:255–260
Lamke LO, Nilsson GE, Reithner HL (1977) The evaporative water loss from burns and the water-vapour permeability of grafts and artificial membranes used in the treatment of burns. Burns 3:159
Kim I, Yoo M, Seo J, Park S, Na H, Lee H et al (2007) Evaluation of semi-interpenetrating polymer networks composed of chitosan and poloxamer for wound dressing application. Int J Pharm 341:35–43
Gupta VB, Anitha S, Hegde M, Zecca L, Garruto R, Ravid R et al (2005) Aluminium in Alzheimer’s disease: are we still at a crossroad? Cell Mol Life Sci 62:143–158
Goullé J-P, Grangeot-Keros L (2020) Aluminum and vaccines: current state of knowledge. Med Mal Infect 50:16–21
Sudarshan N, Hoover D, Knorr D (1992) Antibacterial action of chitosan. Food Biotechnol 6:257–272
Helander I, Nurmiaho-Lassila EL, Ahvenainen R, Rhoades J, Roller S (2001) Chitosan disrupts the barrier properties of the outer membrane of Gram-negative bacteria. Int J Food Microbiol 71:235–244
Acknowledgment
This research was supported by the Ministry of Science and Technology (MOST) in Taiwan, under grant number 108-2221-E-032-015.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huang, YC., Lee, CT. & Don, TM. Physicochemical characteristics of thermo-responsive gelatin membranes containing carboxymethyl chitosan and poly(N-isopropylacrylamide-co-acrylic acid). J Polym Res 28, 173 (2021). https://doi.org/10.1007/s10965-021-02534-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10965-021-02534-w