Abstract
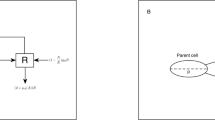
The use of β-lactam (BL) and β-lactamase inhibitor (BLI) combinations, such as piperacillin-tazobactam (PIP-TAZ) is an effective strategy to combat infections by extended-spectrum β-lactamase-producing bacteria. However, in Gram-negative bacteria, resistance (both mutational and adaptive) to BL-BLI combination can still develop through multiple mechanisms. These mechanisms may include increased β-lactamase activity, reduced drug influx, and increased drug efflux. Understanding the relative contribution of these mechanisms during resistance development helps identify the most impactful mechanism to target in designing a treatment to counter BL-BLI resistance. This study used semi-mechanistic mathematical modeling in combination with antibiotic sensitivity assays to assess the potential impact of different resistance mechanisms during the development of PIP-TAZ resistance in a Klebsiella pneumoniae isolate expressing CTX-M-15 and SHV-1 β-lactamases. The mathematical models were used to evaluate the potential impact of several cellular changes as a sole mediator of PIP-TAZ resistance. Our semi-mechanistic model identified 2 out of the 13 inspected mechanisms as key resistance mechanisms that may independently support the observed magnitude of PIP-TAZ resistance, namely porin loss and efflux pump up-regulation. Simulation using the resulting models also suggested the possible adjustment of PIP-TAZ dose outside its commonly used 8:1 dosing ratio. The current study demonstrated how theory-based mechanistic models informed by experimental data can be used to support hypothesis generation regarding potential resistance mechanisms, which may guide subsequent experimental studies.




Similar content being viewed by others
References
Oliphant CM, Eroschenko K (2015) Antibiotic resistance, Part 2: gram-negative pathogens. JNP-J Nurse Pract 11:79–86
Dhillon RH, Clark J (2012) ESBLs: a clear and present danger? Crit Care Res Pract 2012:625170
Drawz SM, Bonomo RA (2010) Three decades of beta-lactamase inhibitors. Clin Microbiol Rev 23(1):160–201. https://doi.org/10.1128/CMR.00037-09
Abodakpi H, Chang KT, Gao S, Sánchez-Díaz AM, Cantón R, Tam VH (2019) Optimal piperacillin-tazobactam dosing strategies against extended-Spectrum-β-Lactamase-producing Enterobacteriaceae. Antimicrob Agents Chemother 63(2):e01906–e01918. https://doi.org/10.1128/AAC.01906-18
Abdelraouf K, Chavda KD, Satlin MJ, Jenkins SG, Kreiswirth BN, Nicolau DP (2020) Piperacillin-tazobactam-resistant/third-generation cephalosporin-susceptible Escherichia coli and Klebsiella pneumoniae isolates: resistance mechanisms and in vitro-in vivo discordance. Int J Antimicrob Agents 55(3):105885
Zhou K, Tao Y, Han L, Ni Y, Sun J (2019) Piperacillin-Tazobactam (TZP) resistance in Escherichia coli due to hyperproduction of TEM-1 β-Lactamase mediated by the promoter Pa/Pb. Front Microbiol 10:833. https://doi.org/10.3389/fmicb.2019.00833
Nicolas-Chanoine MH, Mayer N, Guyot K, Dumont E, Pagès JM (2018) Interplay between membrane permeability and enzymatic barrier leads to antibiotic-dependent resistance in Klebsiella Pneumoniae. Front Microbiol 9:1422. https://doi.org/10.3389/fmicb.2018.01422
Fernández L, Hancock RE (2012) Adaptive and mutational resistance: role of porins and efflux pumps in drug resistance. Clin Microbiol Rev 25(4):661–681. https://doi.org/10.1128/CMR.00043-12
Pages JM, Lavigne JP, Leflon-Guibout V, Marcon E, Bert F, Noussair L, Nicolas-Chanoine MH (2009) Efflux pump, the masked side of beta-lactam resistance in Klebsiella pneumoniae clinical isolates. PLoS ONE 4(3):e4817. https://doi.org/10.1371/journal.pone.0004817
Kakoullis L, Papachristodoulou E, Chra P, Panos G (2021) Mechanisms of antibiotic resistance in important gram-positive and gram-negative pathogens and novel antibiotic solutions. Antibiot (Basel Switzerland) 10(4):415. https://doi.org/10.3390/antibiotics10040415
Heinz E, Ejaz H, Bartholdson Scott J, Wang N, Gujaran S, Pickard D, Wilksch J, Cao H, Haq IU, Dougan G, Strugnell RA (2019) Resistance mechanisms and population structure of highly drug resistant Klebsiella in Pakistan during the introduction of the carbapenemase NDM-1. Sci Rep 9(1):2392. https://doi.org/10.1038/s41598-019-38943-7
Masi M, Réfregiers M, Pos KM, Pagès JM (2017) Mechanisms of envelope permeability and antibiotic influx and efflux in gram-negative bacteria. Nat Microbiol 2:17001. https://doi.org/10.1038/nmicrobiol.2017.1
Prochnow H, Fetz V, Hotop SK, García-Rivera MA, Heumann A, Brönstrup M (2019) Subcellular quantification of uptake in gram-negative bacteria. Anal Chem 91(3):1863–1872. https://doi.org/10.1021/acs.analchem.8b03586
Mi K, Zhou K, Sun L, Hou Y, Ma W, Xu X, Huo M, Liu Z, Huang L (2022) Application of semi-mechanistic pharmacokinetic and pharmacodynamic model in antimicrobial resistance. Pharmaceutics 14(2):246. https://doi.org/10.3390/pharmaceutics14020246
Sahoo S, Mishra A, Kaur H, Hari K, Muralidharan S, Mandal S, Jolly MK (2021) A mechanistic model captures the emergence and implications of non-genetic heterogeneity and reversible drug resistance in ER + Breast cancer cells. NAR cancer 3(3):zcab027. https://doi.org/10.1093/narcan/zcab027
Liakopoulos A, Betts J, La Ragione R, van Essen-Zandbergen A, Ceccarelli D, Petinaki E, Koutinas CK, Mevius DJ (2018) Occurrence and characterization of extended-spectrum cephalosporin-resistant enterobacteriaceae in healthy household dogs in Greece. J. Med. Microbiol 67(7):931–935
Kojima S, Nikaido H (2013) Permeation rates of penicillins indicate that Escherichia coli porins function principally as nonspecific channels. PNAS 110(28):E2629–E2634
Lim SP, Nikaido H (2010) Kinetic parameters of efflux of penicillins by the multidrug efflux transporter AcrAB-TolC of Escherichia coli. Antimicrob Agents Chemother 54(5):1800–1806. https://doi.org/10.1128/AAC.01714-09
Faheem M, Rehman MT, Danishuddin M, Khan AU (2013) Biochemical characterization of CTX-M-15 from Enterobacter cloacae and designing a novel non-β-lactam-β-lactamase inhibitor. PLoS ONE 8(2):e56926. https://doi.org/10.1371/journal.pone.0056926
Helfand MS, Bethel CR, Hujer AM, Hujer KM, Anderson VE, Bonomo RA (2003) Understanding resistance to beta-lactams and beta-lactamase inhibitors in the SHV beta-lactamase: lessons from the mutagenesis of SER-130. J Biol Chem 278(52):52724–52729. https://doi.org/10.1074/jbc.M306059200
Maurizi MR (1992) Proteases and protein degradation in Escherichia coli. Experientia 48(2):178–201. https://doi.org/10.1007/BF01923511
Perilli M, Franceschini N, Bonfiglio G, Segatore B, Stefani S, Nicoletti G, Perez MM, Bianchi C, Zollo A, Amicosante G (2000) A kinetic study on the interaction between tazobactam (a penicillanic acid sulphone derivative) and active-site serine beta-lactamases. J Enzyme Inhib 15(1):1–10. https://doi.org/10.1080/14756369909030337
Nielsen EI, Friberg LE (2013) Pharmacokinetic-pharmacodynamic modeling of antibacterial drugs. Pharmacol Rev 65(3):1053–1090. https://doi.org/10.1124/pr.111.005769
Viane E, Chanteux H, Servais H, Mingeot-Leclercq M-P, Tulkens PM (2002) Comparative Stability Studies of antipseudomonal-lactams for potential administration through portable elastomeric pumps (home therapy for cystic fibrosis patients) and motor-operated syringes (intensive care units). Antimicrob Agents Chemoter 46(8):2327–2332. https://doi.org/10.1128/AAC.46.8.2327-2332.2002
Samara E, Moriarty TF, Decosterd LA, Richards RG, Gautier E, Wahl P (2017) Antibiotic stability over six weeks in aqueous solution at body temperature with and without heat treatment that mimics the curing of bone cement. Bone Jt Res 6(5):296–306. https://doi.org/10.1302/2046-3758.65.BJR-2017-0276.R1
Kaczmarek FM, Dib-Hajj F, Shang W, Gootz TD (2006) High-level carbapenem resistance in a Klebsiella pneumoniae clinical isolate is due to the combination of bla(ACT-1) beta-lactamase production, porin OmpK35/36 insertional inactivation, and down-regulation of the phosphate transport porin phoe. Antimicrob Agents Chemother 50(10):3396–3406. https://doi.org/10.1128/AAC.00285-06
Lee YJ, Huang CH, Ilsan NA, Lee IH, Huang TW (2021) Molecular epidemiology and characterization of carbapenem-resistant Klebsiella pneumoniae isolated from urine at a teaching hospital in Taiwan. Microorganisms 9(2):271. https://doi.org/10.3390/microorganisms9020271
Singh T, Singh PK, Das S, Wani S, Jawed A, Dar SA (2019) Transcriptome analysis of beta-lactamase genes in diarrheagenic Escherichia coli. Sci Rep 9(1):3626. https://doi.org/10.1038/s41598-019-40279-1
Jones AK, Ranjitkar S, Lopez S, Li C, Blais J, Reck F, Dean CR (2018) Impact of Inducible blaDHA-1 on susceptibility of Klebsiella pneumoniae clinical isolates to LYS228 and identification of chromosomal mpl and ampD mutations mediating Upregulation of plasmid-borne blaDHA-1 expression. Antimicrob Agents Chemother 62(10):e01202–e01218. https://doi.org/10.1128/AAC.01202-18
Wang X, Minasov G, Shoichet BK (2002) Evolution of an antibiotic resistance enzyme constrained by stability and activity trade-offs. J Mol Biol 320(1):85–95. https://doi.org/10.1016/S0022-2836(02)00400-X
Ramdani-Bouguessa N, Manageiro V, Jones-Dias D, Ferreira E, Tazir M, Caniça M (2011) Role of SHV β-lactamase variants in resistance of clinical Klebsiella pneumoniae strains to β-lactams in an Algerian hospital. J Med Microbiol 60(Pt 7):983–987. https://doi.org/10.1099/jmm.0.030577-0
Tsai YK, Fung CP, Lin JC, Chen JH, Chang FY, Chen TL, Siu LK (2011) Klebsiella pneumoniae outer membrane porins OmpK35 and OmpK36 play roles in both antimicrobial resistance and virulence. Antimicrob Agents Chemother 55(4):1485–1493. https://doi.org/10.1128/AAC.01275-10
Maurya N, Jangra M, Tambat R, Nandanwar H (2019) Alliance of efflux pumps with β-lactamases in multidrug-resistant Klebsiella pneumoniae isolates. Microb Drug Resist 25(8):1155–1163. https://doi.org/10.1089/mdr.2018.0414
Bergstrand M, Karlsson MO (2009) Handling data below the limit of quantification in mixed effect models. AAPS J 11(2):371–380. https://doi.org/10.1208/s12248-009-9112-5
Clegg LE, Mac Gabhann F (2015) Molecular mechanism matters: benefits of mechanistic computational models for drug development. Pharmacol Res 99:149–154. https://doi.org/10.1016/j.phrs.2015.06.002
Graeme-Cook KA (1991) The regulation of porin expression in Escherichia coli: effect of turgor stress. FEMS Microbiol Lett 63(2–3):219–223. https://doi.org/10.1016/0378-1097(91)90089-s
Zhu M, Dai X (2018) High salt cross-protects Escherichia coli from antibiotic treatment through increasing efflux pump expression. mSphere 3(2):e00095–e00018. https://doi.org/10.1128/mSphere.00095-18
Ferrand A, Vergalli J, Pagès JM, Davin-Regli A (2020) An intertwined network of regulation controls membrane permeability including drug influx and efflux in enterobacteriaceae. Microorganisms 8(6):833. https://doi.org/10.3390/microorganisms8060833
Wong F, Wilson S, Helbig R, Hegde S, Aftenieva O, Zheng H, Liu C, Pilizota T, Garner EC, Amir A, Renner LD (2021) Understanding beta-lactam-induced lysis at the single-cell level. Front Microbiol 12:712007. https://doi.org/10.3389/fmicb.2021.712007
Khalifa SM, El-Aziz A, Hassan AM, Abdelmegeed ES (2021) β-lactam resistance associated with β-lactamase production and porin alteration in clinical isolates of E. coli and K. pneumoniae. PLoS ONE 16(5):e0251594. https://doi.org/10.1371/journal.pone.0251594
Kim MK, Xuan D, Quintiliani R, Nightingale CH, Nicolau DP (2001) Pharmacokinetic and pharmacodynamic profile of high dose extended interval piperacillin-tazobactam. J Antimicrob Chemother 48(2):259–267. https://doi.org/10.1093/jac/48.2.259
Sher A, Niederer SA, Mirams GR, Kirpichnikova A, Allen R, Pathmanathan P, Gavaghan DJ, van der Graaf PH, Noble D (2022) A quantitative systems pharmacology perspective on the importance of parameter identifiability. Bull Math Biol 84(3):39. https://doi.org/10.1007/s11538-021-00982-5
Funding
The authors did not receive any funding for this work.
Author information
Authors and Affiliations
Contributions
ST, LA, and CH conceived the presented idea. ST and EL collected experimental results and explored different analytical angles. AL counseled the details of the strain’s resistance mechanism implementation on the model. CH supervised and evaluated the work. ST wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tandar, S.T., Aulin, L.B., Leemkuil, E.M.J. et al. Semi-mechanistic modeling of resistance development to β-lactam and β-lactamase-inhibitor combinations. J Pharmacokinet Pharmacodyn 51, 199–211 (2024). https://doi.org/10.1007/s10928-023-09895-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-023-09895-3