Abstract
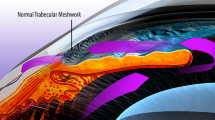
Medical management remains the cornerstone of glaucoma management despite advances in the surgical or laser procedures. After a leap of almost two decades of the advent of prostaglandin analogues, recently a new class of drug, Rho kinase (ROCK) inhibitors, has come to limelight because of their varied therapeutic potential in different clinical conditions of eye, especially glaucoma. Their efficacy of lowering intraocular pressure (IOP) by virtue of an entirely different mechanism of decreasing outflow resistance has ignited a series of clinical trials evaluating their potential as monotherapy or as adjunct to existing antiglaucoma medications, and three of them ripasudil, netarsudil and roclatan have even been approved for clinical use in the recent past. There are evidences suggesting their beneficial effects in glaucoma patients even via non-IOP-dependent mechanisms like neuroprotection by improving blood flow to the optic nerve and increasing ganglion cell survival. They can even act as antifibrotic agents and reduce bleb scarring after glaucoma surgery. Hence, their effective role in glaucomatous optic neuropathy is multifaceted primary being improved drainage through the conventional pathway. On the other hand, certain local adverse effects like conjunctival hyperaemia have been reported in substantial proportion of patients, while some others like blepharitis, subconjunctival haemorrhages and cornea verticillata constitute less common side effects. The purpose of this review is to summarize the discovery, evolution and recent update of clinical trials on Rho kinase inhibitors as antiglaucoma medicine and to delineate their role in existing management protocol.



Similar content being viewed by others
References
Varma R, Lee PP, Goldberg I, Kotak S (2011) An assessment of the health and economic burdens of glaucoma. Am J Ophthalmol 152:515–522
Tham Y-C, Li X, Wong TY et al (2014) Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 121:2081–2090
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M (2002) Early manifest glaucoma trial group. reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol 120:1268–1279
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, Parrish RK 2nd, Wilson MR et al (2002) The ocular hypertension treatment study: Baseline factors that predict the onset of primary open angle glaucoma. Arch Ophthalmol 120(6):714–720
Nau CB, Malihi M, McLaren JW (2013) Hodge DO, Sit AJ: Circadian variation of aqueous humor dynamics in older healthy adults. Invest Ophthalmol Vis Sci 54:7623–7629
Johnson M (2006) What controls aqueous humour outflow resistance? Exp Eye Res. 82:545–557
Gabelt BT, Kaufman PL (2005) Changes in aqueous humor dynamics with age and glaucoma. Prog Retin Eye Res 24:612–37
Keller KE, Aga M, Bradley JM et al (2009) Extracellular matrix turnover and outflow resistance. Exp Eye Res 88:676–682
Tripathi RC, Li J, Chan WF, Tripathi BJ (1994) Aqueous humor in glaucomatous eyes contains an increased level of TGF-beta 2. Exp Eye Res 59:723–727
Tezel G, Kass MA, Kolker AE, Becker B, Wax MB (1997) Plasma and aqueous humour endothelin levels in primary open-angle glaucoma. J Glaucoma 6:83–89
Stamer WD, Acott TS (2012) Current understanding of conventional outflow dysfunction in glaucoma. CurrOpinOphthalmol 23:135–143
Kaufman PL, Barany EH (1976) Loss of acute pilocarpine effect on outflow facility following surgical disinsertion and retrodisplacement of the ciliary muscle from the scleral spur in the cynomolgus monkey. Invest Ophthalmol 15:793–797
Tanna AP, Rademaker AW, Stewart WC, Feldman RM (2010) Meta-analysis of the efficacy and safety of alpha2-adrenergic agonists, beta-adrenergic antagonists, and topical carbonic anhydrase inhibitors with prostaglandin analogs. Arch Ophthalmol 128:825–833
Lichter PR, Musch DC, Gillespie BW et al (2001) Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology 108:1943–1953
Kass MA, Heuer DK, Higginbotham EJ, et al. 2002 The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 120: 701e713. discussion 829–830.
Gedde SJ, Herndon LW, Brandt JD, Budenz DL, Feuer WJ, Schiffman JC; 2012 Tube Versus Trabeculectomy Study Group. Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol. 153 (5): 804–814.e1.
Kopczynski CC, Epstein DL (2014) Emerging trabecular outflow drugs. J Ocul Pharmacol Ther 30:85–87
Tian B, Geiger B, Epstein DL, Kaufman PL (2000) Cytoskeletal involvement in the regulation of aqueous humor outflow. Invest Ophthalmol Vis Sci 41:619–623
.Peterson J.A. Tian B., Geiger B., Kaufman P.L. (2000) Effect of latrunculin-B on outflow facility in monkeys. Exp Eye Res 70:307–313
Tian B, Kaufman P (1998) Volberg T, Gabelt B’ Ann T, Geiger B: H-7 disrupts the actin cytoskeleton and increases outflow facility. Arch Ophthalmol 116:633–643
Amano M, Nakayama M, Kaibuchi K (2010) Rho-kinase/ROCK: a key regulator of the cytoskeleton and cell polarity. Cytoskeleton (Hoboken) 67:545–554
Wang SK, Chang RT (2014) An emerging treatment option for glaucoma: rho kinase inhibitors. Clin Ophthalmol 8:883–890
Wang J, Liu X, Zhong Y (2013) Rho/Rho-associated kinase pathway in glaucoma (Review). Int J Oncol 43:1357–1367
Uehata M, Ishizaki T, Satoh H, Ono T, Kawahara T, Morishita T, Tamakawa H, Yamagami K, Inui J, Maekawa M et al (1997) Calcium sensitization of smooth muscle mediated by a Rho-associated protein kinase in hypertension. Nature 389(6654):990–994
Mizuno Y, Isotani E, Huang J, Ding H, Stull JT, Kamm KE (2008) Myosin light chain kinase activation and calcium sensitization in smooth muscle in vivo. Am J Physiol Cell Physiol 295(2):C358–C364
Huang TY, DerMardirossian C, Bokoch GM (2006) Cofilin phosphatases and regulation of actin dynamics. Curr Opin Cell Biol 18:26–31
McCullough BR, Blanchoin L, Martiel J-L, De La Cruz EM (2008) Cofilin increases the bending flexibility of actin filaments: implications for severing and cell mechanics. J Mol Biol 381:550–558
Loirand G (2015) Rho kinases in health and disease: from basic science to translational research. Pharmacol Rev 67:1074–1095
Johnson M, Shapiro A, Ethier CR, Kamm RD (1992) Modulation of outflow resistance by the pores of the inner wall endothelium. Invest Ophthalmol Vis Sci 33:1670–1675
Svedbergh B, Lutjen-Drecoll E, Ober M, Kaufman PL (1978) Cytochalasin B-induced structural changes in the anterior ocular segment of the cynomolgus monkey. Invest Ophthalmol Vis Sci 17:718–734
Tanihara H, Kakuda T, Sano T, Kanno T, Gunji R (2020) Safety and efficacy of ripasudil in Japanese patients with glaucoma or ocular hypertension: 12-month interim analysis of ROCK-J, a post-marketing surveillance study. BMC Ophthalmol 20(1):275. https://doi.org/10.1186/s12886-020-01490-1
Zhou Q, Gensch C, Liao JK (2011) Rho-associated coiled-coil-forming kinases (ROCKs): potential targets for the treatment of atherosclerosis and vascular disease. Trends Pharmacol Sci 32:167–173
Yamamoto K, Maruyama K, Himori N, Omodaka K, Yokoyama Y, Shiga Y, Morin R, Nakazawa T (2014) The novel Rho kinase (ROCK) inhibitor K-115: a new candidate drug for neuroprotective treatment in glaucoma. Invest Ophthalmol Vis Sci 55(11):7126–7136
Sturdivant JM, Royalty SM, Lin CW, Moore LA, Yingling JD, Laethem CL, Sherman B, Heintzelman GR, Kopczynski CC, deLong MA (2016) Discovery of the ROCK inhibitor netarsudil for the treatment of open-angle glaucoma. Bioorg Med Chem Lett 26(10):2475–2480
Riento K, Ridley AJ (2003) Rocks: multifunctional kinases in cell behaviour. Nat Rev Mol Cell Biol 4:446–456
Watabe H, Abe S, Yoshitomi T (2011) Effects of Rho-associated protein kinase inhibitors Y-27632 and Y-39983 on isolated rabbit ciliary arteries. Jpn J Ophthalmol 55:411–417
Galassi F, Giambene B, Varriale R (2011) Systemic vascular dysregulation and retrobulbar hemodynamics in normal-tension glaucoma. Invest Ophthalmol Vis Sci 52:4467–4471
Delaney Y, Walshe TE, O”Brien C. (2006) Vasospasm in glaucoma: Clinical and laboratory aspects. Optom Vis Sci 83(7):406–414
Hein TW, Rosa RH Jr, Yuan Z, Roberts E, Kuo L (2010) Divergent roles of nitric oxide and rho kinase in vasomotor regulation of human retinal arterioles. Invest Ophthalmol Vis Sci 51(3):1583–1590
Sugimaya T, Shibata M, Kajiura S, Okuno T, Tonari M, Oku H, Ikeda T (2011) Effects of fasudil, a Rho-associated protein kinase inhibitor, on optic nerve head blood flow in rabbits. Invest Ophthalmol Vis Sci 52:64–69
Ohta Y, Takaseki S, Yoshitomi T (2017) Effects of ripasudil hydrochloride hydrate (K-115), a Rho-kinase inhibitor, on ocular blood flow and ciliary artery smooth muscle contraction in rabbits. Jpn J Ophthalmol 61:423–432
Goldhagen B, Proia AD, Epstein DL, Rao PV (2012) Elevated levels of Rho A in the optic nerve head of human eyes with glaucoma. J Glaucoma 21:530–538
Van de Velde S, De Groef L, Stalmans I, Moons L, Van Hove I (2015) Towards axonal regeneration and neuroprotection in glaucoma: rho kinase inhibitors as promising therapeutics. Prog Neurobiol 131:105–119
Kitaoka Y, Kitaoka Y, Kumai T, Lam TT, Kuribayashi K, Isenoumi K, Munemasa Y, Motoki M, Kobayashi S, Ueno S (2004) Involvement of RhoA and possible neuroprotective effect of fasudil, a Rho kinase inhibitor, in NMDA-induced neurotoxicity in the rat retina. Brain Res 1018:111–118
Bertrand J, Winton MJ, Rodriguez-Hernandez N, Campenot RB, McKerracher L (2005) Application of Rho antagonist to neuronal cell bodies promotes neurite growth in compartmented cultures and regeneration of retinal ganglion cell axons in the optic nerve of adult rats. J Neurosci 2(5):1113–21
Wu X, Walker CL, Lu Q, Wu W, Eddelman DB, Parish JM, Xu XM (2017) RhoA/Rho kinase mediates neuronal death through regulating cPLA2 activation. Mol Neurobiol 54(9):6885–6895
Bösel J, Gandor F, Harms C, Synowitz M, Harms U, Djoufack PC, Megow D, Dirnagl U, Hörtnagl H, Fink KB, Endres M (2005) Neuroprotective effects of atorvastatin against glutamate-induced excitotoxicity in primary cortical neurones. J Neurochem 92(6):1386–1398
Sagawa H, Terasaki H, Nakamura M, Ichikawa M, Yata T, Tokita Y, Watanabe M (2007) A novel ROCK inhibitor, Y-39983, promotes regeneration of crushed axons of retinal ganglion cells into the optic nerve of adult cats. Exp Neurol 205(1):230–240
Shaw PX, Sang A, Wang Y, Ho D, Douglas C, Dia L, Goldberg JL (2017) Topical administration of a Rock/Net inhibitor promotes retinal ganglion cell survival and axon regeneration after optic nerve injury. Exp Eye Res 158:33–42
Okumura N, Okazaki Y, Inoue R, Kakutani K, Nakano S, Kinoshita S, Koizumi N (2016) Effect of the Rho-Associated Kinase Inhibitor Eye Drop (Ripasudil) on Corneal Endothelial Wound Healing. Invest Ophthalmol Vis Sci 57(3):1284–1292
Okumura N, Koizumi N, Kay EP, Ueno M, Sakamoto Y, Nakamura S, Hamuro J, Kinoshita S (2013) The ROCK inhibitor eye drop accelerates corneal endothelium wound healing. Invest Ophthalmol Vis Sci 54(4):2493–2502
Okumura N, Kinoshita S, Koizumi N (2017) Application of Rho kinase inhibitors for the treatment of corneal endothelial diseases. J Ophthalmol 2017:2646904. https://doi.org/10.1155/2017/2646904pmid:28751979
Nakagawa H, Koizumi N, Okumura N, Suganami H, Kinoshita S (2015) Morphological changes of human corneal endothelial cells after rho-associated kinase inhibitor eye drop (Ripasudil) administration: a prospective open-label clinical study. PLoS ONE 10(9):e0136802. https://doi.org/10.1371/journal.pone.0136802pmid:26367375
Honjo M, Tanihara H, Kameda T, Kawaji T, Yoshimura N, Araie M (2007) Potential role of Rho-associated protein kinase inhibitor Y-27632 in glaucoma filtration surgery. Invest Ophthalmol Vis Sci 48(12):5549–5557
Cordeiro MF, Reichel MB, Gay JA, D’Esposita F, Alexander RA, Khaw PT (1999) Transforming growth factor-beta1, -beta2, and -beta3 in vivo: effects on normal and mitomycin C-modulated conjunctival scarring. Invest Ophthalmol Vis Sci 40(9):1975–1982
Futakuchi A, Inoue T, Fujimoto T, Inoue-Mochita M, Kawai M, Tanihara H (2016) The effects of ripasudil (K-115), a Rho kinase inhibitor, on activation of human conjunctival fibroblasts. Exp Eye Res 149:107–115
Meyer-ter-Vehn T, Sieprath S, Katzenberger B, Gebhardt S, Grehn F, Schlunck G (2006) Contractility as a prerequisite for TGF-beta-induced myofibroblast transdifferentiation in human tenon fibroblasts. Invest Ophthalmol Vis Sci 47(11):4895–4904
Van de Velde S, Van Bergen T, Vandewalle E, Kindt N, Castermans K, Moons L, Stalmans I (2015) Rho kinase inhibitor AMA0526 improves surgical outcome in a rabbit model of glaucoma filtration surgery. Prog Brain Res 220:283–297
Garnock-Jones KP (2014) Ripasudil: first global approval. Drugs 74:2211–2215
Lan Ma, Ruo-Lan 2019 Qian and undefined Meta-analysis of Rho kinase inhibitor Ripasudil in the treatment of glaucoma. Guoji Yanke Zazhi. 19 (10): 1717–1721.
Tanna AP, Johnson M (2018) Rho kinase inhibitors as a novel treatment for glaucoma and ocular hypertension. Ophthalmology 125(11):1741–1756
Moshirfar M, Parker L, Birdsong OC, Ronquillo YC, Hofstedt D, Shah TJ, Gomez AT, Hoopes PC (2018) SrMedical Hypothesis. Discovery & Innovation in Ophthalmology 7(3):101–111
Inoue T, Tanihara H, Tokushige H, Araie M (2015) Efficacy and safety of SNJ-1656 in primary open-angle glaucoma or ocular hypertension. Acta Ophthalmol 93:e393–e395
Kopczynski C, Novack GD, Swearingen D, van Haarlem T (2013) Ocular hypotensive efficacy, safety and systemic absorption of AR-12286 ophthalmic solution in normal volunteers. Br J Ophthalmol 97:567–572
Williams RD, Novack GD, van Haarlem T, Kopczynski C; 2011 AR-12286 Phase 2A Study Group. Ocular hypotensive effect of the Rho kinase inhibitor AR-12286 in patients with glaucoma and ocular hypertension. Am J Ophthalmol. 152(5): 834–41.e1.
Kaneko Y, Ohta M, Inoue T, Mizuno K, Isobe T, Tanabe S, Tanihara H (2016) Effects of K-115 (Ripasudil), a novel ROCK inhibitor, on trabecular meshwork and Schlemm’s canal endothelial cells. Sci Rep 19(6):19640
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Araie M 2013 K-115 Clinical Study Group. Phase 1 clinical trials of a selective Rho kinase inhibitor, K-115. JAMA Ophthalmol. 131(10): 1288–95.
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Araie M; K-115 2013 Clinical Study Group. Phase 2 randomized clinical study of a Rho kinase inhibitor, K-115, in primary open-angle glaucoma and ocular hypertension. Am J Ophthalmol. 156(4): 731–6.
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Fukushima A, Suganami H, Araie M 2016 K-115 Clinical Study Group. One-year clinical evaluation of 0.4% ripasudil (K-115) in patients with open-angle glaucoma and ocular hypertension. Acta Ophthalmol. 94(1): e26–34
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Suganami H, Araie M; K-115 Clinical Study Group. Additive Intraocular Pressure-Lowering Effects of the Rho Kinase Inhibitor Ripasudil (K-115) Combined With Timolol or Latanoprost: A Report of 2 Randomized Clinical Trials. JAMA Ophthalmol. 2015 Jul;133(7):755–61.
Inazaki H, Kobayashi S, Anzai Y, Satoh H, Sato S, Inoue M, Yamane S, Kadonosono K (2017) Efficacy of the additional use of ripasudil, a rho-kinase inhibitor, in patients with glaucoma inadequately controlled under maximum medical therapy. J Glaucoma 26(2):96–100
Inoue K, Okayama R, Shiokawa M, Ishida K, Tomita G (2018) Efficacy and safety of adding ripasudil to existing treatment regimens for reducing intraocular pressure. Int Ophthalmol 38(1):93–98
Sato S, Hirooka K, Nitta E, Ukegawa K, Tsujikawa A (2016) Additive intraocular pressure lowering effects of the rho kinase inhibitor, ripasudil in glaucoma patients not able to obtain adequate control after other maximal tolerated medical therapy. Adv Ther 33(9):1628–1634
Terao E., Nakakura S., Fujisawa Y., Fujio Y, Matsuya K, Kobayashi Y, Tabuchi H, Yoneda,T, Fukushima A ,Kiuchi Y,et. al. 2017 Time course of conjunctival hyperemia induced by a Rho-kinase inhibitor anti-glaucoma eye drop: ripasudil 0.4.%,Curr Eye Res 42:5 738–742.
Bacharach J, Dubiner HB, Levy B,, Kopczynski CC, Novack GD 2015 AR-13324-CS202 Study Group.Double-masked, randomized, dose-response study of AR-13324 versus latanoprost in patients with elevated intraocular pressure. Ophthalmology 122:302–7.
Serle JB, Katz LJ, McLaurin E, Heah T, Ramirez-Davis N, Usner DW, Novack GD, Kopczynski CC (2018) ROCKET-1 and ROCKET-2 study groups. two phase 3 clinical trials comparing the safety and efficacy of netarsudil to timolol in patients with elevated intraocular pressure: rho kinase elevated iop treatment trial 1 and 2 (ROCKET-1 and ROCKET-2). Am J Ophthalmol. 186:116–127
Lewis RA, Levy B, Ramirez N, Kopczynski CC, Usner DW, Novack GD (2016) Fixed-dose combination of AR-13324 and latanoprost: a double-masked, 28-day, randomised, controlled study in patients with open-angle glaucoma or ocular hypertension. Br J Ophthalmol 100(3):339–344
Aerie Pharmaceuticals I. Aerie Pharmaceuticals Roclatan™ Mercury Phase 3 Topline Efficacy Results Conference Call. 2017
Van de Velde S, Van Bergen T, Sijnave D, Hollanders K, Castermans K, Defert O, Leysen D, Vandewalle E, Moons L, Stalmans I (2014) AMA0076, a novel, locally acting Rho kinase inhibitor, potently lowers intraocular pressure in New Zealand white rabbits with minimal hyperemia. Invest Ophthalmol Vis Sci 55(2):1006–1016
Tanihara H, Inatani M, Honjo M, Tokushige H, Azuma J, Araie M (2008) Intraocular pressure lowering effects and safety of topical administration of a selective ROCK inhibitor, SNJ-1656, in healthy volunteers. Arch Ophthalmol 126:309–315
Arnold JJ, Hansen MS, Gorman GS, Inoue T, Rao V, Spellen S, Hunsinger RN, Chapleau CA, Pozzo-Miller L, Stamer WD et al (2013) The effect of Rho-associated kinase inhibition on the ocular penetration of timolol maleate. Invest Ophthalmol Vis Sci 54(2):1118–1126
Abbasgholizadeh R, Zhang H, Craft JW Jr, Bryan RM Jr, Bark SJ, Briggs JM, Fox RO, Agarkov A, Zimmer WE, Gilbertson SR, Schwartz RJ (2019) Feature article: discovery of vascular Rho kinase (ROCK) inhibitory peptides. Exp Biol Med (Maywood) 244(11):940–951
Hall J, Sall KN, Peace JH et al (2014) Initial clinical evaluation of safety, tolerability and pharmacodynamics of the locally-acting ROCK inhibitor AMA0076. Investig Opthalmol Vis Sci 55:565
Funding
There is neither any source of support nor any conflict of interest of any kind associated with the same.
Author information
Authors and Affiliations
Contributions
All authors contributed equally in this work. All authors have read and approved the final manuscript and given their consent for publication of the article.
Corresponding author
Ethics declarations
Conflict of interest
We (Authors) declare that the manuscript has been read and approved by all of us, and the requirements for authorship as stated in this document have been met with no conflict of interest. We all believe that the manuscript represents honest work
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent of publication
We hereby solemnly declare and confirm that this research article is original and has neither been published nor been sent or publication in any other journal.
Human and animal rights
All applicable international, national and/or institutional guidelines for the care and use of animals were followed. This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Place of study: Regional institute of ophthalmology (RIO), Indira Gandhi Institute of Medical Sciences (IGIMS, Patna).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Saha, B.C., Kumari, R., Kushumesh, R. et al. Status of Rho kinase inhibitors in glaucoma therapeutics—an overview. Int Ophthalmol 42, 281–294 (2022). https://doi.org/10.1007/s10792-021-02002-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-02002-w