Abstract
Purpose
To investigate the spherical shift of intraocular lens (IOL) tilt after intrascleral fixation.
Methods
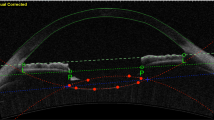
We retrospectively reviewed the medical records of patients who underwent flanged intrascleral IOL fixation with transconjunctival 25- or 27-gauge pars plana vitrectomy at the Department of Ophthalmology of the Jikei University Hospital. The minimum follow-up duration was 3 months. Second-generation anterior segment optical coherence tomography (CASIA2; TOMEY) was used to obtain the values of tilt and decentration of the intrasclerally fixated IOL and postoperative anterior chamber depth. We investigated the relationship between refractive error and various parameters, such as IOL tilt and decentration, axial length, and keratometry. In addition to our clinical investigation, we conducted optical simulations using Zemax to evaluate the spherical shift of the IOL tilt by means of the through-focus response and change in spherical equivalent power.
Results
The study involved 72 eyes of 67 patients. The degree of IOL tilt was correlated with the amount of refractive error (Spearman’s rank correlation coefficient [CC] = − 0.32; P = 0.006). In particular, a tilt angle greater than 10° strongly affected the refractive error. The postoperative anterior chamber depth also correlated with the refractive error (CC = 0.50; P < 0.001), as opposed to decentration (CC = − 0.17; P = 0.15), axial length (CC = − 0.08; P = 0.49), and keratometry (CC = − 0.06; P = 0.64). Optical simulations also revealed a myopic shift that exponentially increased as the tilt became greater.
Conclusion
IOL tilts that are greater than 10° induce refractive error.


Similar content being viewed by others
Data availability
Clinical data supporting the findings of this study are available within the article and its Supplementary Information.
References
Bellucci R, Pucci V, Morselli S, Bonomi L (1996) Secondary implantation of angle-supported anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg 22:247–252. https://doi.org/10.1016/s0886-3350(96)80227-6
Burkhard DH, Augustin AJ (2001) Lens implant selection with absence of capsular support. Curr Opin Ophthalmol 12:47–57. https://doi.org/10.1097/00055735-200102000-00009
Sawada T, Kimura W, Kimura T, Suga H, Ohte A, Yamanishi S, Ohara T (1998) Long-term follow-up of primary anterior chamber intraocular lens implantation. J Cataract Refract Surg 24:1515–1520. https://doi.org/10.1016/s0886-3350(98)80176-4
Ellingson FT (1978) The uveitis-glaucoma-hyphema syndrome associated with the Mark VIII anterior chamber lens implant. J Am Intraocul Implant Soc 4:50–53. https://doi.org/10.1016/s0146-2776(78)80054-8
De Silva SR, Arun K, Anandan M, Glover N, Patel CK, Rosen P (2011) Iris-claw intraocular lenses to correct aphakia in the absence of capsule support. J Cataract Refract Surg 37:1667–1672. https://doi.org/10.1016/j.jcrs.2011.03.051
Heilskov T, Joondeph BC, Olsen KR, Blankenship GW (1989) Late endophthalmitis after transscleral fixation of a posterior chamber intraocular lens. Arch Ophthalmol 107:1427. https://doi.org/10.1001/archopht.1989.01070020501017
Price MO, Price FW Jr, Werner L, Berlie C, Mamalis N (2005) Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg 31:1320–1326. https://doi.org/10.1016/j.jcrs.2004.12.060
Gabor SG, Pavlidis MM (2007) Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg 33:1851–1854. https://doi.org/10.1016/j.jcrs.2007.07.013
Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S (2008) Fibrine glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg 34:1433–1438. https://doi.org/10.1016/j.jcrs.2008.04.040
Ohta T, Toshida H, Murakami A (2014) Simplified and safe method of sutureless intrascleral posterior chamber intraocular lens fixation: Y-fixation technique. J Cataract Refract Surg 40:2–7. https://doi.org/10.1016/j.jcrs.2013.11.003
Yamane S, Inoue M, Arakawa A, Kadonosono K (2014) Sutureless 27-gauge needle-guided intrascleral intraocular lens implantation with lamellar scleral dissection. Ophthalmology 121:61–66. https://doi.org/10.1016/j.ophtha.2013.08.043
Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K (2017) Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology 124:1136–1142. https://doi.org/10.1016/j.ophtha.2017.03.036
Kurimori HY, Inoue M, Hirakata A (2018) Adjustments of haptics length for tilted intraocular lens after intrascleral fixation. Am J Ophthalmol Case Rep 10:180–184. https://doi.org/10.1016/j.ajoc.2018.02.025
Uozato H, Okada Y, Hirai Saishin M (1988) What are the tolerable limits of IOL tilt and decentration? Jpn Rev Clin Ophthalmol 82:2308–2311. https://doi.org/10.3390/vision4030041
Kemer Atik B, Altan C, Agca A, Kirmaci A, Yildirim Y, Genc S et al (2020) The effect of intraocular lens tilt on visual outcomes in scleral-fixated intraocular lens implantation. Int Ophthalmol 40:717–724. https://doi.org/10.1007/s10792-019-01233-2
Kimura S, Morizane Y, Shiode Y, Hirano M, Doi S, Toshima S et al (2017) Assessment of tilt and decentration of crystalline lens and intraocular lens relative to the corneal topographic axis using anterior segment optical coherence tomography. PLoS ONE 12:e0184066. https://doi.org/10.1371/journal.pone.0184066
Narang P, Agarwal A (2016) L-shaped scleral incision may be ideal for IOL explantation, insertion. Ocular Surgery News U.S. ed. Slack Inc.; Available at: https://www.healio.com/news/ophthalmology/20160112/lshaped-scleral-incision-may-be-ideal-for-iol-explantation-insertion [Accessed July 18, 2021]
Behrouz MJ, Kheirkhah A, Hashemian H, Nazari R (2010) Anterior segment parameters: comparison of 1-piece and 3-piece acrylic foldable intraocular lenses. J Cataract Refract Surg 36:1650–1655. https://doi.org/10.1016/j.jcrs.2010.05.013
Hayashi K, Hayashi H (2005) Comparison of the stability of 1-piece and 3-piece acrylic intraocular lenses in the lens capsule. J Cataract Refract Surg 31:337–342. https://doi.org/10.1016/j.jcrs.2004.06.042
Liou H-L, Brennan NA (1997) Anatomically accurate, finite model eye for optical modeling. J Opt Soc Am A 14:1684–1695. https://doi.org/10.1364/josaa.14.001684
Norrby S, Piers P, Campbell C, van der Mooren M (1998) Determining the imaging quality of intraocular lenses. J Cataract Refract Surg 24:703–714. https://doi.org/10.1016/s0886-3350(98)80270-8
Campbell FW, Green DG (1965) Optical and retinal factors affecting visual resolution. J Physiol 181:576–593. https://doi.org/10.1113/jphysiol.1965.sp007784
Phillips P, Pérez-Emmanuelli J, Rosskothen HD, Koester CJ (1988) Measurement of intraocular lens decentration and tilt in vivo. J Cataract Refract Surg 14:129–135. https://doi.org/10.1016/s0886-3350(88)80086-5
Sasaki K, Sakamoto Y, Shibata T, Nakaizumi H, Emori Y (1989) Measurement of postoperative intraocular lens tilting and decentration using Scheimpflug images. J Cataract Refractive Surg 15:454–457. https://doi.org/10.1016/s0886-3350(89)80071-9
Loya N, Lichter H, Barash D, Goldenberg-Cohen N, Strassmann E, Weinberger D (2001) Posterior chamber intra-ocular lens implantation after capsular tear: ultrasound bio-microscopy evaluation. J Cataract Refract Surg 27:1423–1427. https://doi.org/10.1016/s0886-3350(01)00786-6
Kumar DA, Agarwal A, Prakash G, Jacob S, Saravanan Y, Agarwal A (2011) Evaluation of intraocular lens tilt with anterior segment optical coherence tomography. Am J Ophthalmol 151:406–412. https://doi.org/10.1016/j.ajo.2010.09.013
Ding X, Wang Q, Chang P, Li J, Savini G, Huang J et al (2015) The repeatability assessment of three dimensional capsule-intraocular lens complex measurements by means of high-speed sweptsource optical coherence tomography. PLoS ONE 10:e0142556. https://doi.org/10.1371/journal.pone.0142556
Okamoto S, Kimura K, Funakura M, Ikeda N, Hiramatsu H, Bains HS (2011) Comparison of wavefront-guided aspheric laser in situ keratomileusis for myopia: coaxially sighted corneal-light-reflex versus line-of-sight centration. J Cataract Refract Surg 37:1951–1960. https://doi.org/10.1016/j.jcrs.2011.05.040
Kumar DA, Agarwal A, Agarwal A, Chandrasekar R, Priyanka V (2015) Long-term assessment of tilt of glued intraocular lenses: an optical coherence tomography analysis 5 years after. Ophthalmology 122:48–55. https://doi.org/10.1016/j.ophtha.2014.07.032
Jujo T, Kogo J, Sasaki H, Sekine R, Sato K, Ebisutani S, Toyoda Y et al (2021) 27-gauge trocar-assisted sutureless intraocular lens fixation. BMC Ophthalmol 21:8. https://doi.org/10.1186/s12886-020-01758-6
Dubey R, Birchall W, Grigg J (2012) Improved refractive outcome for ciliary sulcus-implanted intraocular lenses. Ophthalmology 119:261–265. https://doi.org/10.1016/j.ophtha.2011.07.050
Lakshminarayanan V, Enoch JM, Raasch T, Crawford B, Nygaard RW (1986) Refractive changes induced by intraocular lens tilt and longitudinal displacement. Arch Ophthalmol 104:90–92. https://doi.org/10.1001/archopht.1986.01050130100030
Erickson P (1990) Effects of intraocular lens position errors on postoperative refractive error. J Cataract Refract Surg 16:305–311. https://doi.org/10.1016/s0886-3350(13)80699-2
Melles RB, Holladay JT, Chang WJ (2018) Accuracy of intraocular lens calculation formulas. Ophthalmology 125:169–178. https://doi.org/10.1016/j.ophtha.2017.08.027
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
The authors thank Tjundewo Lawu for conducting optical simulation using ZEMAX.
Corresponding author
Ethics declarations
Conflict of interest
Financial interests: Author T. Nakano has received Grant from CREWT Medical Systems, Kyowa Medical, Kuribara Medical Instruments, Kowa, Tomey, Otsuka Pharmaceutical, Senju Pharmaceutical, MSD, Pfizer, Alcon Japan, Santen Pharmaceutical, NIDEK, AMO Japan Bayer, and IOL MEDICAL. Author T. Nakano has also received Personal Fees from Kowa, Otsuka Pharmaceutical, Senju Pharmaceutical, Santen Pharmaceutical, Nitto Medical, and Nikon.
Ethical approval
This study was conducted with approval from the institutional review board and in accordance with the ethical standards of the Helsinki Declaration of 1975, as revised in 2000 and 2008.The study protocol was approved by the Institutional Review Board of the Jikei University School of Medicine (approval no.:31–421[10003]), and all clinical procedures were conducted according to the principles of the Declaration of Helsinki.
Consent for participation
The study protocol was disclosed, and patients were given the opportunity to refuse participation in the study.
Consent to publishing
The study protocol was disclosed, and patients were given the opportunity to refuse participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tokuhisa, T., Watanabe, T., Watanabe, A. et al. Refractive error induced by intraocular lens tilt after intrascleral intraocular lens fixation. Int Ophthalmol 42, 1213–1220 (2022). https://doi.org/10.1007/s10792-021-02106-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-02106-3