Abstract
Purpose
To evaluate the characteristics of patients with post-keratoplasty complications and their presentation at an emergency center.
Design
Retrospective one-armed cohort study.
Methods
Data were evaluated on patients who underwent corneal grafts in 2019 and presented to an emergency unit. Data were collected on patient demographics, presenting symptoms, clinical details, diagnosis at emergency visit, final diagnosis, best-corrected visual acuity (BCVA) at presentation and at the last follow-up after management. Severe visual impairment (SVI) and graft rejection were tested for correlations to other factors.
Results
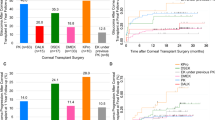
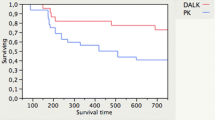
The study sample was comprised of 149 eyes of 124 patients with a mean age of 27.5 years. Keratoconus was the indication for keratoplasty in 94 (75.8%) patients. The main presenting symptoms were pain 57 (38.3%) and red eye in 52 (34.9%) patients. The median interval between emergency visit and keratoplasty was 1.6 years. There were 63 (42.3%) patients who had emergency visits due to suture-related problems. The rates of SVI and graft rejection at the time of discharge after managing emergencies in eyes with previous keratoplasty were 14.1% (95% CI 8.5; 19.7) and 13.4 (95% CI 7.9; 18.9), respectively. Keratoconus (OR = 22.8) and young age (P < 0.001) were negatively associated with SVI after management.
Conclusion
Patients with keratoplasty are at high risk for severe vision loss and should be counseled to seek urgent eye care for early detection and management of sight-threatening complications to improve graft survival and vision.


Similar content being viewed by others
References
Navarro Martínez-Cantullera A, Calatayud Pinuaga M (2016) Obtaining corneal tissue for keratoplasty. Arch Soc Esp Oftalmol 91:491–500
Armitage WJ, Goodchild C, Griffin MD et al (2019) High-risk Corneal Transplantation: Recent Developments and Future Possibilities. Transplantation 103:2468–2478. https://doi.org/10.1097/TP.0000000000002938
Singh R, Gupta N, Vanathi M, Tandon R (2019) Corneal transplantation in the modern era. Indian J Med Res 150:7–22
Tandon R, Singh A, Gupta N, Vanathi M, Gupta V (2017) Upgradation and modernization of eye banking services: Integrating tradition with innovative policies and current best practices. Indian J Ophthalmol 65:109–115
Ong HS, Ang M, Mehta JS (2021) Evolution of therapies for the corneal endothelium: past, present and future approaches. Br J Ophthalmol 105:454–467
Matthaei M, Sandhaeger H, Hermel M et al (2017) Changing Indications in Penetrating Keratoplasty: A Systematic Review of 34 Years of Global Reporting. Transplantation 101:1387–1399. https://doi.org/10.1097/TP.0000000000001281
Song Y, Zhang J, Pan Z (2020) Systematic Review and Meta-Analysis of Clinical Outcomes of Penetrating Keratoplasty Versus Deep Anterior Lamellar Keratoplasty for Keratoconus. Exp Clin Transplant 18:417–428. https://doi.org/10.6002/ect.2019.0123
Liu LY, Li X, Li W, Jiu X, Tian M (2021) Systematic review and meta-analysis of femtosecond laser–enabled keratoplasty versus conventional penetrating keratoplasty. Eur J Ophthalmol 31:976–987
Alio JL, Montesel A, El Sayyad F et al (2021) Corneal graft failure: an update. Br J Ophthalmol 105:1049–1058
Di Zazzo A, Kheirkhah A, Abud TB, Goyal S, Dana R (2017) Management of high-risk corneal transplantation. Surv Ophthalmol 62:816–827
Bamashmus MA, Al-Akily SA, AlAkhalee HA, Al-Nuseriy KO, Farhan MH (2017) Emergency visits after corneal transplantation in Yemen. Oman J Ophthalmol 10:193
Asfour WM, Shaban RI (2009) Post-keratoplasty emergency visits at a hospital in Jordan. Saudi Med J 30:1568–1571
Gnanaraj L, Sandhu S, Hildreth AJ, Figueiredo FC (2007) Postkeratoplasty emergency visits—a review of 100 consecutive visits. Eye 21:1028–1032
World Health Organization (2004) International statistical classification of diseases and related health problems: alphabetical index, vol 3. World Health Organization, Geneva
Alldredge OC, Krachmer JH (1981) Clinical types of corneal transplant rejection: their manifestations, frequency, preoperative correlates, and treatment. Arch Ophthal 99:599–604
Kamp MT, Fink NE, Enger C, Maguire MG, Stark WJ, Stulting RD (1995) Patient-reported symptoms associated with graft reactions in high-risk patients in the collaborative corneal transplantation studies. Collaborative Corneal Transplantation Studies Research Group. Cornea 14:43–48
Morris RJ, Kirkness CM (1988) Emergency presentation of corneal graft patients. Eye 2:71–76
Park CY, Lee JK, Gore PK, Lim CY, Chuck RS (2015) Keratoplasty in the United States: a 10-year review from 2005 through 2014. Ophthalmology 22:2432–2442
Tseng SH, Ling KC (1995) Late microbial keratitis after corneal transplantation. Cornea 14:591–594
Al-Hazzaa SA, Tabbara KF (1988) Bacterial keratitis after penetrating keratoplasty. Ophthalmology 95:1504–1508
Dohse N, Wibbelsman TD, Rapuano SB et al (2020) Microbial keratitis and clinical outcomes following penetrating and endothelial keratoplasty. Acta Ophthalmol 98:e895–e900
Sun JP, Chen WL, Huang JY, Hou YC, Wang IJ, Hu FR (2017) Microbial keratitis after penetrating keratoplasty. Am J Ophthalmol 178:150–156
Haddadin RI, Vora GK, Chodosh J (2013) Corneal trauma following keratoplasty. Int Ophthalmol Clin 53:23–32
Şingar Özdemir E, Burcu A, Yalnız Akkaya Z, Oral B, Örnek F (2018) Wound dehiscence after penetrating keratoplasty. Ulus Travma Acil Cerrahi Derg 24:563–568
Wang X, Liu T, Zhang S et al (2018) Outcomes of wound dehiscence after penetrating keratoplasty and lamellar keratoplasty. J Ophthalmol. https://doi.org/10.1155/2018/1435389
Goweida MB, Helaly HA, Ghaith AA (2015) Traumatic wound dehiscence after keratoplasty: characteristics, risk factors, and visual outcome. J Ophthalmol 2015:631409
Davila JR, Mian SI (2016) Infectious keratitis after keratoplasty. Curr Opin Ophthalmol 1(27):358–366
Fontana L, Moramarco A, Mandarà E, Russello G, Iovieno A (2019) Interface infectious keratitis after anterior and posterior lamellar keratoplasty. Clinical features and treatment strategies. A review Br J Ophthalmol 103:307–314
Porter AJ, Lee GA, Whitehead K (2017) Infectious crystalline keratopathy after Descemet’s stripping endothelial keratoplasty. BMJ Case Rep 2017:bcr-2017220464
Nahum Y, Russo C, Madi S, Busin M (2014) Interface infection after descemet stripping automated endothelial keratoplasty: outcomes of therapeutic keratoplasty. Cornea 1(33):893–898
Wagoner MD, Gonnah ES, AlTowerki AE (2010) Outcome of primary adult optical penetrating keratoplasty with imported donor corneas. Int Ophthalmol 30:127–136
Omar N, Chacra CT, Tabbara KF (2013) Outcome of corneal transplantation in a private institution in Saudi Arabia. Clin Ophthalmol 7:1311
Jeganathan SV, Ghosh S, Jhanji V, Lamoureux E, Taylor HR, Vajpayee RB (2008) Resuturing following penetrating keratoplasty: A retrospective analysis. Br J Ophthalmol 92:893–895
Acknowledgements
We would like to thank the research coordinator Mr. Faisal Al Hamidi for his invaluable help in this study.
Funding
This manuscript did not receive any funding.
Author information
Authors and Affiliations
Contributions
All authors participated in the interpretation of data, drafting or critical revision of the manuscript and approval of the final version of the manuscript and agreed with the decision to submit the manuscript for publication.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest was declared by the authors, and the authors declared that this study received no financial support. None of the authors reports other financial interests in terms of the presented study.
Ethical approval
The local ethics committee of the King Khaled Eye Specialist Hospital approved the protocol, and it adhered to the tenets of the Declaration of Helsinki. The nature of the study and its possible consequences were explained to study participants. All participants have given their written informed consent to participate in this study.
Informed consent
The study was registered with the institutional review board and clearance obtained from the ethics committee of the institution. Written consent from the patient(s) was also obtained. We hereby transfer, assign, or otherwise convey all copyright ownership, including any and all rights incidental thereto, exclusively to the journal, in the event that such work is published by the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Almudhaiyan, T., AlAmry, M., Khandekar, R. et al. Ocular emergencies visits after corneal transplantation at a tertiary eye care hospital in Saudi Arabia. Int Ophthalmol 42, 3897–3904 (2022). https://doi.org/10.1007/s10792-022-02410-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02410-6